Fig. 12.1
A fear/trauma network is composed of mutually excitatory connections. It results from multiple fearful experiences: the representation of a single event may well connect to the particular context, the “when” and “where” it happened. If, however, an additional stressful experience cues an already existing network of traumatic hot memories, the connection to the cold memory is lost, while sensory, cognitive, emotional, and physiological representations interconnect with increasingly mutual excitatory power. Cold, contextual memories, that is, codes of the “where” and “when,” however, are not consistently co-activated as the brain’s architecture does not support the simultaneous activation of two different places (coded by “place cells” in the hippocampus) (Elbert et al. 2006). Thus the fear/trauma network becomes disconnected (symbolized by the scissors) from time and place, and the fear generalizes, giving rise to feelings of impending threat. Narrative Exposure Therapy is thought to reverse this process by reconnecting hot and cold memories while segregating the memory traces of the different events (Figure modified from Schauer and Elbert 2010)
Since the activation of the trauma network serves as a frightening and painful recollection, many PTSD patients learn to avoid cues that act as reminders of the traumatic event. They attempt not to think or talk about any part represented in the trauma network and to stay away from persons and places that remind them of the frightening event. In contrast to their prominent hot trauma memories, survivors who suffer from PTSD have difficulties with autobiographical cold context; that is, they are unable to orient the fear associated with the events appropriately in time and space or to clearly structure these traumatic events in chronological order (Schauer et al. 2011). Such challenges, in conjunction with the avoidance of activating the trauma structure, make it difficult for PTSD patients to narrate their traumatic experiences (Neuner et al. 2008a). It is likely that these mechanisms of traumatic memories are not restricted to PTSD. Individuals suffering from other anxiety disorders, depression, or eating disorders frequently also report repeated vivid intrusive recollections abounding in highly distressful content but lacking cold memory contextual elements (Brewin et al. 2010).
Note that the network connects to response dispositions (= emotions), which can be either an alarm response involving fight and flight or a dissociative response (up to the extent of fainting, i.e., playing dead; Schauer and Elbert 2010). Thus, dissociative amnesia or “shutdown” can occur, replacing intrusions and hyperarousal with dissociation and passive avoidance. Both response types are evolutionarily prepared, and a patient may show either one, depending on the cues that activate the related memory. Narrative Exposure Therapy is thought to reverse these detrimental conditions by strengthening connections to the context.
We conclude that repeated exposure to traumatic events results in the distortion of not merely the content of events but also the overarching organization and structure of both memory storage and retrieval; the more seriously threatening or damaging the survived experiences, the greater degree the disorganization.
12.1.2 The Building Block Effect of Traumatic Load for Trauma-Related Mental Illness
With cumulative adversities and stressors, the trauma network becomes enlarged, ultimately leading to forms of trauma-related suffering (Fig. 12.1): survivors are unable to contextualize cues, and thus the past becomes the present. The writer and Holocaust survivor Primo Levo describes such experiences in his work The Truce: “…I am sitting… in a peaceful relaxed environment, apparently without tension or affliction; yet I feel a deep and subtle anguish, the definite sensation of an impending threat. And in fact ..slowly and brutally.. everything collapses, and disintegrates around me, the scenery, the walls, the people, while the anguish becomes more intense and more precise. I am alone in the centre of a grey and turbid nothing, and I know what this thing means, and I also know that I have always known it: I am in the Lager (death camp).., and nothing is true outside the Lager. All the rest was a brief pause, a deception of the senses, a dream.”
All symptoms of traumatic stress (PTSD) and depression have repeatedly been shown to correlate in their severity with the cumulative exposure to traumatic stress (Mollica et al. 1998; Neuner et al. 2004a; Kolassa and Elbert 2007; Kolassa et al. 2015, Chap. 4). More recently it has become obvious that childhood adversity is the other major dimension in predicting trauma-related mental illness (Catani et al. 2009b,c, 2010; Neuner et al. 2006; Nandi et al. 2014).
12.2 The Rationale and Logic of NET
Given the structure of traumatic memory representations, the goal of an etiologically oriented trauma therapy must be to reconnect hot and cold memory, focusing on the most arousing experiences. Therefore, in NET, the client, with the assistance of the therapist, constructs a chronological narrative of her/his life story with a focus on the traumatic experiences. Within a predefined number, usually about 4–12, of 90 min sessions, the fragmented reports of the traumatic experiences will be transformed into a coherent narrative. Empathic understanding, active listening, congruency, and unconditional positive regard are key components of the therapist’s behavior and attitude. For traumatic stress experiences the therapist explores sensory information, resulting cognitions, affective and physiological responding in detail and probes for respective observations. The patient is encouraged to relive these experiences while narrating, without losing the connection to the “here and now.” Using permanent reminders that the feelings and physiological responses result from activation of (hot) memories, the therapist links these mnemonic representations to episodic facts, that is, time and place (cold memory). The imagined exposure to the traumatic past is not terminated until the related affection, especially the fear presented by the patient, demonstrably decreases. In this way, the therapist is supportive yet directive in eliciting the narrative in order to recover the implicit information of the trauma in its entirety. For survivors of domestic or organized violence, the testimony can be recorded and used for documentary purposes.
After an assessment of the individual’s mental health status, a psychoeducational introduction is presented to the survivor, focusing on the explanation of his or her disturbance and symptoms, and, if appropriate a statement about the universality of human rights, followed by an outline of the treatment rationale tuned to the cognitive capacity of the survivor (age, formal education, etc.).
Narrative Exposure Therapy then starts with a biographical overview of the life span. Figure 12.2 schematically indicates the goal of the therapist: to determine arousal peaks across the life span. Lifetime periods and important biographical events of the survivor are symbolized in a ritual called the lifeline. The lifeline exercise consists of placing positive and negative life events, symbolized by flowers and stones, along a “line” (e.g., rope) in chronological order. With the guidance of the therapist, the patient places the symbols next to the line while classifying them only briefly – just a label will do. The purpose of the lifeline is the reconstruction of subjectively significant life events in their chronological order. An initial, cursory overview of the times and locations in which events occurred within the overarching context of the individual’s life, it serves as introduction to the logic of the therapeutic process. The therapist asks questions concerning the “when” and “where” an event took place, that is, focuses on cold memory and moves on before hot memory contents become strongly activated. The therapist attends to the body language of the patient. When the patient shows any signs of emotional arousal or begins to recall pictures or other sensations, the therapist reminds the patient that a detailed processing and narration of the event will be constructed later, beginning in the next session. The lifeline exercise should be concluded within one session. Otherwise an avoidance conspiracy between client and therapist may delay the essential healing agent, that is, the imagined exposure of the traumatic experience.
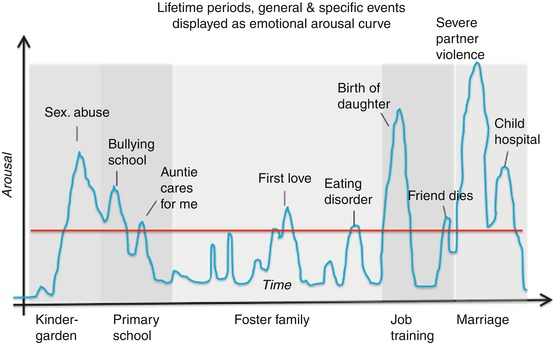
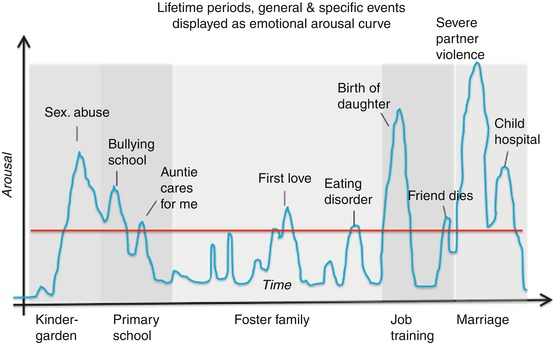
Fig. 12.2
Emotional arousal varies greatly across the life span. The lifeline exercise marks the arousal peaks above a threshold with a symbol, negative valence with a stone and positive valence with a flower, and assigns them to a place (e.g., “hometown”) and a time, ideally a specific event (like “the night before my 12th birthday”) or at least a general event (“when my uncle visited us”). A life period (when I went to school, college; when I was working in New York) can always be assigned (for more details, see Schauer et al. 2011; Schauer and Ruf-Leuschner 2014)
In the next session, the narration starts with essential background information and then the earliest arousing events in life and continues sequentially over time. A pre-trauma period may be used as the time during which a foundation for the therapeutic core process is laid and a good rapport between therapist and patient is established. In this phase, for example, the telling of emotional, warm, or exciting moments in the patient’s early life offers themselves as a training ground for emotional processing and communication between the patient and therapist.
During the narrative procedure, the survivor continues recounting his/her life story in chronological order. Wherever a “stone” (traumatic incident) occurs, the event is relived in a moment-by-moment reprocessing of the sensory, cognitive, emotional, and bodily details of the traumatic scenes, ensuring the interweaving of hot and cold memory elements, meaning-making, and integration. During the telling of the events, the therapist structures the topics and helps to clarify ambiguous descriptions. The therapist assumes an empathic and accepting role. Inconsistencies in the patient’s report are gently pointed out and often resolved by raising in-depth awareness about recurring bodily sensations or thoughts. The patient is encouraged to describe the traumatic events with sensory details and to reveal the perceptions, cognitions, and emotions that had been experienced at that time. During or after the session, the therapist either writes down a version of the patient’s narration or drafts brief notes next to the lifeline that has been sketched or photographed.
In the subsequent sessions, the autobiography is briefly repeated, now emphasizing the cold memories of the event. The patient may add details that may have been missed and that he/she feels are important. Then subsequent emotionally arousing peaks (the next stones and flowers) are processed, that is, additional traumatic experiences are added to the narration. The procedure is repeated in subsequent sessions until a final version of the patient’s life span and complete biographical highlights are created.
There are several options for the closing session. The lifeline may be completed and used as review of the patient’s life. In cases where the narration has been fully recorded in written form, the document may be read aloud to the patient. The patient, the translator, if present, and the therapist sign the lifeline and/or written narration. A copy of the signed document is handed to the patient. With the agreement or upon request of the patient, another copy may be passed on to lawyers or (in anonymized form) to human rights organizations as documentation of these events. In addition, rituals can be used to ease the mourning and grief. Lastly, the patient may be counseled how to go on with life and is potentially offered further, but now future-oriented sessions (such as adjusting to a new role for a refugee or coping with relationships for a battered woman).
12.3 NET Step by Step
The following procedure follows the treatment manual by Schauer et al. (2011).
12.3.1 Session 1: Diagnosis and Psychoeducation
Prior to the diagnostic assessment for trauma-related disorders, we recommend an extensive checklist of family violence and other traumatic stressors encompassing the entire life span. For adversities during childhood, we recommend the MACE (Maltreatment and Abuse Chronology of Exposure) and for organized violence the vivo checklist (for both see Schauer et al. 2011; German version of the MACE in Isele et al. 2014). The checklists provide the therapist with an indication of the traumatic history of the patient and suggest which events might and should appear on the lifeline.
For survivors of trauma it is vital that they learn to conceptualize and understand their condition. Moreover, they need an explanation about the motivation of the therapist and her/his ability to listen to the worst stories (“I am here to assist people who have experienced extremely stressful conditions such as war (rape, forced migration, torture, massacre, natural disaster) and to document the human rights violations that have taken place. …. We hope to use what we learn from you to improve the way survivors of extreme stress are supported and respected in the future…”).
If the person suffers from symptoms of trauma-related illness, it is advisable to proceed with psychoeducation immediately following the diagnosis. It is important to explain to the patient that alarm and/or dissociative responses are part of the defense repertoire of all humans and that trauma symptoms result when extreme and harmful events have been repeatedly experienced. Explain that memories of the trauma are intrusive memories, which may be triggered by single sensory cues, or internal states, in the mind and body. Provide information that these intrusions are perceived as a current threat, keeping the survivor in a state of vigilance as long as the trauma remains unresolved. The intrusive pictures, sounds, and smells, together with the feelings they elicit, require conscious processing before they can be assigned to the past. This will occur during the course of therapy. The therapeutic procedure is outlined to the patient as an offer. At times, some patients believe that they are an “ill-fated creation of God” or “cursed” and are unworthy of treatment. The reasoning that documentation of human rights violations alone justifies the joint effort involved in therapy is often helpful in these cases. Others found joy in the violence they committed and were proud of the team spirit in gangs or armed groups. There are several reasons that a survivor might feel ashamed or guilty or believe that the therapist will not like what they hear about certain details of the individual’s life. As the therapist, it is important to assure the individual that they have the professional skill to support testifying and that their main job is to provide a beneficial experience, regardless of the details, controversial or otherwise.
12.3.2 Session 2: The Lifeline Exercise
The lifeline in NET displays the emotional highlights of the individual’s life in a ritualized and symbolic way. Hereby the survivor places objects that symbolise major events along a rope or string that symbolizes the continuous flow of biographical time (Fig. 12.3). Flowers designate happy major events and the good times in life, for example, for positive, empowering occurrences; moments of achievement; important relationships; experiences of bliss and acceptance. In this way, flowers can serve as resources. Stones symbolize fearful ordeals, especially traumatizing experiences such as life-threatening events or anything that triggers an alarm response or evokes a dissociative response, like abuse, rape, assault, injury or harm, captivity, natural disasters, accidents, etc. Survivors usually also place stones for difficult moments in life, such as times of hardship (divorce, dismissal, sickness). While further symbols may complicate the exercise – flowers – stones carry a clear message and give structure. Nevertheless, additional symbols may meet the needs for special cases: For very sad experiences that cause continuous grief, like the death of a loved one, a candle can be placed and lit. Criminal offenders or perpetrators committing violent acts may not necessarily be of negative valence, and thus a stone may not be an appropriate symbol, neither would a flower be adequate for victory after a massacre. A more neutral symbol may thus be introduced for these cases: we use a small stick to symbolize participation in any form of aggression or violence, including combat (Elbert et al 2012; Hermenau et al. 2013; Crombach and Elbert 2014). It is good to offer a variety of differently sized, colored, and shaped stones and flowers, so as to give choices for the representation of events.


Fig. 12.3
Lifeline put by a former child soldier. Flowers symbolize positive events, stones symbolize negative events (traumatic, stressful, or sad experiences), and sticks are used for combat experiences and perpetrated violent acts
When the rope/string is put on the floor, the therapist encourages the individual to start placing the symbols along the line. The therapist guides the patient to name and mark important events and turns in life, following a chronological order. For each arousing event, the questions “when?” “where?” and “what?” should be answered with only a few words, without going into the details (e.g., “in secondary school, living in my hometown, I was raped by my neighbor,” “a few months ago, living here in this town, a car hit me,” “during the birth of my first child named ‘Jonnie,’” “at the hospital, I was forced to undergo a Cesarean section,” etc.). The therapist affixes a name to each symbol and notes the where and when. Clear brief naming of the symbol and appropriating it a title is important to build confidence in approaching the hot memories. However, it is crucial to not go any deeper at this point, as the lifeline exercise is not the designated time to begin confronting the content of the event. During this stage of the lifeline procedure, the therapist guides the individual in staying on the cold memory side (questions focus on facts, names, dates, etc., rather than on emotions, sensations, physiology, etc.). The lifeline exercise is only an overview of important life events – a “roadmap.” In this regard, it is helpful to settle and cool down after each symbol placement, especially stones, before placing the next event. The focus remains on the “when?” – naming the life-time period – and “where?” not on the “what?” Otherwise, feelings “pile up” toward the end of the lifeline and emotions get mixed up and confused. In this way, the lifeline tool in Narrative Exposure Therapy is a useful first step toward discussing the traumatic material (Schauer and Ruf-Leuschner 2014; Schauer et al. 2014).
The lifeline was first introduced in trauma therapy with children: KIDNET (Schauer et al. 2004; Onyut et al. 2005) and continues to be utilized as such (Schaal et al. 2009; Catani et al. 2009a; Ruf et al. 2010; Ertl et al. 2012; Hermenau et al. 2012; Crombach and Elbert 2014). Later, the classic lifeline method was adopted in NET for different groups of adult survivors of multiple and complex trauma (Bichescu et al. 2007; Neuner et al. 2008b, 2010; Schaal et al. 2009; Halvorsen and Stenmark 2010; Hensel-Dittmann et al. 2011; Pabst et al. 2012, 2014; Stenmark et al. 2013), sometimes as a paper-and-pencil version, in which the patient marks the biographical highlights along the timeline on a piece of paper (Dōmen et al. 2012; Ejiri et al. 2012; Zang et al. 2013). There is clear evidence for the effectiveness of Narrative Exposure Therapy (NET) with the lifeline being included in the treatment plan. However, treatment success has also been confirmed for Narrative Exposure Therapy without the lifeline module (Neuner et al. 2004b; Schauer et al. 2006; Hijazi 2012) and also, alternatively, with the lifeline module at the end of the therapy (Zang et al. 2014). Conversely, clinical efficacy of the lifeline as a stand-alone procedure in the treatment of traumatized individuals has not been demonstrated and would not be predicted on the basis of the theoretical assumptions presented at the beginning of this chapter.
12.3.3 Session 3: The Narration
The narration begins during the third session, starting at the very beginning of life. The chronology of the narration should address the most arousing events of the patient. The family background should not be neglected: how the patient grew up, what the relationship to his parents was, and what other attachment figures and bonds played a role during the early stages of development (“When are you born and where? Who was bringing you up? Which people were your family? What did they tell you about your first years of life, before your own memory sets in? Any pictures, documents?”). Depending on the resources in terms of the amount of sessions, discussion of the pre-trauma period should remain limited, so as not to avoid narrating the more difficult material later on. Usually time is allocated to work through the first traumatic experience during the same double session (90–120 min) that the narration is initiated. Full expression of the fearful and defensive responding is desirable now during the imagined exposure, allowing for the individual to subsequently experience the reduction in arousal that occurs while narrating the period that followed the most threatening “hot spot.”
The contextual information must first be clearly recollected, and then the event is reported in detail, and, finally, it is put into the past from its present perspective:
WHEN? Time and setting: Establish when the incident took place. Lifetime period? Season of the year? Time of day?
WHERE? Location and activity: Establish as precisely as possible where the incident took place. Where was the person at that time? Begin asking for sensory details of the scenery, the house, the road, etc.
WHAT? Begin the narration, when the arousal begins to rise. Only then, the therapist shifts to slow motion. It may take some courage for both the client and the therapist to deliberately slow down and recall in detail what happened. The therapist supports the processing of the material by allowing the emotional responses to run their course. Hot memory (the associated elements of the fear/trauma structure) is activated involving the following sequence: sensation (what did you see, hear, smell… body position…), cognition (what did you think?), emotion (what did you feel? Note that a therapist will not be able to understand the feelings of a client, as long as the respective thoughts are not known), physiological responses (heartbeat, sweating, cold hands, etc.), and meaning content (Fig. 12.1). The therapist helps to put the hot memory into words and connect them to autobiographical flow, that is, fit them into the narrative. Basically, the therapist keeps pushing on until the experience, especially the emotions, have been put into words and the client starts to feel relief. Stopping anytime before that point is detrimental. The therapist has reached the goal, when a good movie could be made from the client’s descriptions. For the therapist, it is a good idea to let this little film play in one’s mind, although only as if moving together, shoulder by shoulder with the survivor through the scene.
NOW! Let the patient contrast the past and present feelings together with the current bodily sensations: Individual: “At the time of the disaster, I felt horrified, now as I look back, I am getting sad.” Therapist: “I can see you are sighing.” “Your eyes are tearing up now.” “Can you feel the fear in your body now? Where do you feel it?” This will allow the individual to develop better sensorial awareness. There is no need for hesitation when attempting to label the patient’s affective responses: a patient will inform the therapist immediately if the feelings have been labeled incorrectly. Once the fear has been put into words, the client realizes that there is no current danger and that the source of arousal is the memory of a threat rather than an instant threat itself. Consequently, the arousal will decrease.
After the arousal has noticeably reduced, be sure to bring the narrative to a close for this session. Even if time in the session is running out, it is of utmost importance to establish a clear ending to the traumatic event that has been worked on. The way to bring this closure is by transitioning to the time that occurred immediately following the event. To do this, the therapist wants to have the client verbalize in at least a few sentences what happened in the time period following the incident. In case it seems difficult to let go of the emotions of the imagined exposure, a question helpful for moving forward can be to ask how the survivor subsequently managed to live through the aftermath of this event (the hours, days, weeks, and months afterward). This strategy assists in transitioning from stress and discomfort of the hot memory toward session closure by aligning with the directionality of the NET lifeline to which the individual is already accustomed. It is important to clarify the time period following the traumatic event in order to enable the patient to integrate the incident into the greater life story. During “exposure,” arousal and negative emotions are escalating. During “closure,” arousal is decreasing, and the therapist supports this calming down process. Always be clear about the direction in which you are headed.
BOND! The therapist attends to the healing of social pain. The warm, empathic, and nonjudgmental attitude of the therapist while processing the events allows for the healing of attachment wounds. This undertaking invites the establishment of corrective relationship experiences by revisiting old social pain situations in the presence and with the support of a therapeutic relationship.
Hence, the arc of tension within a session begins with storytelling prior to the trauma, proceeds to the details constituting the trauma itself, and then extends to the period occurring shortly after the traumatic event concludes. This allows for the trauma to be contextually situated and for the patient to orient the time and space, as well as the emotional and meaning context, of the event. Before drawing the session to a close, the therapist will ascertain through observation and questioning as to whether the patient’s arousal level has subsided and that the individual once again has their bearings in the present reality.
12.3.4 Session 4 and Subsequent Sessions: Completing the Narration
In the subsequent session, the narrative elaborated in the previous session will be summarized, and the narration of subsequent life and traumatic events is continued. The number of sessions (usually 10–12) required depends on the setting and the severity of PTSD. In complex cases, e.g., in patients with borderline personality disorder, a greater number of sessions may be required (see the case presentation). However, a limit to the number of exposure sessions should be set early on so to circumvent avoidance or delaying of the narration of the worst events.
12.3.5 Cognitive Restructuring and the Days After
At the end of a session, patients often begin to reflect on the meaning content. A more formal cognitive restructuring process may be supported by explicitly pointing out the following:
New insights about the meaning of the event for the patient’s life. Patients may realize how the everyday emotions and unhealthy behavioral patterns (such as general anxiety, mistrust, rage, outbursts of anger) have their origins in the traumatic experience.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





