INTRODUCTION
The chapter by Chana et al. provides a comprehensive overview of the biological mechanisms that underpin neuropsychiatric disorders in HIV-infected individuals. Their review of the latest evidence on the neuropathogenesis of HIV infection helps shed light on how HIV-associated neurocognitive disorders (HANDs) develop as well as on how specific co-factors, such as substance abuse, may facilitate these disorders. These types of biologic mechanisms provide critical insights into the natural history, prognosis and management of mental disorders in HIV. However, understanding and addressing the burden of mental disorders in HIV-infected individuals is more complex than the pathophysiology of a viral infection of the central nervous system. A broader framework is required to help think about both the risk of mental disorders in HIV-infected individuals and the disease burden associated with HIV and mental illness at a population level.
MULTILEVEL APPROACH TO THINKING ABOUT MENTAL DISORDERS AND HIV
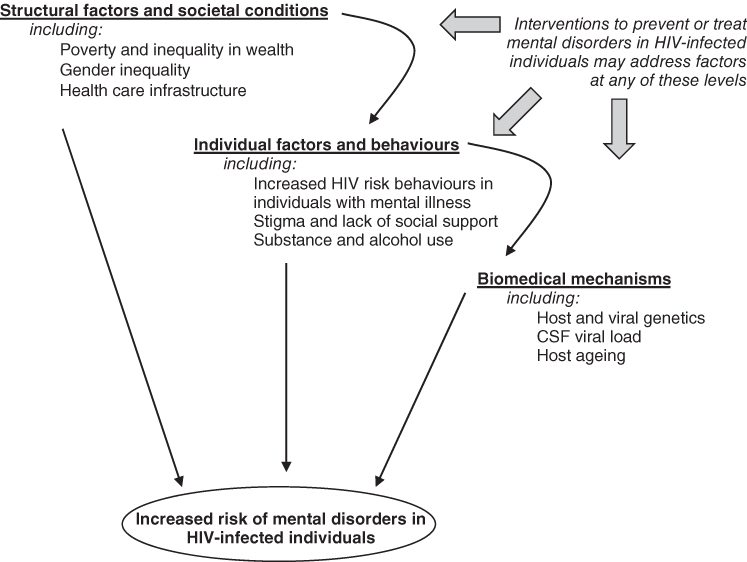
In this broader consideration, a multilevel formulation provides a valuable model for thinking about the interaction of HIV and mental illness at a range of different levels of biological and social organization (Figure 2.1.1). The review by Chana of the aetiology and pathogenesis of HIV-associated disorders, including HANDs, focuses on biological mechanisms from the organ system and tissues (e.g. the blood–brain barrier) to the level of the neuron. However, there are also important upstream approaches to thinking about the pathogenesis of mental disorders in HIV that manifest beyond the central nervous system and extend to individual behaviours and the features of societies that help shape these. Such ‘social pathologies’ range from behaviours related to an individual’s risk of HIV acquisition and/or mental disorders, to the broader set of structural factors that create conditions to facilitate or prevent HIV and/or mental illness in communities.
Figure 2.1.1 Multilevel framework for thinking about the factors involved in the pathogenesis of mental illness and HIV.
MENTAL DISORDERS AND THE TRANSMISSION OF HIV INFECTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



