39 Transcanal Transpromontorial Endoscopic Approach for Vestibular Schwannoma Resection
39.1 Introduction
Totally endoscopic surgery is now a well-accepted minimally invasive technique for the treatment of many anterior skull base pathologies. While in these cases endoscopic approaches have become well established, totally endoscopic approaches to other areas of the skull base such as the cerebellopontine angle (CPA) and the internal auditory canal (IAC) have been limited. Currently, endoscopy in CPA surgery is primarily used as an adjunct to conventional microscopic surgical techniques for vestibular schwannoma (VS) treatment. The first application of the endoscope to IAC surgery was to assist in visualization with the retrosigmoid approach. After removal of the CPA component, the intracanalicular portion was removed under endoscopic visualization, trying to avoid extensive drilling of the posterior aspect of the petrous bone,s. Literatur , s. Literatur or using a keyhole retrosigmoid approach.s. Literatur Endoscope-assisted microsurgery (EAM) of the CPA has provided an excellent initiation of the endoscope into posterior fossa surgery,s. Literatur and the advances in the application of endoscopy in the surgical treatment of middle ear cholesteatomas and neoplasmss. Literatur , s. Literatur , s. Literatur , s. Literatur have further improved its acceptance in otology and lateral skull base surgery. With the gradual development and progression of middle ear endoscopic surgery, greater comfort and skill with endoscopic inner ear anatomy and surgery has come.s. Literatur Microscopic approaches for treatment of VS have been firmly established and their outcomes widely studied, including the retrosigmoid/suboccipital, transmastoid-translabyrinthine, and subtemporal middle cranial fossa approach.s. Literatur All these methods require external incisions with variable degrees of temporal bone drilling to adequately expose the IAC and CPA. Recently, progression from EAM to a fully endoscopic technique to the IAC for VS resection has been described and clinically applied.s. Literatur , s. Literatur In 2012, an exclusive endoscopic approach, the transcanal transpromontorial endoscopic approach (TTEA), to the IAC was described and used to resect a cochlear schwannoma (CS) involving the IAC.s. Literatur Since this time, several publications documenting VS resection using the TTEA have emerged.
39.2 Transcanal Transpromontorial Endoscopic Approach to the IAC
In the TTEA, the external auditory canal (EAC) is used as natural surgical corridor to reach the fundus of the IAC, passing through the cochlea and the vestibule and exposing the entire IAC (Fig. 39‑1 ). From an anatomical point of view, this approach allows the surgeon to work on the medial wall of the tympanic cavity and lateral skull base, avoiding cerebellum and middle and posterior fossa manipulation and potentially reducing the morbidity related to standard approaches. Since cochlear drilling is mandatory in order to access the IAC, any residual hearing is sacrificed with this procedure (Fig. 39‑2 ).


39.3 Indications
Growing or symptomatic VS limited to the IAC with nonserviceable hearing (type C or D, according to AAO-HNS [American Academy of Otolaryngology–Head and Neck Surgery] classification).
CSs, with or without IAC involvement.
Residual or recurrent VS involving the IAC, after prior microsurgical resection.
39.4 Surgical Technique
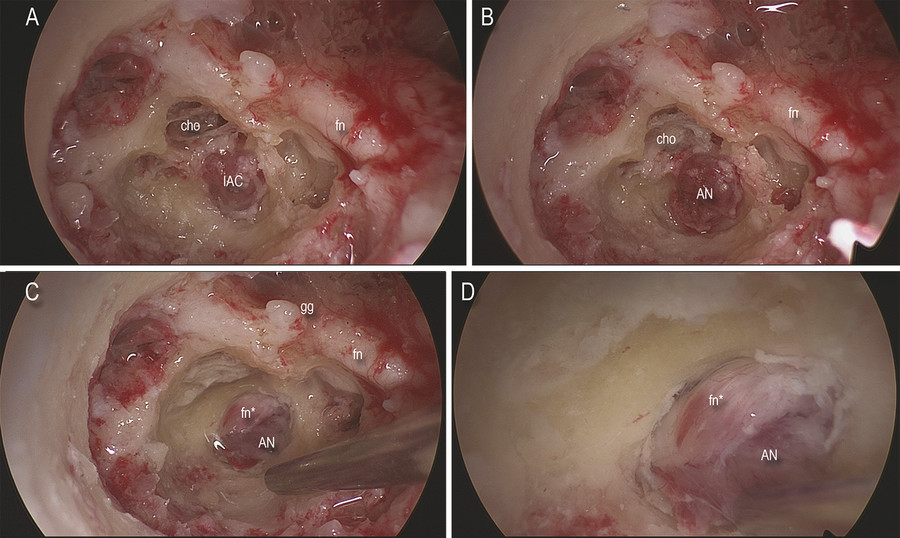
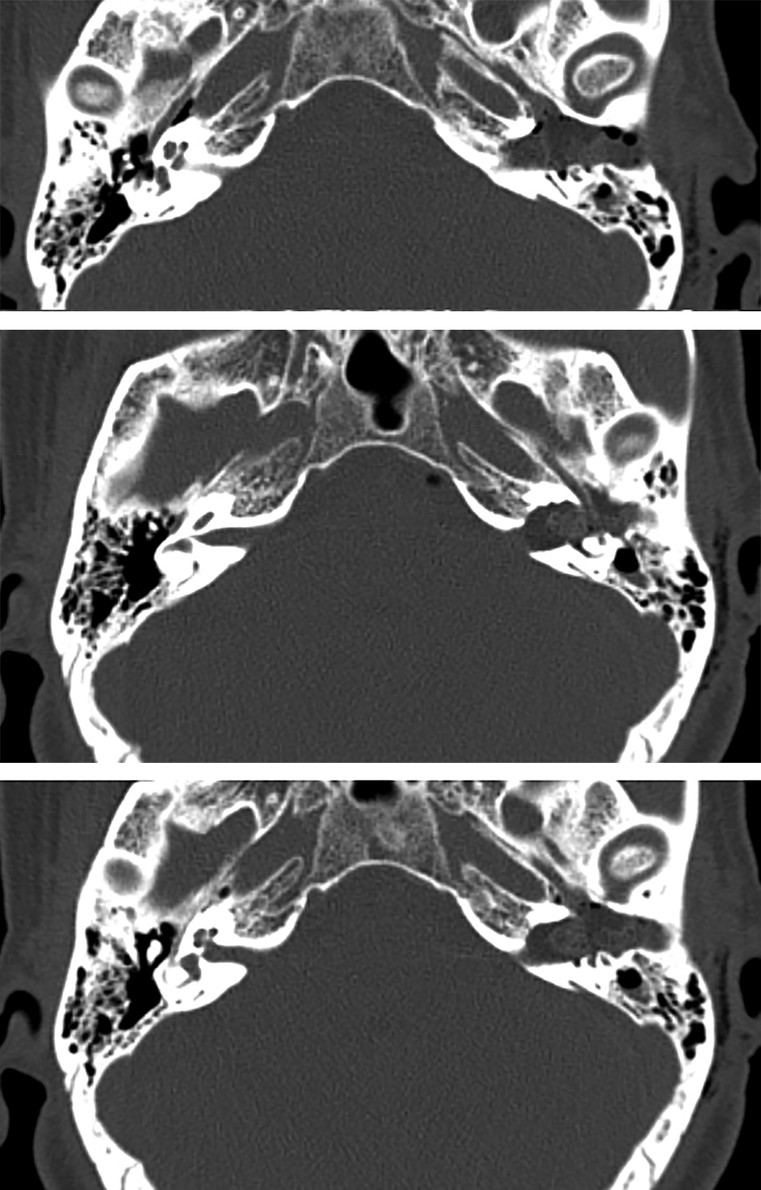
A 0-degree rigid endoscope (Karl Storz, Tuttlingen, Germany) is used, 15 cm in length and 3 mm or 4 mm in diameter. An AIDA three-chip high-resolution monitor and camera (Karl Storz, Tuttlingen, Germany) are employed. The patient is positioned supine, the head gently rotated to the other side, with facial nerve monitoring (NIM) applied. A circumferential skin incision of the EAC is made with a round knife under 0-degree endoscopic view, between the cartilaginous and bony portions of the EAC. The skin is elevated circumferentially with the tympanic membrane, detaching the annulus from the bony ring. The flap, pedicled on the umbus, is transposed laterally and then detached from the malleus using a microscissors ensuring that all skin is removed to avoid iatrogenic cholesteatoma. After the tympanic cavity is exposed (Fig. 39‑3 a), the bony EAC is drilled (Fig. 39‑3 b), with the anterior limit being the temporomandibular joint and the posterior limit being the mastoid segment of the facial nerve, providing maximum surgical access to the medial wall of the tympanic cavity. The bony annulus is then circumferentially drilled, progressively exposing the hypotympanum, protympanum, retrotympanum, and attic spaces, with the ossicular chain and promontory region well visualized (Fig. 39‑3 c). Ossicular chain disarticulation is then performed as a necessary step to access the entire medial tympanic cavity. The incus and the malleus are removed, leaving the stapes undisturbed (Fig. 39‑3 d). The tympanic segment of the facial nerve is exposed from the second genu to the geniculate ganglion, located between the cog and the cochleariform process. After this, the stapes is removed, entering into the vestibule and identifying the saccule (Fig. 39‑4 a,b). The spherical recess in the saccular fossa is endoscopically identified, since this structure marks the end of the inferior vestibular nerve and represents an important landmark for the localization of the fundus of the IAC. The bony overhang of the round window niche is drilled, exposing the membrane of the round window. Using a piezosurgery instrument (Mectron, Carasco/Genova, Italy), the promontory with lateral aspect of the otic capsule is removed at the cochlear level, identifying the basal, middle, and upper turns of the cochlea (Fig. 39‑4 c). After exposing the cochlear turns, the bony wall between the cochlea and the spherical recess is carefully drilled, entering the fundus of the IAC (Fig. 39‑4 d). Dissection of the IAC is performed, following the dura of the IAC from the fundus to the porus, progressively exposing the VS (Fig. 39‑5 a). The bones between the IAC and the internal carotid artery anteriorly, the IAC and the mastoid portion of the facial nerve posteriorly, the IAC and the jugular bulb inferiorly, and the IAC and the tympanic segment of the facial nerve superiorly are removed circumferentially. The bone of the otic capsule is removed from lateral to medial, thereby exposing the dura of the medial surface of the temporal bone, representing the deepest limit of the dissection. After IAC exposure, the dura is opened and the VS is more fully exposed (Fig. 39‑5 b). At this time, identification of the facial nerve in the IAC is mandatory in order to avoid facial nerve injury (Fig. 39‑5 c); the use of a facial nerve stimulator can help the surgeon during dissection. The tumor is then carefully dissected and removed in piecemeal fashion while maintaining the integrity of the facial nerve (Fig. 39‑5 d). When the VS has limited extension into the CPA, the bone of the porus can be enlarged using a diamond burr so that the last portion of the tumor can be safely dissected in the angle. Once tumor dissection is complete, an inspection of the IAC is performed to confirm complete tumor resection (Fig. 39‑6 a–c). Closure is performed with abdominal fat, packing the promontorial defect and closing the communication between the inner ear and middle ear (Fig. 39‑6 d). Fibrin glue is used to fix the fat graft into the promontorial defect; a piece of muscle is used to close the eustachian tube orifice. The whole EAC is filled with fat, and a blind sac closure of the skin of the EAC is performed. The authors do not routinely employ intensive care unit observation, and a computed tomography (CT) scan of the brain is performed 6 hours after the surgery (Fig. 39‑7 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








