Alcohol dependence II
Assessment
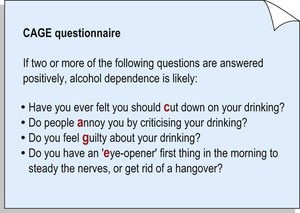
All patients should be asked about their alcohol consumption, and specific quantities recorded. Vague responses, such as ‘I only drink socially’, are not acceptable; many alcoholics consider themselves to be very sociable drinkers. As alcohol consumption varies for most people, it is usually easiest to enquire about a typical week and calculate the number of units consumed. Remember that measures poured at home are usually larger than the standard measures provided in bars. The pattern of alcohol consumption is important. Alcoholics typically have a rigid pattern, with regular consumption throughout the day, beginning with an early morning drink to alleviate withdrawal symptoms. The CAGE questionnaire is commonly used as a quick screening tool for alcohol dependence (Fig. 1).
Treatment
Withdrawal from alcohol
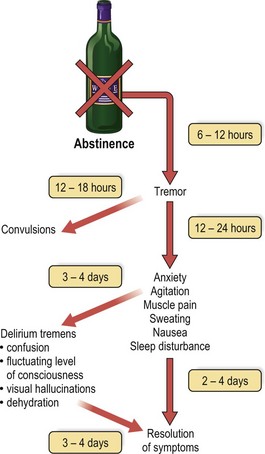
Many withdrawals are not planned and happen after a period of enforced abstinence from alcohol. This may occur following admission to hospital and should always be considered in a patient who becomes tremulous or confused within a few days of admission. Symptoms of the withdrawal syndrome are summarised in Figure 2. They are usually treated with benzodiazepines (e.g. chlordiazepoxide) which, like alcohol, increase the activity of the neurotransmitter GABA. The drug is given in sufficient doses to control the symptoms, and the dose is then gradually reduced and stopped over the course of a week, by which time the symptoms will have resolved. Parenteral thiamine should be given to all patients to prevent Wernicke’s encephalopathy. Detoxification should be offered to all alcoholics expressing a wish to stop drinking, including those who have been through this process many times in the past.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree