Abnormal Shape/Configuration of Corpus Callosum
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Normal Variant
Callosal Dysgenesis
Callosotomy
Neoplasm
Lipoma
Glioblastoma Multiforme
Lymphoma, Primary CNS
Decreased White Matter Volume
Hypomyelination
Periventricular Leukomalacia
HIE, Term
Cerebral Infarction, Chronic
Diffuse Axonal Injury (DAI)
Multiple Sclerosis
Radiation and Chemotherapy
Obstructive Hydrocephalus
Less Common
Holoprosencephaly
Holoprosencephaly Variants
Rare but Important
Hypertensive Intracranial Hemorrhage
Marchiafava-Bignami
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Normal corpus callosum (CC) varies in thickness, shape
Isolated callosal dysgenesis not common
Look for second lesion
Associated CNS anomalies in > 50%
Heterotopia
Cortical dysplasia
Noncallosal midline anomalies
Abnormal brainstem or cerebellum
If not congenital, history crucial!
Helpful Clues for Common Diagnoses
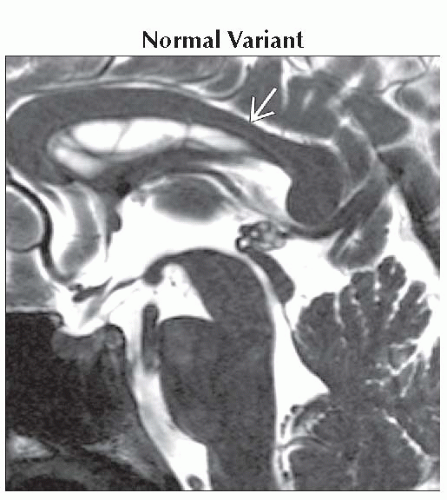
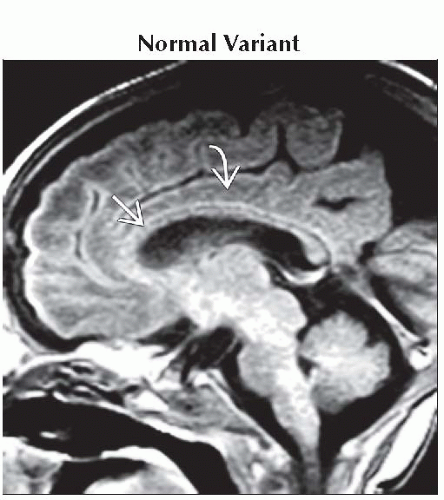
Normal Variant
Size, shape, thickness of normal CC vary
Splenium, genu are largest parts of corpus callosum
Narrowing between body, splenium (“isthmus”) is normal
Dorsal surface of fully developed, normally myelinated corpus callosum often “wavy”
Immature corpus callosum is thin
Pre-myelination
Gradually thickens with progressive myelination
Callosal Dysgenesis
One or all segments absent
Rostrum, splenium most likely deficient
Remnants vary in size, shape, configuration
“Micro” CC
Small, but well-formed
Often syndromic
“Mega”CC
Isthmus usually absent
Megalencephalic (bulky white matter)
Or small to normal brain (syndromic)
Callosotomy
Surgical disruption
Focal: Approach to 3rd ventricle or suprasellar tumor
Diffuse: Surgery for intractable seizures
Best seen on sagittal or coronal MR
Neoplasm
Can be benign/focal or malignant/diffusely infiltrating
Lipoma
40-50% interhemispheric fissure
Common in callosal dysgenesis
Can be bulky, mass-like (“tubonodular” type, usually associated with CC agenesis; may extend through choroidal fissures into lateral ventricles)
Thin mass curving around CC body/splenium (“curvilinear” type, CC present but may be dysgenetic)
Glioblastoma Multiforme
“Butterfly” glioma
Central necrosis + thick irregular rim enhancement
Lymphoma, Primary CNS
Hyperdense on NECT
Strong, uniform enhancement
Decreased White Matter Volume
Many causes (congenital, acquired)
All may result in focal or diffuse callosal thinning
Hypomyelination
Chromosomal, inborn errors of metabolism
Periventricular Leukomalacia
Premature infant
“Scalloped” lateral ventricles
HIE, Term
Term infant with profound partial asphyxia → WM/cortex damaged
Cerebral Infarction, Chronic
Axonal loss → focal/diffuse thinning CC
Diffuse Axonal Injury (DAI)
20% involve CC (splenium, undersurface posterior body)
Multiple Sclerosis
Chronic, late
Obstructive Hydrocephalus
Acute
Corpus callosum (CC) stretched
CC bowed upwards
Forniceal columns bowed downwards
Chronic
Post-shunt encephalomalacia
Sequela of acute callosal impingement against falx
Helpful Clues for Less Common Diagnoses
Holoprosencephaly
Corpus callosum absent in alobar
Large dorsal “cyst” often present
Semilobar may have residual splenium
Frontal fusion & hypoplasia
Splenium may be present
Lobar
Genu may or may not be present
Gray matter often crosses with genu
Holoprosencephaly Variants
Middle interhemispheric variant
a.k.a., syntelencephaly
Splenium, genu present, body deficient
Middle CC body “dips”
Gray matter crosses at dip
If severe, add bilateral perisylvian polymicrogyria
Helpful Clues for Rare Diagnoses
Hypertensive Intracranial Hemorrhage
CC rare primary site
Marchiafava-Bignami
Middle-aged alcoholic
CC demyelination, necrosis, atrophy
SELECTED REFERENCES
1. Pierson TM et al: Mega-corpus callosum, polymicrogyria, and psychomotor retardation: confirmation of a syndromic entity. Neuropediatrics. 39(2):123-7, 2008
2. Samaranch L et al: SPG11 compound mutations in spastic paraparesis with thin corpus callosum. Neurology. 71(5):332-6, 2008
3. Mataró M et al: Functional and magnetic resonance imaging correlates of corpus callosum in normal pressure hydrocephalus before and after shunting. J Neurol Neurosurg Psychiatry. 78(4):395-8, 2007
4. Hetts SW et al: Anomalies of the corpus callosum: an MR analysis of the phenotypic spectrum of associated malformations. AJR Am J Roentgenol. 187(5):1343-8, 2006
5. Rollins N: Semilobar holoprosencephaly seen with diffusion tensor imaging and fiber tracking. AJNR Am J Neuroradiol. 26(8):2148-52, 2005
6. Kinsman SL: White matter imaging in holoprosencephaly in children. Curr Opin Neurol. 17(2):115-9, 2004
7. Barkovich AJ et al: Callosal agenesis with cyst: a better understanding and new classification. Neurology. 56(2):220-7, 2001
8. Kier EL et al: The normal and abnormal genu of the corpus callosum: an evolutionary, embryologic, anatomic, and MR analysis. AJNR Am J Neuroradiol. 17(9):1631-41, 1996
9. Mendelsohn DB et al: Corpus callosum lesions after closed head injury in children: MRI, clinical features and outcome. Neuroradiology. 34(5):384-8, 1992
Image Gallery
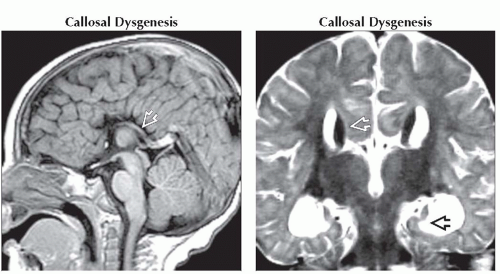 (Left) Sagittal T1WI MR shows callosal agenesis. Note radial array of paracentral gyri “pointing” to the 3rd ventricle as well as absence of identifiable cingulate gyrus. Hippocampal commissure is visualized posteriorly
 . (Right) Coronal T2WI MR shows the absence of crossing callosal fibers, the presence of Probst bundles . (Right) Coronal T2WI MR shows the absence of crossing callosal fibers, the presence of Probst bundles  , and vertical hippocampi , and vertical hippocampi  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|