Fig. 10.1
Diagram of the brain through the midsagittal plane showing the locations of capsulotomy (cap), cingulotomy (c), and stria terminalis (ST) lesioning
10.3.1.1 Anterior Capsulotomy
A lesion is created in the anterior limb of the internal capsule starting at the frontal horn of the lateral ventricle along the head of the caudate nucleus (Fig. 10.2). The genu of the capsule stands out clearly in sagittal views, and the lesion is made in this region. We tend to start the lesions in the posterior part of the limb at the level of the anterior commissure, moving in an anterior direction at higher levels. Bilateral lesions are produced, in most cases by performing two overlapping thermocoagulations on each side, using an electrode 4 mm long and 2 mm in diameter (Elekta Instruments®).
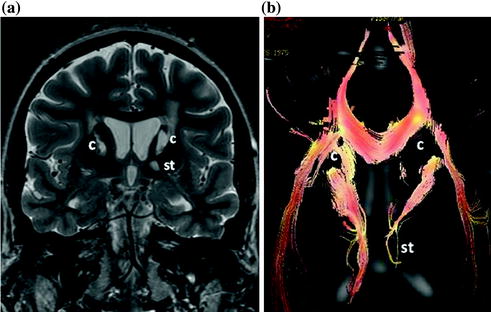
Fig. 10.2
Coronal MRI (a) and an overlay of MRI and tractography in the axial projection (b) after bilateral anterior capsulotomy (c) and stria terminalis (st) lesioning
10.3.1.2 Anterior Cingulotomy
Lesions are effected in the anterior cingulum adjacent to Brodman areas 24 and 32 (Fig. 10.1) and may be unilateral or bilateral [2, 20, 25]. We currently use tractography to locate the cingulum and to verify the degree of disconnection achieved. Thermal lesions are made using an electrode 4 mm long and 2 mm in diameter. The lesions we make are smaller than those previously described and are restricted exclusively to the cingulum.
10.3.1.3 Stria Terminalis Lesioning
This procedure was described in the 1970s and has been developed by Dr. Juan Burzaco, with good results [32]. The stria in the external, posterior part of the frontal horn 2 mm lateral, 1 mm anterior, and 1 mm superior to the anterior commissure is located (Fig. 10.2). This procedure is useful in alleviating the aggressive behaviour and depression that is sometimes associated with obsessions . Lesioning is ordinarily carried out in the tract on the left side. In contrast to the two previous procedures, simultaneous bilateral lesioning may give rise to such adverse secondary effects as hyperthermia, confusion, and persistent nausea-vomiting lasting up to a week. An electrode 4 mm long and 1 mm in diameter (Elekta Instruments®) is used.
10.3.1.4 Combined Lesioning
Unlike neurostimulation, stereotactic ablative surgery allows various lesion procedures to be combined in a single intervention. In cases of OCD associated with depression or anxiety, we perform bilateral anterior capsulotomy together with bilateral anterior cingulotomy . If compulsions and aggression are also a major component, left stria terminalis lesioning is added to the other two procedures.
Other teams have used two additional lesion procedures:
10.3.1.5 Subcaudate Tractotomy
Neurosurgical lesions are produced in the substantia innominata , an area ventral to the caudate nucleus , containing neuronal cell bodies with connections similar to those in the ventral portions of the striatum and the globus pallidus. Lesions are created in the fibres that connect the thalamus to the orbitofrontal cortex and cingulated gyrus [7, 27, 46].
10.3.1.6 Limbic Leucotomy
This procedure combines subcaudate tractotomy and anterior cingulotomy [21].
10.3.2 Gamma Knife Radiosurgery
We have performed capsulotomies and cingulotomies using Gamma Knife radiosurgery (Elekta Instruments®). With our equipment, 192 beams of gamma radiation emitted by Cobalt-60 sources are focused on the target to be treated, the lesions can be located in the posteriormost areas of the anterior limb of the internal capsule (Fig. 10.3) or in the cingulum (Fig. 10.4) [23, 33]. The radiation dose of the individual beams is low, but focusing 192 beams with high precision so that they converge on a single point for exposure times of several hours subjects the selected anatomical site to doses equal to or greater than 120 Gy, producing a lesion at the desired point while at the same time achieving low adjacent radiation exposure. The primary advantage of this technique is that it obviates having to make any incisions in the skull.
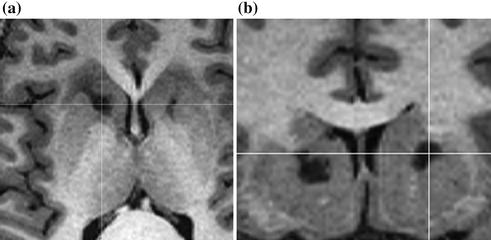
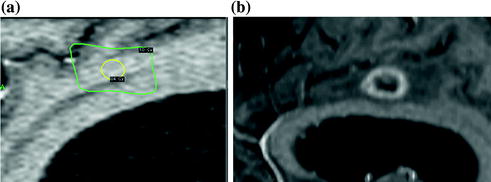
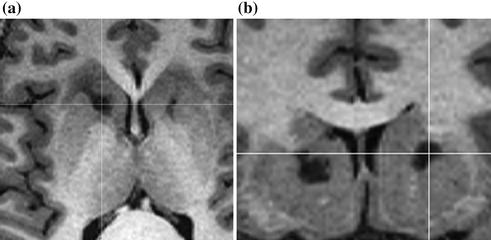
Fig. 10.3
Axial (a) and coronal (b) MRI 18 months after bilateral anterior capsulotomy performed by Gamma knife radiosurgery
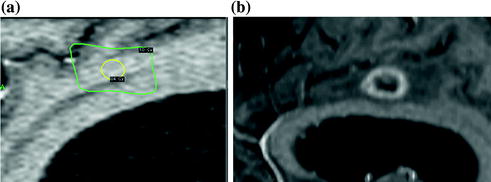
Fig. 10.4
Cingulotomy performed by gamma knife radiosurgery : dose planning (a) and MRI follow-up one year later (b)
10.4 Clinical Course and Procedure Results
Results are to be assessed at least six months after surgery, and changes in patient condition take place up to two years after the procedure [34]. There are scales for rating OCD symptoms, the most common being the Yale-Brown obsessive compulsive scale (Y-BOCS). The Beck and Hamilton scales are also used, to rate anxiety, along with scales to rate quality of life , Lehman’s quality of life (QOL) scale being the one most commonly employed.
10.4.1 Anterior Capsulotomy
Initial results reported by Dr. L. Leksell yielded favourable responses in 50 % of OCD cases [19, 29]. Later series of patients treated from the 1970s to 1990s achieved improvement in 70 % of OCD patients undergoing the procedure [35, 40, 45]. Results for recent series have been consistent with these latter success rates, with fewer adverse effects [30, 41]. Outcomes for patients treated by Gamma Knife radiosurgery reported by the Karolinska Institute team have been similar [23].
Immediate undesirable secondary effects associated with this procedure are transient, lasting three to six months, and include headache, transient urinary incontinence, impaired cognitive function, especially memory, and confusion. Focal neurological deficits associated with haemorrhage and tardive epileptic seizures have been observed in 3 % of cases [10, 35].
10.4.2 Subcaudate Tractotomy
Series published from the 1970s to the 1990s yielded a significant percentage improvement in around 50 % of OCD cases, with good results in 40 % of patients suffering from anxiety. Epileptic seizures in 2 % of cases were the most frequent adverse effect apart from initial, transient symptoms similar to those reported for capsulotomy [27].
10.4.3 Anterior Cingulotomy
Large series have been reported over the past 40 years, with improvement rates in OCD patients ranging between 56 and 36 % of cases [3, 20]. For the most recent published series there were complete long-term responses in 47 % of cases and partial responses in 22 % [11]. Anxiety improved to a large extent, specifically in 43 % of cases in the most recent series [26, 43]. Immediate, transient symptoms have included headache, confusion, and urinary incontinence. Tardive epileptic seizures have affected up to 9 % of cases in some series. With modern targeting procedures this unwanted effect has now decreased considerably.
10.4.4 Limbic Leucotomy
Initial results were extremely encouraging, with 89 % of OCD patients improving [22]. In more recent studies the improvement rate for OCD patients has reached 80 % [9, 24]. Adverse effects include drowsiness for variable lengths of time, confusion, urinary incontinence, and cognitive impairment lasting longer than in other procedures.
10.5 Our Results
Over the past 10 years our team has operated on 100 OCD patients with suitable follow-up of cases; current mean follow-up is six years. Obsessions and compulsions underwent significant improvement in 71 % of the OCD cases treated. Improvement was evidenced by a sustained decrease of more than 50 % in the Y-BOCS score. Overall, quality of life in these patients improved in 75 % of cases as measured by Lehman’s quality of life (QOL) scale in late follow-up, with scores increasing by 50 % or more [32].
Transient symptoms observed for time periods of between two and six months have included confusion, some degree of cognitive impairment, urinary incontinence, fever of central origin, nausea-vomiting, hallucinations, heightened response to psychotropic medication, and tardive depression. Haemorrhagic lesions were observed in 5 % of cases, requiring intervention in two cases (40 % of the patients with bleeding), infections were recorded in 2 % of cases, and epileptic seizures were observed in 4 % of formerly seizure-free patients.
Results are attained gradually over the course of the two years following surgery, as confusion and cognitive impairment improve. In 30 % of cases patient condition worsened, making a second surgery necessary. In the cases that underwent a second surgical intervention, improvement was similar to the rate achieved after the first procedure.
10.6 Gamma Knife Radiosurgery
10.6.1 Bilateral Anterior Capsulotomy
There have been few published series since the 1960s [23, 28, 29, 31, 33, 42]. With improvements in imaging definition, the precision of lesion localization has increased, with less damage to more posterior areas of the thalamus. Symptoms improve without collateral effects to the extent that surgery succeeds in cutting off only the anterior limb of the internal capsule by locating the target in the area that includes the medial connections of the internal capsule between the thalamus and the basal frontal region visualized by functional MRI. For cases with the proper indications, outcomes are similar to those attained using open ablative procedures, that is, significant improvement in 70 % of cases. Changes appear in patients from between six months to a year after treatment, and our team has not observed any adverse effects, though cognitive impairment and other disorders such as apathy (indifference towards one’s surroundings) have been reported in a significant number of cases in earlier series with long-term follow-up [9]. These effects have been related to the presence of lesions in the posterior and basal regions of the thalamus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







