7 | Adjacent Level Degeneration |
 | Case Presentation |
History and Physical Examination
S.M. is a 49-year-old male who initially presented 17 years ago with complaints of persistent neck and right arm pain. He was diagnosed with a herniated nucleus pulposus at the C5-6 level and subsequently underwent anterior cervical diskectomy and interbody fusion. Postoperatively the patient did very well for ~10 years until he presented again with symptoms of left arm pain and gait imbalance. Imaging studies at that time revealed degenerative changes proximal to his previous arthrodesis indicative of a diagnosis of cervical spondylotic myeloradiculopathy, which was treated with C4 corpectomy and C3-5 anterior cervical fusion. The patient experienced complete resolution of his radicular and myelopathic complaints following surgery and remained symptom-free for another 5 years after his second operation.
Five years later, the patient developed new symptoms of right arm discomfort in a distribution different from the pain that he had experienced prior to his first two surgeries; in addition, he also noted subtle changes in his dexterity apparent only when he played the piano. Physical exam findings included a positive Spurling sign, weakness in his right triceps and wrist extensor muscles as well as diffuse hyperreflexia and positive Hoffmann signs bilaterally.
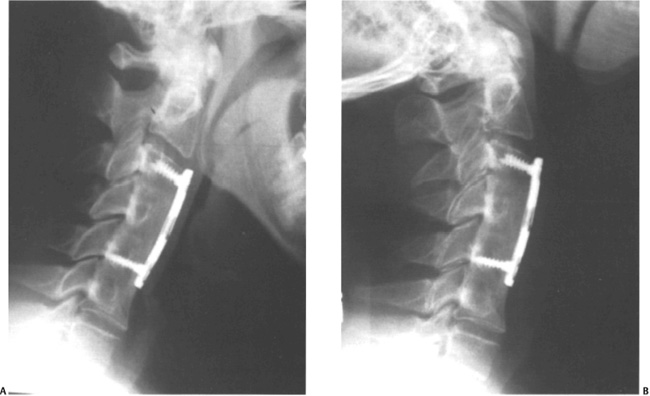
Figure 7–1 (A) Flexion lateral radiograph. (B) Extension lateral radiograph.
Radiological Findings and Diagnosis
Plain radiographs of the cervical spine demonstrated a solid fusion from C3 to C6 with no motion on flexion-extension lateral films (Fig. 7–1). Magnetic resonance imaging (MRI) of the cervical spine revealed a new right paramedian disk herniation at the C6-7 level resulting in compression of both the spinal cord and the right C7 nerve root, representing a second occurrence of adjacent segment disease of the cervical spine after two successful operations to treat myeloradiculopathy (Fig. 7–2). Because his symptoms were refractory to multiple nonoperative treatments such as antiinflammatory medications and cervical traction, the patient elected to proceed with anterior cervical decompression consisting of a C6-7 diskectomy followed by fusion with iliac crest allograft and anterior plating (Fig. 7–3).

Figure 7–2 T2-weighted sagittal magnetic resonance imaging demonstrating a disk herniation at the C6-7 level.

Figure 7–3 Postoperative lateral radiograph following anterior cervical diskectomy and fusion of C6-7.
 | Background |
Over the past several decades anterior cervical decompression and fusion has proven to be a reliable treatment for a myriad of pathological conditions, including trauma, deformity, infection, tumor, and arthritis. Based upon the favorable long-term results reported in multiple longitudinal studies, anterior cervical decompression and fusion procedures have become the standard of care for the management of cervical myelopathy and radiculopathy.1,2 Having gained wider acceptance among surgeons, spinal fusions are increasingly being performed in younger patients at rates that continue to escalate, generating concerns about the ongoing consequences of this procedure.3 In particular, there has been considerable interest in the long-term survival of the spinal motion segments adjacent to these fusion constructs. Adjacent segment degeneration describes the radiographic deterioration of the motion segments adjacent to a preexisting arthrodesis, which may not necessarily correspond with a patient’s symptoms.4 In contrast, adjacent segment disease refers to the development of clinically significant findings that positively correlate with the degenerative changes adjacent to a prior fusion that are evident on imaging studies.
Numerous retrospective reviews of patients who had undergone anterior cervical fusion (ACF) have reported relatively high rates of postoperative radiographic degeneration.5–9 Baba et al observed progressive spinal stenosis in 25% of patients who had been treated with ACF for spondylotic myeloradiculopathy at an average of 8.5 years after their index procedures.10 In their report of 180 patients who presented with a variety of different pathological diagnoses that were all addressed with ACF, Goffin et al determined that the incidence of adjacent radiographic degeneration was 92% at a minimum of 5 years’ follow-up; however, the reoperation rate for symptomatic disease was limited to just 6% of these cases.11 Gore and Sepic also examined the 5-year results of 146 individuals with a history of previous anterior cervical diskectomy and fusion (ACDF) surgery in which they noted new spondylosis in 25% and worsening of preexisting degenerative changes in another 25%.12 Despite an incidence of progressive spondylosis approaching 50%, only 14% required additional surgery for clinically significant disease. When this same population was followed for an average of 21 years postoperatively, 98% were found to have developed some radiographic evidence of adjacent level degeneration, although once again the vast majority of these patients did not require any further surgery.13 Ishihara et al identified adjacent segment disease in 19% of 112 subjects evaluated at least 2 years after ACDF.14 In the series of Bohlman et al, 9% of 122 ACDF patients followed for an average of 6 years developed symptomatic disease necessitating further surgical intervention.1 Although progressive degeneration was frequently detected at the levels adjacent to a cervical fusion, these studies do not establish a clear correlation between these radiographic abnormalities and the development of symptoms referable to these changes, nor do they establish any relevant association between adjacent segment degeneration and the long-term outcomes following ACF.
 | Etiology |
The pathophysiological processes underlying postarthrodesis adjacent segment degeneration have not been well characterized and its etiology remains a matter of extensive debate. There are ample data to suggest that adjacent level degeneration may be a direct effect of the altered biomechanical environment that is present following a cervical fusion. Multiple studies employing either radiography,10,15 fluoroscopy,16 or biomechanical testing17 have demonstrated compensatory increases in motion immediately above and below an arthrodesis. The presence of heightened stresses and strains in the motion segments in close proximity to a fusion construct has been confirmed using flexion-extension x-rays,9 human cadaveric specimens,18 and finite element analysis.19 Likewise, the in-tradiskal pressures at the levels adjacent to a cervical fusion were recently shown to be elevated in an in vitro biomechanical study.20 Kyphotic malalignment after ACF may also serve to accelerate this junctional deterioration by transmitting even more substantial forces on the neighboring intervertebral levels.21,22 These pathological changes are thought to give rise to cervical instability and facilitate the transfer of excessive loads to the unfused segments, placing them at greater risk for failure even under normal physiological conditions. This potential relationship between ACF and subsequent spondylotic degeneration is supported by the results of similar retrospective reviews assessing the long-term outcomes of patients with Klippel-Feil syndrome and cervical block vertebrae,23,24 as well as children who underwent cervical arthrodesis for traumatic instability.25 At the time of final follow-up, the majority of these subjects also exhibited significant radiographic degeneration or hypermobility adjacent to the fused levels. In addition to these biomechanical considerations, it is possible that a variety of genetic and biological factors, acting either locally at the fusion site or more systemically, may play a role in the formation of these degenerative changes.
Previous investigations have demonstrated that cervical spondylosis is a virtually inevitable consequence of the normal aging process, although it frequently exists in the absence of clinical findings. By the age of 50 years approximately half of all adults will exhibit some evidence of cervical degeneration on plain radiographs.26 In an asymptomatic population greater than 40 years of age, Boden et al determined the prevalence of spondylotic changes on MRI scans of the cervical spine to be nearly 60%.27 Given the ubiquitous nature of cervical spondylosis, it is conceivable that the deterioration of levels adjacent to a spinal fusion may not be influenced by the iatrogenic mechanical stresses that are produced by the rigid motion segment but may instead represent the natural history of the underlying degenerative disease. According to this mechanism, adjacent segment degeneration arises largely as a result of progressive cervical spondylosis and any deleterious effects of an arthrodesis on adjacent levels are of less importance than the degeneration that is typically seen in the aging spine.
In support of this premise, several in vivo clinical studies have failed to detect any disproportionate increases in motion at the segments adjacent to a cervical fusion.28–30 Using dynamic fluoroscopic imaging, Reitman et al also did not discover any significant disparities in pre- and postoperative junctional intervertebral motion in individuals who had been treated with ACDF.31 Gore et al evaluated the lateral x-rays of both ACF patients as well as age- and sex-matched controls with no history of cervical complaints and identified no difference in the incidence of spondylosis between the two populations.32 The degeneration of adjacent segments has been shown to occur more frequently when ACF is used to address a diagnosis of spondylosis than when arthrodesis is performed for other conditions such as trauma, tumor, or infection.8,33 These studies suggest that the establishment of adjacent segment degeneration may be more dependent upon any preexisting degeneration that is already present at adjacent spinal levels than it is on any alterations in the biomechanical environment that were brought on by the fusion. Based upon this hypothesis, patients who have symptomatic spondylotic disease requiring surgery would be more likely to harbor subclinical disease at adjoining motion segments that may continue to progress over time.
Several authors have also compared the radiographic outcomes of ACF and nonfusion procedures to determine whether the arthrodesis itself is primarily responsible for accelerating the formation of degenerative changes. Lunsford et al noted equivalent rates of adjacent segment disease among subjects undergoing ACDF for cervical disk herniations and others managed with diskectomy alone.34 The prevalence and average annual incidence of adjacent level disease in a series of 846 consecutive cases of cervical radiculopathy treated with posterolateral foraminotomy were found to be similar to those reported after ACF.35 In another study the incidence of adjacent segment degeneration associated with ACDF was actually lower than that observed following posterior decompression without fusion (41% vs 50%, respectively).36
The most extensive investigation of adjacent segment disease was published by Hilibrand et al, who defined the incidence, prevalence, and natural history of this disorder in their long-term retrospective review of 374 consecutive patients who underwent 409 anterior cervical decompression and stabilization procedures for spondylotic radiculopathy or myelopathy.37 In this study the overall prevalence of adjacent level disease requiring further surgical intervention was 14.2% over 2- to 21-year follow-up with a relatively constant annual incidence of 2.9% during the 10 years after the index operation. Kaplan-Meier survivorship analysis estimated that 13.6% of all patients undergoing ACF would develop new symptomatic cervical disease correlating to a degenerated segment adjacent to the previous arthrodesis within 5 years, and at 10 years the predicted prevalence of clinically significant disease increased to 25.6%. The authors also identified various risk factors for the development of adjacent segment disease, including preexisting deterioration of adjacent levels at the time of ACF; fusions adjacent to the C5-6 or C6-7 levels, the most mobile segments of the cervical spine, which are predisposed to arthritic changes38; and single-level procedures, which may not have adequately addressed any advanced spondylotic disease that was already present at other levels prior to surgery. Collectively, these results indicate that rather than being a direct complication of an arthrodesis, adjacent segment degeneration may instead simply reflect the normal progression of cervical spondylosis.
 | Nonoperative Management |
In the absence of frank myelopathic signs and symptoms, nonoperative modalities such as antiinflammatory medications, physical therapy, and cervical traction may be utilized as part of the initial treatment of symptomatic adjacent level disease. In one retrospective cohort study of 122 subjects who were diagnosed with adjacent segment disease following ACDF, 63% improved with the use of non-surgical methods and did not require subsequent operative intervention.14 Because only 28% of the patients in their series responded appropriately to conservative therapies, Hilibrand et al concluded that nonoperative management may be less effective for the treatment of symptomatic adjacent level disease than it is for other cervical pathology.37 Fortunately, the majority of this group who failed these conservative measures experienced excellent resolution of their symptoms following surgical intervention.
Surgical Management
The principles of surgical treatment are the same for adjacent level disease as they are for any degenerative condition—namely, to decompress the neural elements while providing spinal stability. However, the abnormal biomechanical forces that are thought to be generated across the fused segment raise the concern that standard operative approaches may be less effective for adjacent segment disease than they are for primary cervical spondylosis. Hilibrand et al published the radiographic and clinical results of different anterior cervical decompression and fusion procedures that were performed for symptomatic adjacent level disease.39 Among those who underwent anterior diskectomy and interbody grafting with tricortical autograft, the rate of arthrodesis as confirmed by flexionextension lateral x-rays was only 62.5%, irrespective of the number of levels that were addressed. In contrast, all of the patients who were treated with corpectomy and autogenous strut grafting were found to have successfully healed. The authors attributed this superior fusion rate to the increased bony contact area afforded by strut grafting compared with the use of smaller ACDF grafts as well as the requirement of bone formation across only two surfaces instead of the four or six that are involved in multilevel ACDF constructs. Although there were no significant differences in the clinical results between these two groups, patient outcomes were significantly better among individuals who achieved a solid arthrodesis. It should be noted that none of these procedures was augmented with anterior cervical plating. The current authors advocate the use of internal fixation to increase fusion rates.
Alternatively, adjacent segment disease may also be managed using a posterior approach to the cervical spine. Nonfusion strategies, including cervical laminectomy and laminoplasty, allow for the preservation of motion and avoid the hazards inherent to revision anterior surgery; laminoforaminotomy may also be indicated in patients with symptomatic disease who present with complaints consistent with a unilateral radiculopathy secondary to lateral disk herniations or osteophyte formation.40 However, posterior decompression alone must be performed judiciously because of the risk of developing progressive postoperative kyphosis, especially in those who already demonstrate some degree of deformity in the sagittal plane preoperatively.41,42 Although posterior cervical decompression and fusion may be appropriate for spondylotic disease affecting several adjacent spinal segments, there are no long-term studies evaluating its efficacy for the treatment of adjacent level disease.
 | Authors’ Preferred Method of Surgical Management |
Before proposing any form of operative intervention it is critical to establish whether the patient’s complaints are the result of new spondylotic disease at the levels adjacent to the previous arthrodesis or whether they represent recurrent symptoms related to inadequately treated pathology, the presence of a pseudarthrosis, or chronic nerve pain. In some cases it may be difficult to differentiate between these clinical scenarios, such as with a patient who has had residual neurological deficits that never resolved despite undergoing successful cervical decompression and fusion. In these situations a detailed history and thorough physical examination are necessary to characterize the distribution and temporal onset of the patient’s current symptoms, and these findings should be corroborated with relevant imaging studies.
Once adjacent segment disease has been identified as the primary pathological process responsible for the patient’s symptoms, the formation of a reasonable surgical plan in conjunction with the adherence to proper intraoperative techniques will serve to enhance the clinical outcomes and minimize the incidence of complications. Aside from certain individuals with severe stenosis spanning several levels who may be candidates for posterior cervical decompression and fusion, we generally treat symptomatic adjacent segment disease through an anterior approach. Although we consider ACDF to be a viable option for addressing compression at one, two, or three adjacent segments, the results of our previous investigations suggest that corpectomy with strut grafting may be preferable for the management of multilevel disease.39,43 At this time we employ internal fixation in virtually all ACF cases and will sometimes use allogenic bone graft in conjunction with anterior cervical plating, except in smokers or those with other medical comorbidities that may reduce the likelihood of its successful incorporation.
Pearls
The current literature regarding adjacent level disease clearly supports the treatment of all degenerated segments that correlate with the clinical symptoms in question. In addition, from what is known about the natural history of this condition we believe that any levels that demonstrate abnormal motion on dynamic lateral radiographs or exhibit evidence of neural element compression on MRI should also be included within the ACF to improve postoperative outcomes.44 If the decision is made to exclude an adjacent segment with only a moderate degree of involvement from the surgical procedure, patients should be counseled that they have an ~25% chance of developing progressive spondylosis leading to symptomatic disease at that or another level during the first 10 years after their original cervical arthrodesis.37
All patients undergoing surgery for adjacent level disease are referred to an ear, nose, and throat specialist for examination of the vocal cords. If there is any evidence of paralysis or any other abnormalities, a revision approach using the previous incision is indicated to preserve vocal cord function on the unaffected side. If the vocal cords are normal, a surgeon may prefer to place the incision on the contralateral side to avoid the challenges associated with a revision approach through scar tissue. During the exposure of the anterior cervical spine, it is good practice to avoid any damage to the intervertebral disks, the anterior longitudinal ligament, and the longus colli muscles at the levels in close proximity to an ACF because it has been reported that iatrogenic injury to these structures may contribute to the progression of spondylotic degeneration at those levels.8 Intraoperatively the surgeon should also strive to maintain or restore acceptable cervical lordosis to minimize the transfer of mechanical stresses to adjacent spinal segments and theoretically limit any further deterioration.21,22 Finally, in situations where the newly degenerated level is located in the cervicothoracic region, which is subject to substantial junctional forces, it may be prudent to include additional segments anteriorly or even supplement the ACF with posterior fixation in an attempt to reduce the incidence of graft or hardware failure.



