23 | Acute Odontoid Fractures |
 | Case Presentation |
History and Physical Examination
A 46-year-old male was involved in a rollover car accident and taken via ambulance to the emergency department in a hard cervical collar. There was no loss of consciousness at the scene. He had several complaints, including neck, facial, and leg pain, in addition to shortness of breath. He also had multiple facial and head lacerations.
On physical exam, the patient had minimal tenderness with palpitation at the midline of the neck. There were no palpable step-offs or gross deformity. He had full motor strength in his bilateral upper and lower extremities. Sensation was intact to light touch in all dermatomal distributions. There were no long tract signs, and rectal examination revealed good sphincter tone.
Radiological Findings and Diagnosis
Radiographic evaluation showed a pneumothorax with multiple rib fractures and a closed tibia and fibula fracture. Facial radiographs demonstrated a mandible and orbital fracture. Computed tomographic (CT) scan of the head revealed a small subdural hematoma. Cervical spine series including an anteroposterior (AP) and cross-table lateral views were done, revealing no acute pathology. He remained in a rigid cervical collar and was emergently intubated secondary to pulmonary issues. The patient was transferred to our institution for management of the closed head injury. Our emergency department repeated the cervical spine x-rays, which included an AP, cross-table lateral, and open-mouth view, which showed a type II odontoid fracture. CT scan of the cervical spine revealed 4 mm of displacement and 15 degrees of anterior angulation (Fig. 23–1).
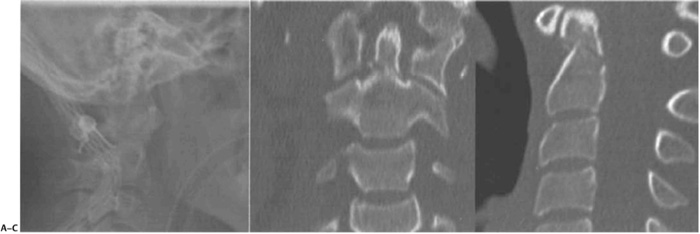
Figure 23–1 (A) Lateral radiograph. (B) Coronal computed tomographic (CT) section. (C) Sagittal CT section demonstrating a type II odontoid fracture.
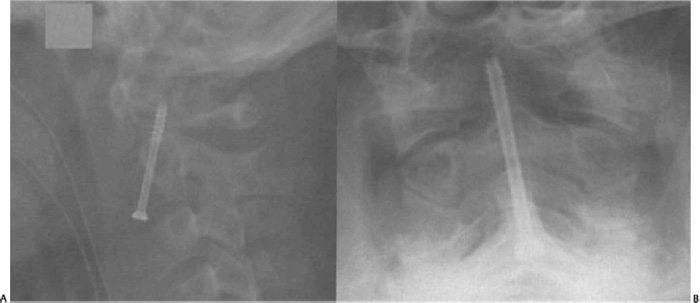
Figure 23–2 (A) Lateral radiograph and (B) anteroposterior radiograph postplacement of a single odontoid screw. Note the screw has no purchase in the tip of the dens where the dense cortical bone is found.
To stabilize the odontoid fracture, he was placed in a halo vest and transferred to the intensive care unit (ICU). After the patient was optimized for surgical intervention, he had a single anterior odontoid screw placed (Fig. 23–2). He did very well postoperatively until he had an acute onset of neck pain. Radiographs revealed the displacement of the odontoid fracture with screw migration (Fig. 23–3A). He was returned to the operating room where a posterior C1-2 fusion with iliac crest bone graft was performed in addition to removal of the anterior odontoid screw (Fig. 23–3B,C). He was placed in a rigid collar for 8 weeks and remained neurologically intact.
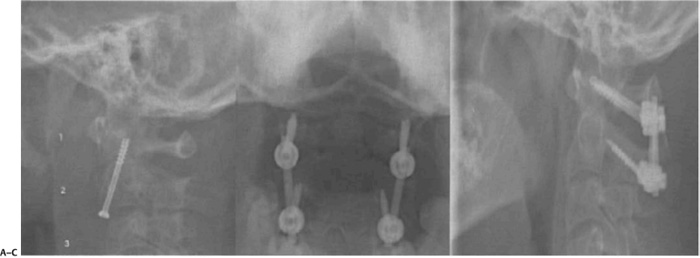
Figure 23–3 (A) Lateral radiograph demonstrating the displacement of the odontoid fracture with migration of the screw. AP (B) and lateral (C) radiographs showing a posterior cervical fusion with C1 lateral mass screws and C2 isthmic screws performed after failure of the odontoid screw.
 | Background |
In the adult population, odontoid fractures account for 9 to 15% of cervical spine fractures. This fracture typically occurs through the tip of the dens or its base or extends into the C2 body.1–3 Odontoid process fractures with neurological deficits occur in 10 to 20% of cases.4–7 Neurological sequelae, when present, are usually catastrophic or fatal due to the high level of spinal cord injury.
Odontoid fractures occur in various age groups in a bimodal distribution.8 These injuries result from low-energy impact such as falls in the elderly or high-energy impact such as motor vehicle accidents in the young population. Clinical signs range from isolated neck pain to quadriplegia with respiratory center involvement.
The majority of odontoid fractures are associated with high energy; therefore, it is not uncommon for the odontoid fracture to be initially undetected during the evaluation of more obvious injuries of the chest, abdomen, and other long bone fractures. Facial trauma and altered mental status may mask the symptoms of upper cervical injury and delay diagnosis. Head injury associated with odontoid fractures may be as high as 40% and complicates the initial assessment and treatment.
Symptomatic presentation may be limited even in the absence of altered mental status. Pain referred to the head and neck region is a common complaint. Numbness and paresthesia in the distribution of the greater occipital nerve, as well as posterior cervical muscle spasms, should lead to closer investigation. Neurological deficits may include quadriplegia, hemiparesis, or Brown-Séquard syndrome. Patients with posterior subluxation or displacement are at increased risk of cord injury, as well as higher rates of respiratory compromise.
The diagnosis of odontoid fractures relies on imaging evaluation. This employs the use of plain film, CT scan, and magnetic resonance imaging (MRI) modalities. Plain radiography remains the mainstay for identification of odontoid fractures. Radiographs should include three views of the cervical spine, including AP, cross-table lateral, and open-mouth odontoid views. The magnitude and direction of displacement should also be noted. Oblique views can provide additional information but are not mandatory. Flexion and extension views can be used to evaluate the stability of chronic odontoid injuries.
Furthermore, concomitant injuries to the remainder of the spine should be thoroughly investigated. Recent studies reveal that there is a 34% risk of noncontiguous spine fractures. Plain radiographs can be done of the thoracic and lumbar spine; however, most trauma patients have CT scans of the chest/abdomen/pelvis, which can be reformatted to evaluate for spine fractures.
A CT scan is performed if a bony injury is identified on plain films, a fracture is suspected, or the patient has an altered mental status. Sagittal and coronal reformats are important to characterize the plane of the fracture line as well as the degree of comminution. In many institutions, trauma patients with a suspected cervical spine injury have an initial CT scan, negating the need for plain films.
MRI has a more limited role in evaluating patients who have sustained an odontoid fracture. MRI should be done if there is a neurological deficit or a suspected ligamentous injury. MRI may demonstrate the disruption of the transverse ligament, particularly using the multiplanar gradient echo modalities.
There have been several classifications described for odontoid fractures. In 1974, Anderson and D’Alonzo2 classified these fractures on an anatomical level, which was correlated to fracture union. Type I fracture is an oblique fracture through the upper part of the odontoid process. These are rare fractures, accounting for less than 5% of all odontoid fracture types. This fracture pattern is usually stable. However, it is occasionally associated with gross instability due to injury to the apical and/or alar ligaments resulting in occipital-cervical dislocation. Type II fractures occur at the junction of the base of the odontoid and body of the axis. They are the most common and problematic fracture type, resulting in a high pseudarthrosis rate.11 Type III fractures extend into the body of the axis (Fig. 23–4A). They may be more stable than type II fractures and have a higher union rate with nonsurgical treatment.
In 2005, Grauer et al12 attempted to modify the Anderson and D’Alonzo classification of odontoid fractures based on current treatment options. The modified classification system more precisely distinguishes between various type II fractures. Subtype A are transverse type II fractures without comminution and less than 1 mm displacement. Subtype B are oblique fractures passing from anterior-superior to posterior-inferior with displacement greater than 1 mm. Subtype C are also oblique fractures, but instead pass from anterior-inferior to posterior-superior with significant comminution (Fig. 23–4B).
The mechanism responsible for odontoid fractures is usually hyperextension or hyperflexion of the cervical spine. However, recent finite element models illustrate a more complex mechanism.9 The application of either or both extension and axial rotation by force vector placement caused the greatest risk of odontoid fracture. Force loading that placed the cervical spine in extension coupled with lateral shear or compression led to type I fracture, whereas axial rotation and lateral shear produced type II fractures. The exact mechanism for type III fractures remains unclear; however, it involves a flexion moment through the occiput.
There are many types of odontoid fractures, as noted in the various classification schemes. Issues such as fracture type, degree of initial displacement, extent of angulation, ligamentous injury, fracture healing, neurological function, and the age of the patient must be addressed. Each of these variables can alter the treatment decision-making process. Treatment options include a rigid cervical collar, halo vest immobilization, odontoid screw fixation, and posterior atlantoaxial arthrodesis.
 | Authors’ Preferred Method of Management |
Type I fractures are quite uncommon; therefore, it is difficult to compare the various treatment methods. Clinically these injuries are often incidental and not associated with instability. Generally, type I odontoid fractures are treated with collar immobilization for 6 to 8 weeks for symptomatic relief. Even if union does not occur, the clinical results are usually satisfactory and the patient asymptomatic. In some cases, a type I fracture is a sign of greater craniocervical instability. In occipitocervical dislocation, a posterior fusion is performed from the occiput to the axis. This construct may need to be extended further based on the fracture pattern.
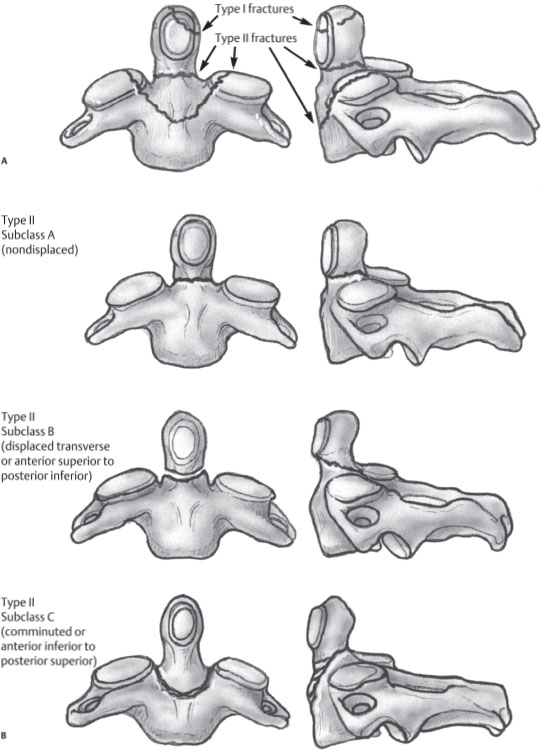
Figure 23–4 (A) Anderson and D’Alonzo classification. (B) Proposed modification of type II odontoid fractures, including type IIA, IIB, and IIC



