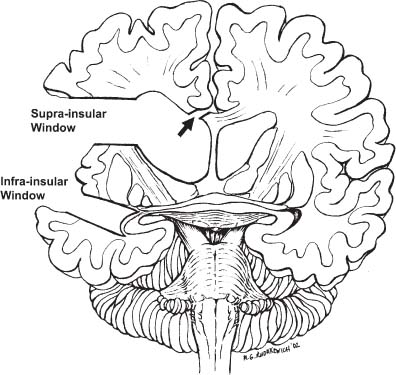
69 Diagnosis Rasmussen’s encephalitis causing epilepsy partialis continua Problems and Tactics A previously healthy 5-year-old boy was diagnosed with Rasmussen’s encephalitis following the acute onset of left-sided focal seizures without an associated alteration in level of consciousness. His seizures progressed to the point where almost continuous clonic activity in the left thumb and hand was observed. Because of this child’s diffuse hemispheric disorder, a periinsular hemispherotomy was undertaken in an effort to control his epilepsy. Keywords Periinsular hemispherotomy, epilepsy, pediatric, Rasmussen’s encephalitis This 5-year-old boy had a normal birth and neurological development prior to the acute onset of left-sided focal motor seizures, which were unassociated with an altered level of consciousness. The seizures were initially brief, involving the face and arm and/or leg, but gradually, over the course of weeks, they progressed despite medical management with numerous antiepileptic medications. He ultimately developed epilepsy partialis continua involving the left thumb and hand. As his seizure disorder evolved, the child developed a progressive left hemiparesis affecting the arm more than the leg. He remained cognitively intact throughout. Lumbar puncture did not reveal any evidence of an infectious encephalitic process. Magnetic resonance imaging (MRI) of the brain demonstrated scattered areas of cortical T2 hyperintensity in the right parietal lobe; the lateral, inferior, and medial aspects of the right temporal lobe; and the right inferior frontal lobe and right cingulum. There was slight associated volume loss of the right cerebral hemisphere. The left hemisphere was normal in appearance and signal intensity. Magnetoencephalography (MEG) and magnetic source imaging (MSI) demonstrated spike sources diffusely localized to the areas of the right cerebral hemisphere which showed cortical swelling and high T2 signal (Fig. 69–1). Prior to the definitive operation for control of this child’s epilepsy, a biopsy of the right superior temporal gyrus was undertaken. The result was consistent with a diagnosis of Rasmussen’s encephalitis. The procedure described here is a slight modification of that outlined by Villemure and Mascott.1 A question-mark-shaped scalp flap, with its inferior limb extending down to the root of the zygoma and its superior limb extending to just above the area of the superior temporal line, was elevated. A generous frontotemporoparietal craniotomy was then fashioned. A semicircular durotomy overlying the sylvian fissure, with releasing cuts into the frontal and parietal lobes, provided appropriate access to the cortical surface. FIGURE 69–1 (A) Axial magnetic resonance imaging/MEG magnetic source imaging/magnetoencephalography (MRI/MEG) depicting multiple spike clusters in the Rolandic region, a finding typical for Rasmussen’s encephalitis. (B) Coronal MRI/MEG illustrating position of spike clusters in the hemisphere that showed only mild atrophic changes. No focal lesions were found on MRI. The first intradural maneuver was to create a suprainsular window, which would allow for exposure of the upper part of the insular cortex (Fig. 69–2). Image guidance was used to create a representation of the insula onto the overlying frontal and parietal opercular cortex. This opercular cortex and underlying white matter were then resected using a subpial aspiration technique until the insular cortex and the circular sulcus that surrounds it were exposed. An attempt was made to preserve the large arteries and veins at the posterior end of the sylvian fissure to minimize postoperative swelling of the disconnected hemisphere. FIGURE 69–2 Artist’s rendering of neurosurgical corridors created for complete hemispheric disconnection. Both supraand infrainsular windows are necessary to gain access to the lateral ventricle. From this approach, the callosotomy can be performed as shown through the suprainsular window (arrow). The frontal and temporal lobe opercula are removed to expose the insular cortex, which will also be removed.
Rasmussen’s Encephalitis Causing Epilepsy Partialis Continua
Clinical Presentation
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree