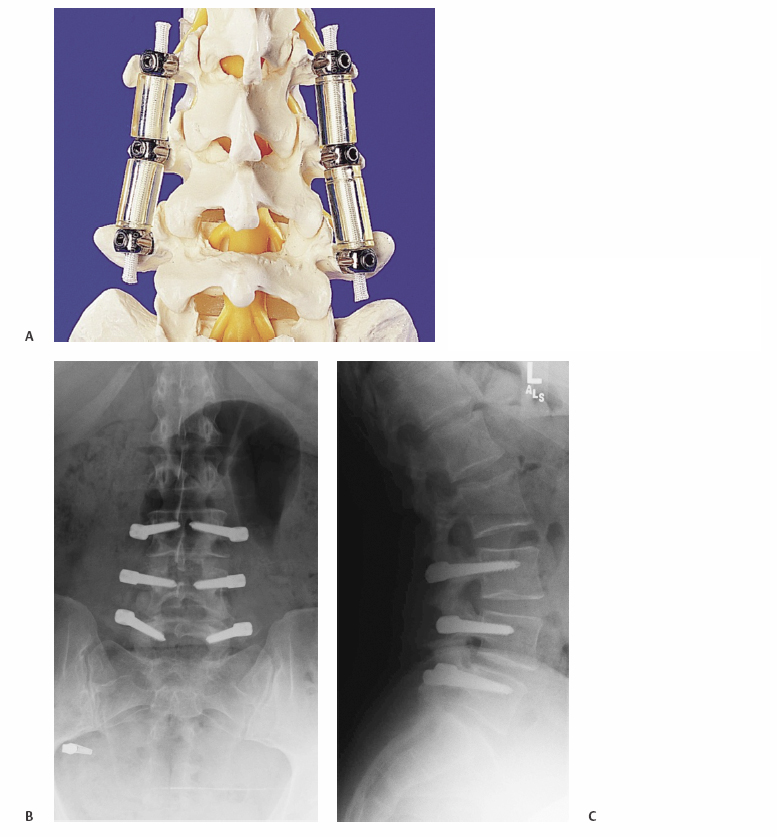
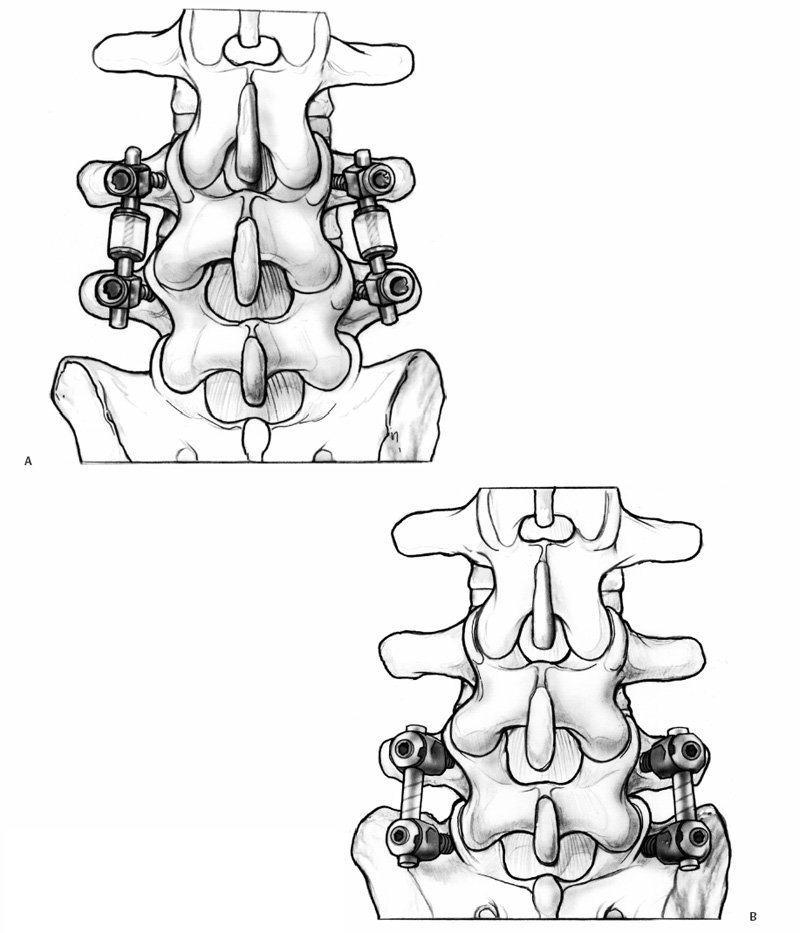
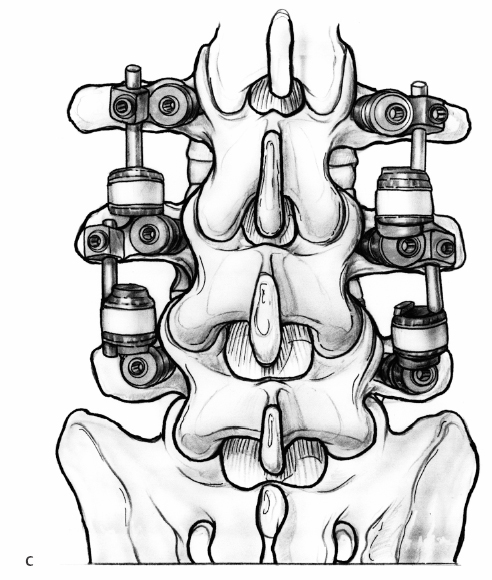
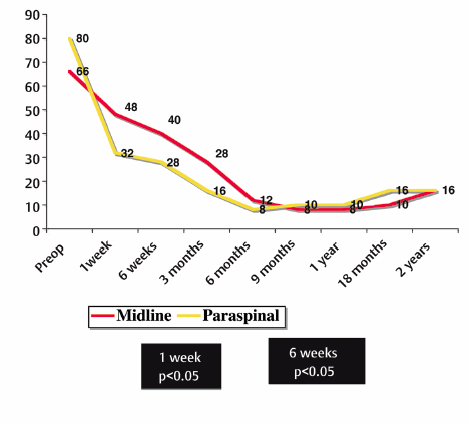
24 Posterior Nonfusion Pedicle Screw-based Stabilization Neel Anand and Eli M. Baron Posterior nonfusion pedicle screw-based stabilization is a technology whose role has yet to be fully defined in the management of degenerative lumbar disease. Numerous devices have appeared in the past 15 years with various proposed indications from discogenic pain to fusion alternatives in cases of possible instability. We review currently available posterior nonfusion pedicle screw-based stabilization systems and discuss their potential indications. We also review our experience with Dynesys (dynamic neutralization system of the spine; Zimmer Spine, Inc., Warsaw, IN), and lessons learned in terms of the treatment of degenerative disc disease (DDD) with pedicle screw-based nonfusion stabilization. The first pedicle screw-based posterior nonfusion system introduced into clinical practice was the Graf ligamentoplasty. The suggestion has been made that these pedicle screw-based systems can function as a tension band theoretically resulting in offloading of the diseased disc with a possibility of functional improvement.1–3 Graf ligamentoplasty was introduced in the 1990s. In this procedure, nonelastic braided polyester ligaments in the form of a loop were applied around pedicle screws under tension to lock the motion segment in extension.4 The Graf ligament in theory shifted the load from the anterior aspect of the disc to the posterior anulus.5 By offloading the painful anterior portion of the disc, the Graf ligamentoplasty theoretically may have been useful in the treatment of back pain.4,6 Grevitt et al5 reviewed the outcomes in 50 patients undergoing Graf ligamentoplasty primarily for DDD. At a mean follow-up of 24 months, they reported Oswestry Disability Index (ODI) scores improving from an average of 59 to 31%. Similarly, Gardner and Pande7 looked at outcomes in patients undergoing Graf ligamentoplasty for DDD. They reported good to excellent results in 62% of patients with an average follow-up of 7.84 years. The mean ODI improved significantly from 59 ± 10 preoperatively to 37.7 ± 14 after 7 years. Brechbuhler et al1 concluded that good results were seen in patients with a combination of facet arthritis, minor disc degeneration, mild loss of intervertebral height, and fit back musculature. Hadlow et al8 compared the results of Graf ligamentoplasty with the results of posterolateral fusion in a retrospective series of 83 patients. They noted a higher revision rate with a Graf ligamentoplasty at 2 years with better outcomes in patients managed by posterolateral fusion. This was significant at 1 year, but at 2 years the differences no longer reached significance. Rigby et al9 also noted poor long-term results with Graf ligamentoplasty. In their retrospective series of 51 patients, they noted a 21.5% complication rate, with 7 patients needing to go on to spinal fusion procedures. The Graf ligamentoplasty has several theoretical drawbacks. The device is applied with compression across the pedicle screws.4,6 As a result of the compression, flexion is restricted and in theory, loads are increased across the posterior anulus. The increased loads across the posterior anulus could theoretically result in disc-related pain. Also reported was increased lateral recess narrowing with hypothetical nerve root compression especially in the presence of preexisting stenosis.6 The most experience with posterior nonfusion stabilization has been with Dynesys (Fig. 24.1). This consists of pedicle screws, which are made of a titanium alloy (Protasul-100) and polyethyleneterephthalate (Sulene-PET) cord and polycarbonate-urethane spacers.3 The Dynesys system was designed to reduce the high revision rate seen with Graf ligamentoplasty. The polyester band used with the Graf system was eliminated and replaced with a cord/spacer between screw heads. As the cord/spacers are nonelastic, flexion compresses disc and the axis of flexion is the posterior ligament. When a patient extends with Dynesys, the anterior anulus opens without compression of the posterior anulus and the Dynesys system theoretically unloads the disc, especially if the patient is in a position of lordosis where the spacers become weight bearing.6 Schmoelz et al10 demonstrated that the Dynesys system offloads the disc in biomechanical testing, especially during extension. Thus, the problem seen with Graf ligamentoplasty where the posterior anulus was overloaded is theoretically avoided, as compression of the posterior anulus is not occurring. Dynesys may also restore the instantaneous axis of rotation to within normal limits in previously degenerated segments.11 Recently, a dynamic magnetic resonance imaging (MRI) study was performed of Dynesys in vivo. Beastall et al12 noted a reduction of motion from the preoperative state at levels instrumented with Dynesys. They confirmed that no reduction occurred in posterior disc height, while a small decrement was noted in anterior disc height. They also noted no significant differences in adjacent segment motion when comparing adjacent levels to the preoperative state. Fig. 24.1 (A) Dynesys implant. Postoperative anteroposterior (B) and lateral (C) radiographs of implanted Dynesys. (A, Courtesy of Zimmer Spine.) Stoll et al13 reported very good results in 83 patients undergoing Dynesys in a multicenter trial. The indications were spinal stenosis, DDD, disc herniations, revision surgery, and others. They noted no screw breakage. The authors postulated that this might be due to the elasticity of the spacers/cord combination, which may cause cyclic peak load on the implant to be lower than in rigid constructs. Theoretically, offloading of the disc may result in reduced disc degeneration. Putzier et al2 compared the results of 49 patients undergoing microdiscectomy alone versus 35 undergoing microdiscectomy with the addition of Dynesys stabilization. They noted that patients with Dynesys stabilization had no further degenerative changes in disc height, configuration, or morphology. They hypothesized that this was due to neutralization of intradiscal pressures and offloading of facet joints. These findings were similar to an earlier series from the same group suggesting Dynesys to be effective in reducing disc degeneration. The series noted this to be true with early disc degeneration, whereas patients with marked degeneration or deformity were deemed inappropriate candidates for Dynesys implantation.2 Grob et al14 reported the results of 31 patients who had undergone Dynesys implantation. They reported a 67% improvement rate. The mean Visual Analog Scale (VAS) score improved from 7.0 and 6.66 to 4.7 and 2.8 for leg and back pain, respectively. They questioned, however, the value of Dynesys implantation as their late reoperation rate was 19%. Nevertheless, Grob et al assessed Dynesys implantation for a variety of indications including lumbar stenosis, spondylosis, disc degeneration, failed back surgery, degenerative listhesis, and extradural tumor. Given the small series and the very heterogeneous group of indications it is difficult to draw any firm conclusions. Bordes-Monmeneu et al15 reported 2-year outcomes in 94 patients undergoing Dynesys implantation. Indications for surgery included disc herniation, DDD, and lumbar stenosis. They reported a decrease in ODI from a mean of 56.8 to 21.4 along with remission of sciatica and back pain in nearly all cases. In conclusion, they noted that Dynesys might be useful when there is a need for “incorporating the functionality concept as opposed to restricting movement. This system can be defined as a disc prosthesis fitted externally to the disc.” Though not implanted in this trial for DDD as an indication, Welch et al16 reported preliminary results from the Food and Drug Administration’s investigational device exemption (FDA IDE) clinical trial of Dynesys. The study included 101 patients undergoing surgery at six trial centers for indications including spondylolisthesis, retrolisthesis, and stenosis, among others. They noted significant improvements at one year in both patient leg and back pain (ODI scores improved from 80.3 to 25.5 and from 55.6 to 26.3, respectively). The authors noted that Dynesys “may be preferable to fusion for surgical treatment of degenerative spondylolisthesis and stenosis because it decreases back and leg pain while avoiding the relatively greater tissue destruction and the morbidity of donor site problems encountered in fusion.” They noted that this may be related to Dynesys preserving the disc and unloading the facet joints, permitting more normal motion. Sengupta4 developed two pedicle screw-based nonfusion stabilization systems that never achieved significant clinical use. Nevertheless, these represent important theoretical considerations in the development of the technology. The FASS (fulcrum-assisted soft stabilization) system was developed to avoid the theoretical limitations of the Graf ligament. The Graf ligament resulted in lateral recess narrowing and increased loading of the posterior anulus. In the FASS system a fulcrum is placed between pedicle screws in front of an elastic ligament. This, in turn, distracts and unloads the disc anteriorly, changing any posterior compressive force into anterior distractive force. The implant also creates lordosis independent of the patient’s musculature and resists the segment going into kyphosis. The dynamic soft stabilization (DSS) system utilizes titanium springs to unload the disc at rest. With motion, depending on the location of the instantaneous axis of rotation, the system would theoretically unload the disc further or become load bearing.4 Highsmith et al17 noted that with widespread use of rigid pedicle screw-based instrumentation for spinal fusions, the incidents of adjacent-level disease appears to be increasing. It has been reported to be as high as 35% to 45%. They reviewed a new generation of spinal implants made of the semicrystalline thermoplastic polymer polyetheretherketone (PEEK). This includes a pedicle screw system utilizing a PEEK rod. The rod is attached to a modified top-loading multiaxial metallic screw (CD Horizon Legacy; Medtronic Sofamor Danek, Memphis, TN). They suggest that the semirigid hybrid of titanium pedicle screws and PEEK rods may have several clinical indications. They state the first scenario is the de novo treatment of spinal instability in which a solid osseous fusion is desired, with less potential adjacent-level stress. They also state a second clinical indication is for patients who have already undergone an instrumented fusion, but in whom adjacent-level disease has developed. Stabilization adjacent to the previous fusion may be desirable when the adjacent level can be stabilized with reduction of the risk of subsequent reoperation in neighboring levels. Finally, they suggest that their potential use of a hybrid PEEK rod/titanium screw construct is to create a tension band (e.g., in a patient with mobile or fixed spondylolisthesis). In these cases, the patient may not need an osseous arthrodesis, but placement of the screw rod construct may limit the progression of any deformity. Recently, several other pedicle screw-based dynamic systems have become available (Fig. 24.2). These include AccuFlex (Globus Medical, Inc., Audubon, PA), PEEK rod (Medtronic Sofamor Danek), Agile (Medtronic Sofamor Danek), and Isobar (Scient’X, Guyancourt, France). Today, there are limited clinical and biomechanical data regarding these devices. Kim et al18 reported clinical results for BioFlex (BioSpine Co., Ltd, Sungdang-gu, Seoul, Korea), a nitinol spring rod dynamic pedicle screw-based stabilization system. Good results were reported using this device to augment posterior lumbar interbody fusion and also as an adjacent segment device in levels primarily treated with a posterior lumbar interbody fusion. Fig. 24.2 Newer pedicle screw nonfusion stabilization systems including Agile (Medtronic Sofamor Danek, Memphis, TN, A); AccuFlex (Globus Medical, Inc., Audubon, PA, B); and Stabilimax (Applied Spine Technologies, Inc, New Haven, CT, C). Mandigo et al19 reported limited results with the Accu-Flex rod system. The AccuFlex like other posterior dynamic stabilization systems has been approved as a fusion device. Recently, Palmer et al20 reported biomechanical and radiographic analysis of a novel pedicle screw-based device that limits extension. This device has been developed by Triage Medical (Irvine, CA) and is implanted into the pedicles at a single spinal level. Bumpers prevent the superior and inferior articular facets from coming in contact and thus limit extension. Additionally, the instrumented spine had 62% less motion during flexion and 49% less motion during extension compared with the intact spine when the device was inserted at L3-L4. Imaging analysis demonstrated 84% less compression of the posterior disc of the instrumented spine during extension and no difference during flexion when compared with the intact spine. Given the reduced motion seen with placement of this device, it may be considered a form of pedicle screw-based dynamic stabilization. Another device in clinical trials is the Stabilimax NZ device (Applied Spine Technologies, Inc, New Haven, CT). This device is designed to reduce the neutral zone. Cadaveric studies have demonstrated reduced bending moments when compared with rigid screws and the Dynesys system. Additionally, the hypothesis of Panjabi has been that the increase in the neutral zone seen in the injured spine creates increasing stresses on the surrounding soft tissue and musculature and this, in turn, increases inflammation responsible for pain generation. Thus, devices that restore the neutral zone (that limit movement to more normal movement) theoretically are associated with reduction in pain.21 Khoueir and colleagues22 suggested various indications for posterior dynamic stabilization. They discussed the need for controlled motion in the iatrogenically destabilized spine. Hypothetically, laminectomy may result in substantial facet joint removal. In some instances, iatrogenic destabilization may occur. One possible role of the posterior dynamic stabilization would be to reduce motion after destabilizing laminectomy, thus avoiding arthrodesis. They also noted that posterior dynamic stabilization devices might be theoretically useful for increased anterior load sharing to augment interbody fusion. They also reviewed the above-mentioned indication of protection and restoration of degenerated disc and possibly facet joints and noted that treatment of discogenic pain is perhaps the least understood area where posterior dynamic stabilization may have a role. Adaptation of nonfusion stabilization techniques for the aging spine is mentioned as a possibility, as current rigid fusion devices provide a high degree of rigidity, which may not be optimal in case of osteopenia. The application of “softer stabilization” techniques may possibly be more desirable in these settings. Lastly, they mention that posterior nonfusion stabilization might be useful to minimize the risk of fusion-related sequelae such as adjacent segment degeneration, iatrogenic flatback deformities, and pseudarthrosis. Scott-Young23 described several possibilities for using posterior dynamic stabilization as a strategy for revision of lumbar disc arthroplasty. His suggestions included patients with facet arthropathy contributing to pain, following disc arthroplasty, patients who experience facet arthropathy years after disc replacement, patients with an eccentrically or undersized disc replacement device resulting in functional spinal imbalance, and lastly as an augmentation in patients with multilevel total disc replacement to avoid coronal imbalance. In the United States, the Dynesys FDA IDE trial was for patients with predominant leg pain with or without spinal stenosis and/or grade 1 spondylolisthesis. The authors have reported off-label use of Dynesys as a posterior nonfusion stabilization system for degenerative disc disease.24 The authors have also reported on the use of Dynesys as a posterior stabilizing device in a hybrid construct.25 Posterior instrumentation is performed here at two or more levels with fusion being performed at the markedly degenerated or unstable level and nonfusion stabilization at the less-degenerated levels. Good short- to mid-term results have been observed in well-selected patients. Our indications today are based on preserving the disc, while at the same time stabilizing the degenerated segment in patients with mechanical loading back pain. Our ideal patient would have mechanical loading back pain with no secondary gain factors limited to one or two levels with the following imaging findings: Stenosis of any degree at the involved level is not a contraindication and we would perform a microscopic laminoforaminotomy to achieve decompression, avoiding a laminectomy. We recently reported on 88 patients who underwent posterior nonfusion stabilization of the lumbar spine at 118 levels using the Dynesys system.26 The indications were spondylolisthesis in 48 patients, 12 retrolisthesis, 52 central/lateral recess stenosis, 6 dynamic foraminal stenosis, and 36 DDD, and 4 patients were instrumented adjacent to a previous fusion. This article discussed the benefits of a paraspinal muscle-sparing approach for posterior nonfusion stabilization as compared with the conventional midline approach. There were no significant complications from surgery. The surgical time and estimated blood loss were 150 minutes and 350 cc, respectively, for the midline approach and 120 minutes and 300 cc for the paraspinal approach. All outcome measures in both groups showed significant improvement at last follow-up. Between the groups there was significant difference in the reduction of the treatment intensity score (TIS) when measured at 1 week and 6 weeks (Table 24.1).26,27 The preoperative 1-week and 6-week values for the midline group were 66, 48, and 40, respectively, and 80, 32 (P < 0.05), and 28 (P < 0.05) for the paraspinal group (Fig. 24.3). This trend continued through 3 months to 6 months though not statistically significant. At 12 and 24 months there was no difference between the two groups. The VAS scores similarly showed a nonsignificant trend to lower values in the first month in the paraspinal group when compared with the midline group. The ODI and SF-36 Health Survey scores similarly showed improvement in both groups, but no significant difference between the groups (Table 24.2).
Brief History
More Recent Systems
Indications
Dynesys System Experience
| The Treatment Intensity Score is calculated by adding all components up and multiplying by 4. Each component is assigned a value 0 to 5. |
| Please answer the questions below, choosing the answer that most closely describes your situation at present. We understand that there may be one or more alternatives that may apply to you, please choose the one you feel is most descriptive of your problem. |
| What medication are you taking for your pain? |
| • None |
| • Tylenol, aspirin, Motrin, Alleve or other non-prescription pain medication |
| • Prescription anti-inflammatories (Relafen, Celebrex, Vioxx, etc.) or muscle relaxants (Soma, Flexeril) |
| • Vicodin, Codeine, Norco |
| • Medrol dose pack/steroids |
| • Morphine analogs (Oxycontin, MS Contin, Percocet, etc.) |
| How long is the pain relieved before you need medication again? |
| • 24 hours or more (rarely take them) |
| • 12 hours |
| • 8 hours |
| • 6 hours |
| • 4 hours |
| • Less than 4 hours |
| How long have you taken these medications? |
| • Use them occasionally only (i.e., do not need them every day) |
| • 6 weeks |
| • 3 months |
| • 6 months |
| • 1 year |
| • 2 years or more |
| Have you needed to seek other treatment options specifically because of pain in your neck or back? |
| • None |
| • Physical therapy, massage therapy, shiatsu, yoga, chiropractor |
| • Acupuncture, acupressure, alternative medicine therapies |
| • Pain management consultation |
| • Injections such as nerve root blocks or epidural steroids |
| • Spinal cord stimulator, morphine pump |
| How often have you had to see a doctor or therapist, or go to the emergency room, specifically because of unbearable pain (disregard any routine follow-up visits)? |
| • Never |
| • Once in 6 months or less |
| • Once in 3 months |
| • Every 6 weeks |
| • Every week or 2 to 3 times a week |
| • Need admission to the hospital for severe pain/surgery |
Source: Anand N, Hamilton JF, Perri B, Miraliakbar H, Goldstein T. Cantilever TLIF with structural allograft and RhBMP2 for correction and maintenance of segmental sagittal lordosis: long-term clinical, radiographic, and functional outcome. Spine 2006;31(20):E748–753; reprinted with permission.
We have also reported on the results of 35 patients undergoing Dynesys stabilization for back pain from lumbar DDD, average age was 44 years with 21 females and 14 males.24 All patients had a clear history of discogenic back pain with no leg pain further corroborated by MRI and/or discogram. Average follow-up was 18 months. In our series, VAS scores were reduced from a preoperative average of 9 to 2.5. Additionally, there were significant reductions in SF-36 and ODI scores.
Surgical Technique
All patients are positioned prone on the Jackson table with care taken to maximize lordosis. Patients needing decompression are operated through a midline approach with microscopic laminotomy/foraminotomy with or without a discectomy followed by posterior nonfusion stabilization. The facet capsule and facet joint are carefully preserved. The midline structures are preserved in all the cases with care being taken to suture the lumbodorsal fascia back to the midline at the end of the procedure. None had a complete laminectomy. Patients not needing decompression are operated with bilateral paraspinal muscle-sparing approaches. In this manner tissue damage is minimized. Additionally, great care is taken not to violate the facet capsules or any of the muscle attachment.
We feel it is imperative to preserve the soft tissue when nonfusion stabilization is performed. Significant muscle damage has been described after midline, muscle stripping approaches to the spine.28–34 Similarly, increased inflammatory mediators have been demonstrated in patients undergoing conventional microdiscectomy versus minimally invasive microdiscectomy.35 Increased edema has been described on MRI in the paraspinal muscles of patients undergoing the midline muscle-stripping approach for open fusion versus those undergoing surgery with a minimally invasive approach.36 Panjabi originated the concept of the neutral zone in the lumbar spine as a region of intervertebral motion surrounding the neutral posture where little resistance is offered by the passive spinal column.37 He observed that the neutral zone might be a clinically important measure of spinal stability function. The neutral zone may increase with injury or degeneration of the spinal column or with weakness of the muscles. This may lead to spinal instability or low-back pain. With an increase in the neutral zone the stresses on the surrounding musculature increased in an effort to maintain the neutral zone, which theoretically may result in pain. Panjabi concluded that the spinal stabilizing system adjusts so that the neutral zone remains within certain physiologic thresholds to avoid clinical instability. It is thus possible that in nonfusion surgery maintaining the soft tissue and musculature surrounding the spinal segment may be significantly more important than in fusion surgery to achieve segmental balance and maintain the neutral zone within physiologic limits. Niosi et al38 confirmed in a cadaveric model that Dynesys implantation reduced the neutral zone to less than the intact spine; the injured spine typically had a significant increase in its neutral zone. We have seen improved functional results in early outcomes in patients undergoing the paraspinal approach for implantation of posterior nonfusion stabilization versus the midline approach.39 We believe that posterior nonfusion stabilization is most likely of benefit to the patients with early evidence of disc degeneration. The patients who have severe disc degeneration or severe facet arthropathy are more likely to benefit from spinal fusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








