Fig. 1.1
Epidemiology of acute coma in the intensive care unit (ICU). Panel a illustrates the estimated distribution of ICU admissions for acute coma after primary brain injury in industrialized countries. Panel b illustrates the estimated distribution of ICU admissions for acute coma after secondary brain injury. Critical illness-related encephalopathy (delirium) and prolonged sedation are important causes of coma in the ICU
Secondary, functional brain disorders are commonly encountered in the ICU (Fig. 1.1b). Critical illness-related acute brain dysfunction (also called critical illness-related encephalopathy or delirium) has recently emerged as a frequent complication in mechanically ventilated patients even without primary acute brain injury, who are admitted to the ICU for a variety of medical and surgical conditions, particularly following severe sepsis, multiorgan dysfunction, circulatory shock, and major cardiovascular surgery (Ely et al. 2004). In fact, septic encephalopathy is a major cause of secondary acute brain dysfunction (Sonneville et al. 2013); sedation is also associated with an increased risk of encephalopathy, particularly with prolonged use of benzodiazepines (Pandharipande et al. 2006). More importantly, and somewhat alarming, critical illness-related acute brain dysfunction is not only an independent factor of worse outcome (Girard et al. 2010), but has also recently been associated with long-term neurological sequelae and impaired cognitive function among ICU survivors (Pandharipande et al. 2013).
1.3 The Role of EEG in the ICU (See Also Chap. 2)
Electroencephalography monitoring (EEG) provides essential information about brain function, particularly in comatose patients, and is increasingly being used in the ICU (Claassen et al. 2013). Long-term EEG recording has become a fundamental part of the so-called brain multimodal monitoring, i.e., the constellation of invasive (intracranial pressure and brain oxygen monitors, cerebral microdialysis technique) and noninvasive (EEG, transcranial doppler, near-infrared spectroscopy) technologies that allow a comprehensive scrutiny of the injured brain and help optimize the management of comatose ICU patients (Oddo et al. 2012). In this setting, the role, potential utility, and present use of EEG in the ICU have greatly evolved over the last decade (Fig. 1.2). The predominant place of EEG in the ICU consists in diagnosing and helping manage convulsive and nonconvulsive seizures and SE in neurological and neurosurgical ICU patients (Friedman et al. 2009; Rossetti and Lowenstein 2011; Rossetti and Oddo 2010), as well as in medical (Oddo et al. 2009) and surgical (Kurtz et al. 2014) ICU patients with septic or other forms of acquired encephalopathy. Another well-recognized role of EEG is to guide the titration of several sedative agents (midazolam, propofol, barbiturates) that are commonly used for pharmacological coma (see Chap. 4) in patients with refractory SE or refractory intracranial hypertension. There are other emerging, promising roles for EEG monitoring in ICU patients. A prominent one, exploiting quantitative EEG analysis, is to use EEG to continuously monitor the brain function at the bedside in patients with primary acute brain injury, aiming to detect in a timely fashion secondary cerebral insults (e.g., ischemia, elevated intracranial pressure, nonconvulsive seizures) that are known to further aggravate patient outcome (see Chap. 5). In particular, quantitative EEG has shown great potential for the detection of delayed cerebral ischemia after SAH (Foreman and Claassen 2012). It may be conceivable that using EEG in this context may prevent secondary injury and improve outcome; however, further studies are needed to confirm this issue. Finally, EEG, together with other electrophysiological tools such as somatosensory and auditory evoked potentials (see Chap. 6), is increasingly used in combination with clinical examination, in order to better understand the mechanisms of acute coma and to further improve outcome prognostication after acute brain injury, particularly in patients with HIE after CA (Oddo and Rossetti 2011; Taccone et al. 2014).
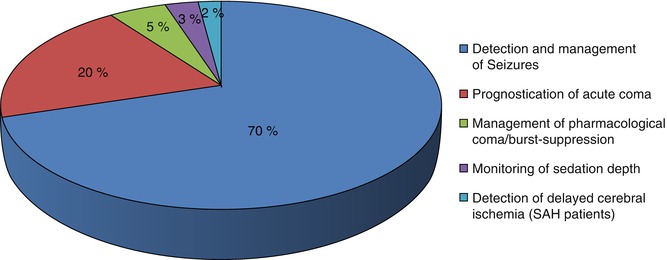
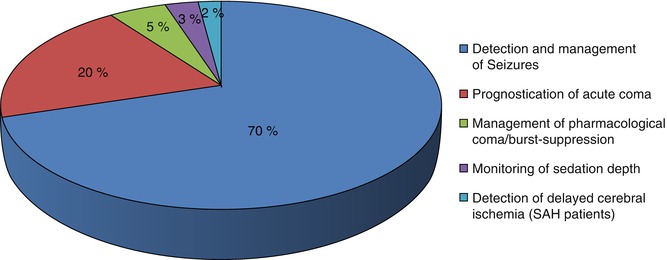
Fig. 1.2




Current indications and potential clinical utility of electrophysiological examinations in the ICU. EEG is primarily used to diagnose and manage seizures/status epilepticus. It has an emerging role and great potential in other conditions, mainly for the management of pharmacological coma, the monitoring of the depth of sedation in the mechanically ventilated patient, and as an additional noninvasive tool to detect secondary cerebral insults in acute brain injury patients, e.g., delayed ischemia after aneurysmal subarachnoid hemorrhage. Finally, EEG and evoked potentials have an important role in addition to clinical examination to improve coma prognostication, particularly after cardiac arrest
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







