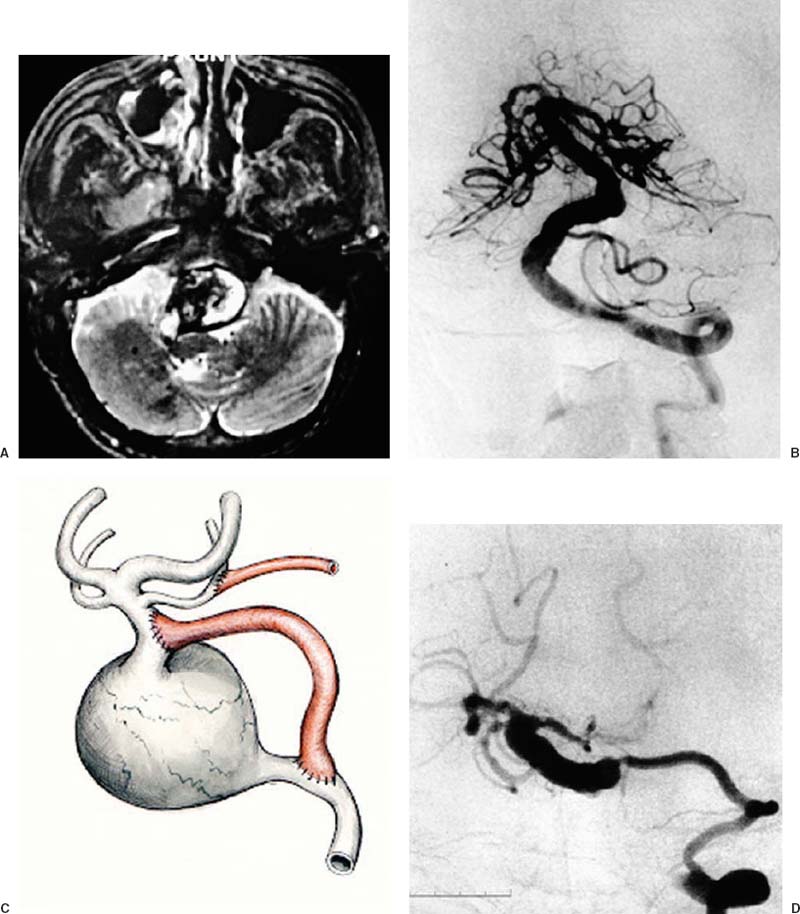
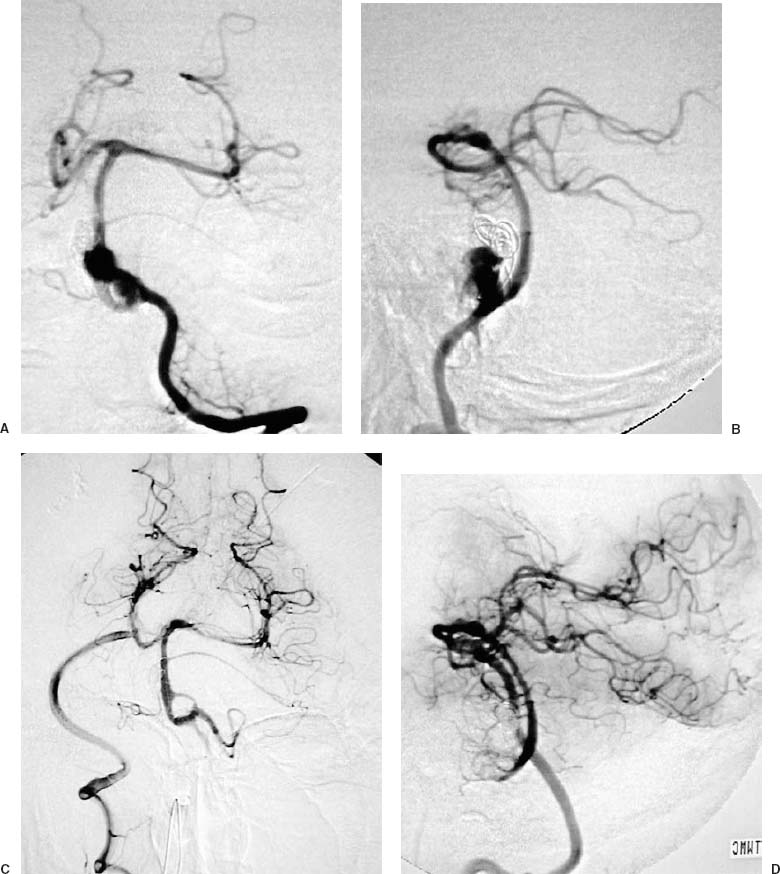
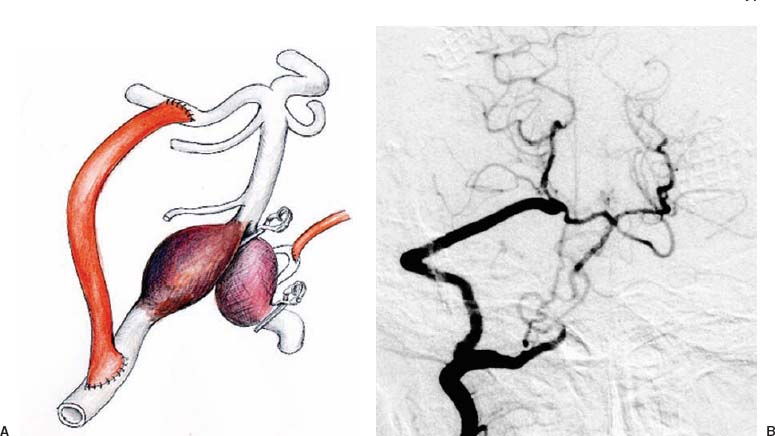
71 Diagnosis Thrombosed basilar artery aneurysm (Case 1); dissecting aneurysms of bilateral vertebral artery with large thrombus (Case 2) Problems and Tactics Although superficial temporal artery–superior cerebellar artery (STA–SCA) and occipital artery–posterior inferior cerebellar artery (OA–PICA) have been used for vascular reconstruction of the posterior circulation, these bypass pedicles may not immediately provide a major increase in blood flow.1 Earlier in our experience, we had treated complex vertebrobasilar aneurysms by using either a vertebral artery–vertebral artery (VA–VA) radial artery (RA) interposition graft or a vertebral artery–basilar artery (VA–BA) radial artery interposition graft for vascular reconstruction (Fig. 71–1). These bypasses are technically more difficult to perform than distal SCA or posterior cerebral artery (PCA) anastomosis and have a higher risk of ischemic complications. This prompted us to develop a PCA–VA radial artery graft bypass, which will provide an adequate volume of blood flow immediately. In the early 1980s, Sundt et al had already published the procedure for a PCA–external carotid saphenous vein graft bypass.2 In our method, the V3 segment of the VA is used as a donor vessel. The advantage of the V3 segment as a donor vessel is that it can be exposed more easily than the external carotid artery (ECA) in our modified lateral semiprone position.3 In addition, the graft flow may be identical to the pretreatment state. The length of the graft is relatively short (~10–12 cm) compared with the ECA–PCA radial artery graft (~16–18 cm). With our increasing experience, we have found that this procedure is also effective in the treatment of medically intractable severe stenosis of the BA. In this case report, we describe the operative procedure of the PCA–VA radial artery graft bypass. Keywords Vertebrobasilar aneurysms, PCA-VA radial graft bypass, severe stenosis of BA. FIGURE 71–1 Illustrative case of a vertebral artery–basilar artery (VA–BA) bypass using a radial artery (RA) interposition graft in a case with thromosed giant aneurysm of the BA. Prior to making a VA–RA–BA bypass, a superficial temporal artery–superior cerebellar artery (STA–SCA) bypass had been performed for reducing ischemic complications. The postoperative consciousness was clear but preoperative paraparesis worsened to tetraparesis due to circulatory disturbance of the perforating arteries. (A) Preoperative magnetic resonance imaging (T2-axial). (B) Preoperative left vertebral angiography (VAG) (anteroposterior). (C) Schematic drawing of a bypass between the V3 portion of the VA and the P2 of the posterior cerebral artery using a radial artery graft. (D) Postoperative left VAG (oblique view). FIGURE 71–2 Illustrative case with thrombosed giant aneurysm of the basilar artery treated with a V3–RA–P2 bypass. Prior coil embolization did not stop further enlargement of the aneurysm. (A,B) Preoperative bilateral VAGs (oblique view). (C,D) Postoperative right VAGs (anteroposterior view and lateral view). A 48-year-old man presented with a 2-year history of right abducens paresis. Diagnosis of a thrombosed BA aneurysm was made (Fig. 71–2). During the following period of observation, dysarthria, dysphasia, gait ataxia, and incoordination of the limbs gradually appeared. Four months prior to surgery, the patient underwent intravascular coil embolization. The symptoms were aggravated postoperatively with neumonitis and he needed a respirator for respiratory control. Just before the V3 segment of VA–radial artery graft–P2 segment of PCA (V3–RA–P2) bypass surgery, the patient had ataxic respiration, quadriparesis, and bilateral abducens pareses, although he was able to come off the respirator. FIGURE 71–3 Illustrative case with bilateral dissecting aneurysms of vertebral arteries treated with a V3–RA–P2 bypass. (A) Schematic drawing of a V3–RA–P2 bypass using a radial artery graft. (B) Postoperative right VAG (oblique view). A 52-year-old man developed the left Wallenberg syndrome. The examination revealed a dissecting aneurysm of the left VA with a large thrombus (Fig. 71–3). The patient underwent OA–PICA bypass with trapping of the left VA in the subacute stage. At this point, there was no dissection found in the right VA. He was discharged from the hospital on foot with remaining left Wallenberg syndrome. Four months later, he was brought in the hospital with decreased consciousness and was found to have a highly stenotic right VA. The consciousness level improved with medical treatment; however, the single photon emission computed tomography (SPECT) examination revealed highly decreased blood flow in the entire posterior fossa. In the subacute stage this time also, a V3–RA–P2 bypass plus OA–PICA bypass surgery was performed. This bypass is composed of nine steps: 1. Preparation of the STA and OA pedicle and radial artery graft 2. Exposure of the V3 segment 3. Combined transpetrosal (retrolabyrynthine presigmoid) craniotomy 4. Exposure of the PCA 5. STA–SCA anastomosis 6. P2–RA anastomosis (distal suture) 7. Introduction of the RA graft to the extracranial VA and RA–V3 anastomosis (proximal suture) 8. Opening of the graft and pressure monitoring 9. VA or BA ligation if necessary
The Posterior Cerebral Artery–Vertebral Artery Bypass Using Radial Artery Graft for Complex Aneurysms and Severe Occlusive Diseases of the Basilar Artery
Clinical Presentation
Case 1
Case 2
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree