Vignette 2
Obstructive Sleep Apnea Associated With Cerebral Hypoxemia
An increase in the arousal threshold may predispose critically ill patients with obstructive sleep apnea (OSA) to prolonged apneas and death. In one early study, impaired arousal was hypothesized to have led to prolonged apneas, electroencephalogram (EEG) flattening, and generalized tonic spasms described as “cerebral anoxic attacks.”1 We present two critically ill patients with OSA, in whom elevated arousal thresholds may have prolonged obstructions, leading to diffuse cerebral hypoxemic EEG patterns, followed by transient encephalopathy in one subject and death in the other (Vignette Figs. 2.1 to 2.3).2,3
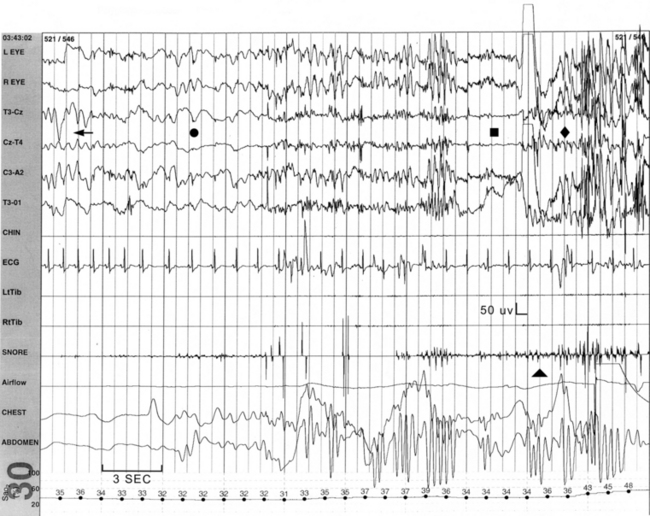
VIGNETTE FIGURE 2.1 The patient described in case 1 suffered a prolonged 90-second obstructive apnea, during which the electroencephalogram (EEG) revealed a sudden change from a classic rapid eye movement sawtooth pattern (arrow) to a poorly organized, diffuse delta slow wave pattern (closed circle) followed by a general flattening of all activity (square) that led to attempts to arouse the patient (as evidenced by diffuse movement artifact; diamond). Nevertheless, persistent obstruction (triangle) necessitated emergent rescue breathing maneuvers. Persistent EEG flattening followed by slowing and eventual recovery of normal waking patterns was appreciated in subsequent epochs. L, Left; R, right; T, temporal; C, central; O, occipital; CHIN, mentalis electromyogram (EMG); LtTib, left anterior tibialis EMG; RtTib, right anterior tibialis EMG; SNORE, snoring microphone; Airflow, nasal airflow; CHEST, thoracic respiratory effort; ABDOMEN, abdominal respiratory effort; Sao2 (%), arterial oxygen saturation. (Modified from Dyken MD, Yamada T, Glenn CL, et al. Obstructive sleep apnea associated with cerebral hypoxemia and death. Neurology. 2004;62:491-493.)
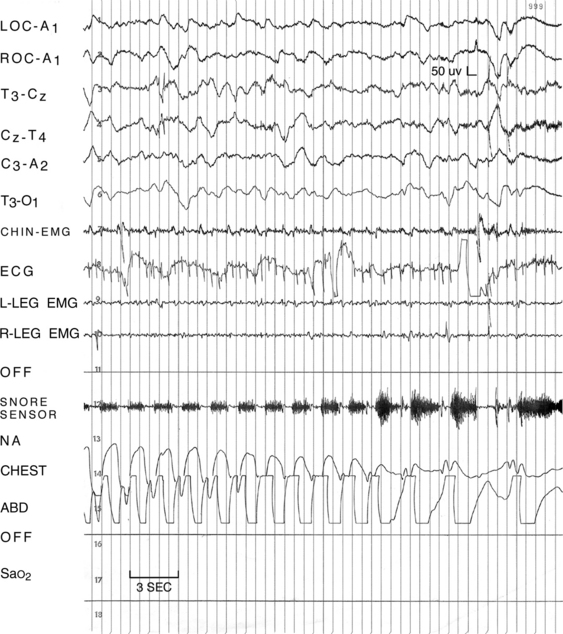
VIGNETTE FIGURE 2.2 The subject described in case 2 had a 30-second obstruction that was associated with an SaO2 low of 12%. At that time there was a dramatic change from the preceding stage N3 polysomnographic pattern, with an electroencephalogram that showed progressive development of a disorganized, delta/theta slow wave pattern over a 2.5-minute period. LOC, Left outer canthus; ROC, right outer canthus; A1, left ear reference; A2, right ear reference; T, temporal; C, central; O, occipital; EMG, electromyogram; L-LEG, left leg; R-LEG, right leg; NA, nasal airflow; CHEST, chest effort; ABD, abdominal effort; Sao2, arterial oxygen saturation. (Modified from Dyken ME, Afifi AK, Im KB. Stroke in sleep. In: Chokroverty S, Sahota P, eds. Acute and Emergent Events in Sleep Disorders. New York: Oxford University Press; 2011:328-348).
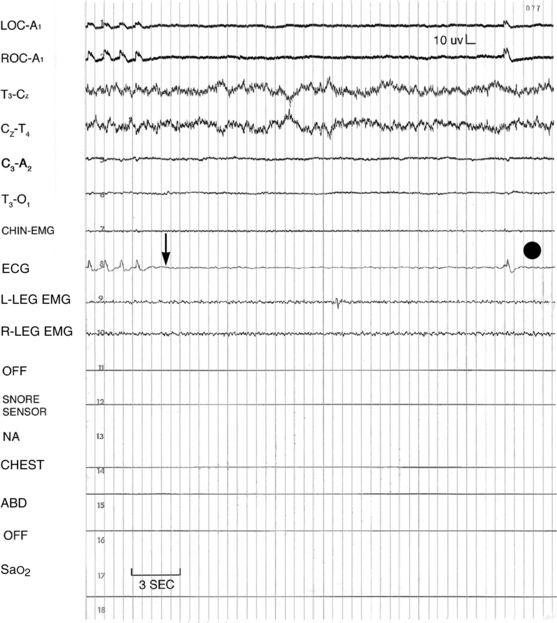
VIGNETTE FIGURE 2-3 Following the subject in the final series of apneic events in case 2, no discernible electroencephalographic activity was captured while using a recording sensitivity of 1.0 μV/mm. A prolonged period of asystole (arrow) was followed by cardiac arrest, at which time the patient was declared dead (closed circle). LOC, Left outer canthus; ROC, right outer canthus; A1, left ear reference; A2, right ear reference; T, temporal; C, central; O, occipital; L-LEG, left leg; R-LEG, right leg; NA, nasal airflow; CHEST, chest effort; ABD, abdominal effort; Sao2, arterial oxygen saturation. (Modified from Dyken MD, Yamada T, Glenn CL, et al. Obstructive sleep apnea associated with cerebral hypoxemia and death. Neurology. 2004;62:491-493).
Case 1
A 52-year-old man with multiple previous diagnoses that included OSA, pulmonary hypertension, diabetes, and myocardial infarction was admitted to the hospital for a coronary artery bypass. A polysomnogram with a bilevel positive airway pressure (BPAP) titration was requested because he had persistent snoring with gasping arousals, sleepiness, and morning headaches. During rapid eye movement (REM) sleep there was a 90-second obstructive apnea, with a minimum oxygen saturation (SaO2) of 31%, followed by diffuse EEG slowing (not compatible with the patient’s normal slow wave pattern of stage N3 [NREM 3] sleep), suggesting cerebral hypoxemia (see Vignette Fig. 2.1). This apnea persisted despite increasing BPAP to 15/10 cm H2O, loud commands, shaking, and sternal rub. After 30 seconds of unresponsiveness, the initial EEG slowing was immediately followed by a 45-second period of flat/absent EEG activity (using a recording sensitivity of 7 μV/mm). At this time emergency rescue breathing was initiated, and after two breaths he resumed his normal waking breathing pattern and opened his eyes. Within 30 seconds he responded in a slow/encephalopathic manner, and after 19 seconds his baseline cognitive functioning returned. During this time there was a progressive buildup of diffuse theta slow wave activity that was followed by a mixture of minimal theta with interspersed occipital alpha rhythm. Following full arousal it took 45 seconds for the normal baseline EEG to return. Later, BPAP at 29/25 cm H2O resolved all obstructions, and the patient reported better sleep than usual.








