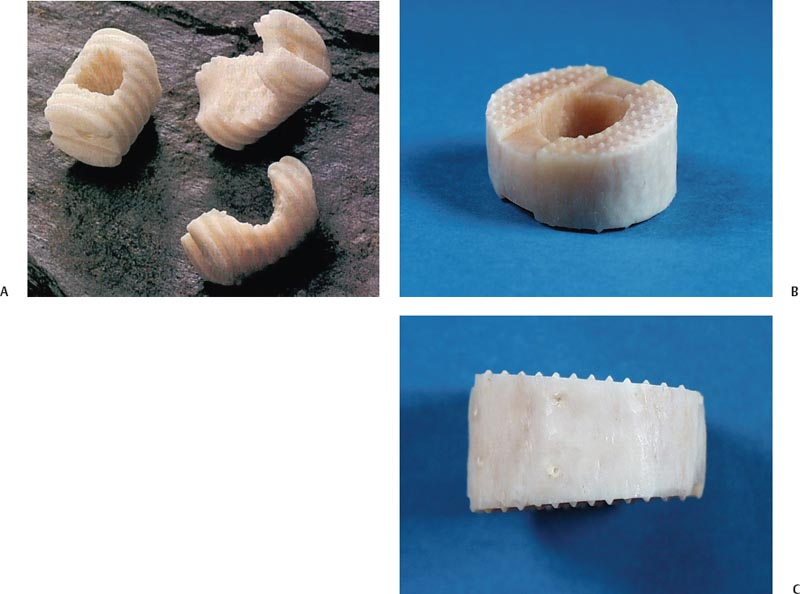
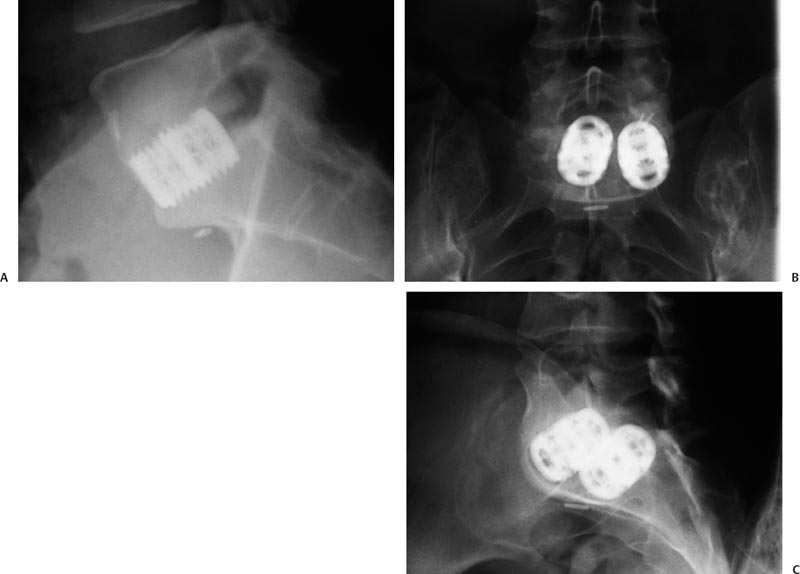
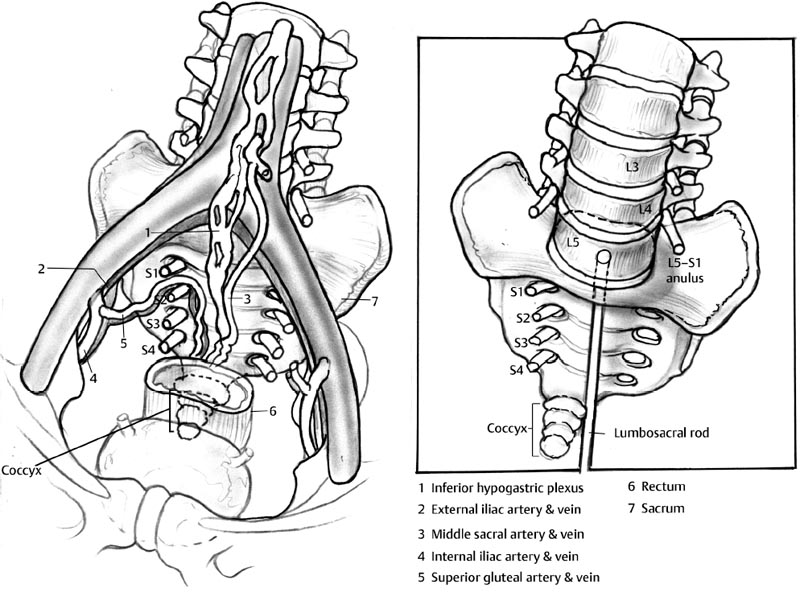
27 Spinal Fusion: Anterior Approach Selvon St. Clair and Isador H. Lieberman The technique of spinal arthrodesis was first described by Albee1 in 1911 for the treatment of Pott disease or spinal tuberculosis. The anterior lumbar interbody fusion operation (ALIF) was first described by Carpenter2 and Burns3 for the treatment of spondylolisthesis. The basic principles of the procedure were outlined starting with an anterior approach to the lumbar spine, complete anterior discectomy, subsequent segment reduction, and correction of spinal deformity and fusion with cadaveric tibial shaft rings supplemented with autologous bone graft. In an attempt to reduce the approach-related morbidity, there have been numerous modifications of the procedure to incorporate the minimally invasive philosophy. In addition to the classic open transperitoneal approach,4 ALIF can now be effectively performed via the laparoscopic transperitoneal,5 open retroperitoneal,6 mini-open retroperitoneal,7 and endoscopic retroperitoneal approaches.8 Further, two new approaches for anterior lumbar fusion have recently been described and include the percutaneous transsacral9 and the lateral transpsoas10 approaches. Furthermore, the increased popularity of ALIF is attributed, in part, to the recent development of threaded metallic interbody cages and the available supply of allograft dowels and other osteogenic factors. Regardless of the specific approach, ALIF usually yields a consistently high fusion rate with good to excellent postoperative clinical outcomes, thereby representing a valuable option for anterior fusion of the lumbar spine. Before the 1980s, the anterior interbody lumbar spinal fusion operation had only one widely accepted indication: the treatment of spondylolisthesis. Excellent clinical outcomes are expected when anterior interbody fusion is used to supplement posterior segmental instrumentation and fusion of spondylolytic spondylolisthesis.11 This technique has been proven to be safe and effective for patients even with high-grade slippage.12 Since its initial application, the indications for anterior lumbar interbody have expanded and are now effectively employed to treat a variety of disorders of the lumbar spine. At present, ALIF is used for the treatment of axial back pain from degenerative disc disease, recurrent disc herniation, failed posterior spine fusion, and postlaminectomy syndrome.13,14 In addition, it is used for the treatment of certain spinal infections and spinal tumors. Furthermore, in spinal deformity correction for both sagittal and coronal plane imbalances, anterior interbody fusion has the role of reestablishing a clinically acceptable degree of lumbar lordosis. Perhaps the most widely accepted role of ALIF is in providing the foundation for long spinal fusion and supplementation of posterior instrumentation and fusion. This is especially important for patients with poor bone stock and patients at risk for nonunions. Finally, anterior interbody fusion is also used for indirect foraminal decompression when posterior approaches are contraindicated. The goals of interbody fusion are essential to keep in mind when planning to perform ALIF. There are three main goals of the procedure: the attainment of solid fusion; the restoration of lumbar spine anatomy; and finally, the reduction or minimization of approach-related complications (see Complication section). To ensure a solid arthrodesis, meticulous attention to the following techniques is paramount. First, a thorough discectomy and endplate preparation is done to ensure maximum bone to bone contact. This is accomplished by reaming or curettage. The goal is to establish clean endplates with sufficiently bleeding bone. Since the anterior longitudinal ligament is sacrificed, care must be taken to establish good soft tissue tension about the interspace to adequately secure the implants. Keep in mind, a carefully performed complete circumferential discectomy provides a large surface area for the interbody graft of choice to be implanted. The availability and variety of graft materials has significantly increased for anterior interbody fusion. Coupled with the recent modifications of the anterior approaches to the lumbar spine, the availability of a new generation of interbody devices is directly related to the excellent outcome and popularity of ALIF. The graft materials include the gold standard: tricortical iliac bone. The utility of this graft is limited by the morbidity associated with anterior graft harvest, which can be as high as 30%.14 In addition to the aforementioned limitation, the compressive strength of these grafts does not exceed physiologic axial loads during routine spine motion,15–17 and have been shown to fatigue. These limitations can result in early failure as assessed by loss of disc space height, pathologic motion, and increased rate of pseudarthrosis. The increased use of allograft bone for anterior interbody fusion is attributed to the morbidity associated with autologous graft harvest, its higher compressive strength relative to endplates and cancellous bone,18,19 and the recent advances in allograft bone harvesting and preparation. Femoral allografts are now available in a precisely machined aseptic threaded bone dowel or femoral rings that can be implanted directly into the intervertebral space (Fig. 27.1 ). In addition, the center of the femoral allograft is usually filled with autologous bone, which has been demonstrated to yield a good fusion rate in several studies.20–24 Further refinement of the femoral allograft by demineralization of its surface has been theorized to increase fusion rate, but evidence to support this claim is currently unavailable. The limitations of availability of allograft bone and the slight increased risk of disease transmission have somewhat curtailed the widespread use of this particular interbody graft material. The development of metallic threaded interbody fusion devices (titanium and carbon fiber implants) is attributed, in part, to the inherent limitations of allograft bone materials. The devices are designed to be used as a composite graft with either osteoinductive or osteogenic materials. The metallic threaded interbody fusion devices facilitate fusion while concurrently providing immediate stability and maintenance of disc space height. Although first developed by Bagby to treat cervical stenosis (wobbler syndrome) in horses in the early 1980s, the concept was quickly adapted for the treatment of lumbar degenerative disc disease.25–27 The first cage (BAK) was successfully implanted, in 1991, and was found to promote excellent interbody fusion (Fig. 27.2A,B). In biomechanical studies these devices have been shown to stabilize the spinal motion segments to reliably promote fusion.19,28–32 Certain cylindrical cages are now designed with a tapered end, to more reliably restore lumbar lordosis (Fig. 27.2C).31,33 Clinically, metallic threaded interbody fusion cages have been shown to stabilize the lumbar spine motion segment for fusion adequately without the requirement of supplemental fixation.24,34,35 Finally, despite the lack of solid available clinical evidence to substantiate this claim, carbon fiber composite implants are available and have been touted to improve fusion rates as a result of their modulus, which may allow for greater load sharing than the titanium implants. Fig. 27.1 Allograft graft materials. (A) Bone dowels. (B,C) Femoral ring allografts. Fig. 27.2 (A) Lateral radiograph showing BAK cage substituted into the L5-S1 intervertebral disc space with excellent restoration of disc space height and lumbar lordosis. Anteroposterior (B) and lateral (C) radiographs show newgeneration threaded cages inserted into the L5-S1 disc space. Restoration of spinal anatomy is critical for successful anterior interbody fusion. Tensioning of the soft tissues and ligaments that surround the disc space restores the disc space height and enhances retention of the interbody graft. Furthermore soft tissue tensioning facilitates the use of larger interbody cages, which increases the surface area for fusion.29–31,36,37 It is crucial to obtain or correct the proper spinal balance, in both the coronal and the sagittal planes, which is caused by intradiscal distraction and soft tissue conditioning. It has been demonstrated that perhaps more important than the use of tapered cages to restore adequate lordosis is the degree of intradiscal distraction and retensioning of the anulus. Another aspect in correction of spinal anatomy is indirect neuroforaminal decompression by restoration of foraminal dimensions that have been reduced as a result of disc space collapse. This is facilitated both indirectly by restoration of adequate disc space height and directly by anterior decompression of the radial bone spurs or disc material.33 Surgical approaches to the anterior lumbar spine can be performed by either transperitoneal or retroperitoneal approaches. Recently, newer techniques have been described to gain access to the anterior lumbar spine. These are based on the minimally invasive principles and include the following approaches: the lateral transpsoas, the transsacral approach, the endoscopy- or laparoscopy-assisted approach, and the mini-open ALIF. The anterior lumbar approaches are performed by experienced orthopaedic and neurosurgery surgeons or by general or vascular surgeons. The techniques for these approaches will be discussed in detail below with emphasis placed on the more commonly employed approaches. Because surgical exposure of the different zones of the lumbar spine present unique challenges to the surgeon, the open approach to upper (T12-L2), middle(L2-L5), and lower (L5-S1) lumbar zones will be described separately. For approaches to the thoracolumbar junction patients are normally positioned in the lateral decubitus position. For the midlevel approach, they may be either lateral decubitus or supine; for lower lumbar regions, a combination of positioning may be appropriate but usually the patient is supine. The surgical team should ensure that bony prominences are well protected by padding and the patient is comfortably secured on the operating table. Pneumatic sequential compressive devices are applied to the patient’s legs to reduce the risk of deep vein thrombosis. A Foley catheter is usually placed to assist with fluid management. The hips and knees are usually flexed to loosen any tension on the psoas muscle and lower extremity vasculature. The retroperitoneal approach to the lumbar spine was first described by Iwahara38 and Harmon39 in the early 1960s and later modified by Mayer,40 who added the muscle-splitting component. For exposure to the thoracolumbar region, the senior author prefers an extrapleural or extracavitary approach to prevent potential complications associated the violation of the pleural cavity. An oblique thoracoabdominal incision is usually made over the 11th or 12th rib and is extended a few centimeters down onto the abdominal wall. Exposure to the rib of interest is then obtained by dividing the subcutaneous tissues and the serratus anterior and latissimus dorsi muscles. The intercostal muscles are then divided to expose the superior border of the rib, which is then partially resected after having been subperiosteally dissected free from surrounding tissues to protect the underlying neurovascular bundle. At this point, the external and internal oblique muscles are divided in line with their fibers. The underlying transversalis layer is split to gain access to the peritoneum, which is carefully dissected off the diaphragm and the psoas muscle for entry into the retroperitoneal space. At this time, proponents of an intracavitary approach will take the diaphragm down to gain access to the anterior thoracolumbar junction, but in our experience, this step can be bypassed. To reduce extensive blood loss, careful vessel ligation is important. Overlying the vertebral bodies are the paired segmental vessels, which are dissected and divided as close to the aorta as possible to prevent disruption of the collateral circulation to the spinal cord. Preventing disruption of the collateral circulation to the spinal cord reduces the chance of catastrophic cord ischemia.41,42 Access to the anterior disc space is then unhindered. Notably, careful attention should be paid to the artery of Adamkiewicz, which usually arises on the left between T8-T10, but may vary between T7 and L4. It provides blood flow to the anterior and posterior spinal arteries, in the thoracolumbar area, and its disruption can lead to paraplegia. At this anterior lumbar zone, injury to the retroperitoneal lymphatics is not uncommon but can be reliably managed by oversewing the lymphatic chain. The midlumbar spine zone is usually exposed via a retroperitoneal approach using a left anterior paramedian incision to avoid injury to the prominent sided vena cava and right common iliac vein. For exposure to the L3-L4 disc space, the skin incision should commence as close to the umbilicus as possible. The incision is then taken through the subcutaneous tissues down to the anterior abdominis rectus muscle and sheath, which is then divided in line with the skin incision, extending into the external oblique muscle. At the junction of the posterior rectus muscle and sheath is the arcuate line, an access corridor to the retroperitoneal space, which can be developed by bluntly separating the peritoneum off from lateral to medial direction to the posterior rectus sheath. The peritoneal sac is then dissected off of the psoas muscle and the left ureter, and the iliac artery and vein are then identified. Self-retaining retractors are employed to maintain the exposure while the surgeon gains access to the disc spaces. A detailed understanding of the presacral neuroanatomy (Fig. 27.3) is paramount for careful dissection in this zone because one has to mobilize the left iliac artery and vein medially and the divided lumbar segmentals laterally. For exposure to the L2-L3, and L3-L4 levels, little or no segmental vessel ligation is needed. The exception is, on occasion, when the lumbar vessels along the anterior body of L4 must be divided for safe mobilization of the great vessels. Furthermore, the tethering of the iliac vein by the ileolumbar or ascending vein over the L5 is common and is usually sacrificed to gain adequate exposure to the L4/5 disc space. The ileolumbar vein can be quite large, between 3 to 5 mm at its entry to the left common iliac vein, and accidental injury can result in massive hemorrhage. To ligate this vessel, the sympathetic trunk is first identified along the anterior border of the psoas muscle. The groups of fibers that anchor this muscle to the superior and inferior vertebral margins are released to facilitate lateral retraction. The L5 nerve root is usually found in proximity to the ileolumbar vein and care must be taken to avoid its resection. Several incisions may be used for retroperitoneal access to the anterior lumbo-sacral junction. They include a paramedian incision, a transverse incision with either a muscle-cutting or muscle-splitting approach,39 an oblique incision extending from the iliac crest and ending a few centimeters proximal between the umbilicus and pubic symphysis, and a Pfannenstiel incision—low transverse incision. The incision is again carried through subcutaneous tissue down to rectus muscle, which is mobilized to the midline. The retroperitoneal space is then developed directly anteriorly by bluntly separating the peritoneal sac from lateral to medial because iliac arteries and veins cross the lateral aspect of the L5-S1 disc space. The ipsilateral ureter is normally identified and swept toward the midline along with the peritoneum. At this point, the sacral promontory and the L5-S1 disc are exposed by careful dissection between the iliac vessels. Division of the middle sacral vessels and resection of the thin anterior longitudinal ligament complete the approach. In the retroperitoneal approaches to the lumbosacral junction, fibers of the pelvic sympathetic plexus may be damaged, resulting in retrograde ejaculation in a male patient. Although concerned patients have been advised to bank their sperm, retrograde ejaculation is a rare phenomenon and is ephemeral if it does occur.
Indications
Goals
Surgical Approaches
Patient Positioning
Open Approaches
Retroperitoneal
Thoracolumbar Zone (T12-L2)
Midlumbar Zone (L2-L5)
Lumbo—Sacral Zone (L5-S1)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








