Alpha Activity
▲ Alpha Rhythm
Other Names
Occipital alpha rhythm
Posterior dominant rhythm
Posterior basic rhythm
Types
Alpha squeak
Squeak effect
Description
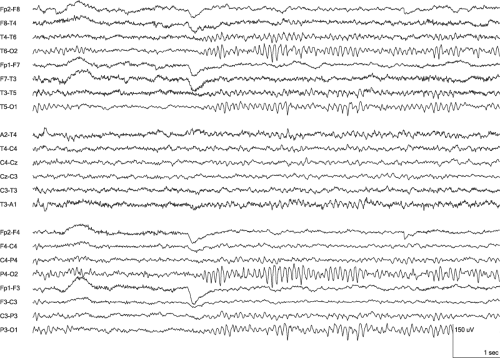
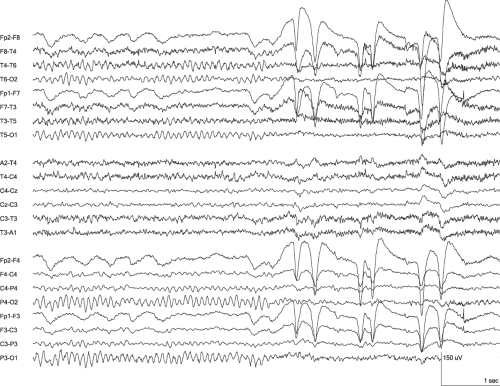
With Hans Berger’s 1929 publication on what would be called the human electroencephalogram, the alpha rhythm was the first EEG pattern to be named (Berger, 1929). This pattern continues to be the most commonly noted rhythm in clinical EEG interpretation presumably for the same reason Berger identified it, because it is commonly present and easily recognized. According to the International Federation of Clinical Neurophysiology (IFCN) definition, the alpha rhythm has a frequency of 8 to 13 Hz and is present over the posterior head regions in a state of relaxed wakefulness with the eyes closed (Chatrian et al., 1974; Noachtar et al.,1999). It attenuates or disappears with drowsiness, concentration, stimulation, or visual fixation, and the abrupt loss of the alpha rhythm because of visual or cognitive activity is termed blocking. The alpha rhythm may be present with the eyes opened if the environment is devoid of light or visual fixation is not present. In particular, drowsy individuals who awaken and open their eyes without immediate visual fixation may have a paradoxical alpha rhythm because the rhythm is absent with eyes closed due to drowsiness and briefly present with eyes opened due to lack of full visual alertness (Fisch, 1999; Niedermeyer, 1999c). This most commonly occurs in the context of sedation (Erwin et al., 1984). The extent of the alpha rhythm’s blocking varies among individuals and, along with its amplitude and persistence of each run of activity, tends to decrease with aging (Fisch, 1999). The complete absence of blocking with either visual fixation or concentration is abnormal (Blume et al., 2002; Kiloh et al., 1981; Westmoreland and Klass, 1998). Unilateral blocking also is abnormal and is termed Bancaud’s phenomenon (Bancaud et al., 1955). In such instances, the side lacking the blocking response is abnormal.
The alpha rhythm’s amplitude varies among individuals and usually is between 40 and 50 μV in adults. Overall, children have higher amplitude alpha rhythms (Niedermeyer, 1999b). An amplitude greater than 60 μV occurs in only 6% of adults, and an amplitude greater than 100 μV is exceedingly rare (Niedermeyer, 1999c). Adults commonly have a lower amplitude, and 30% having an amplitude less than 20 μV. An amplitude between 5 and 10 μV is not rare, and the alpha rhythm is not present in up to 10% of healthy individuals (Kellaway, 1990; Kiloh et al., 1981). The absence of an alpha rhythm may be genetic and can be transmitted with autosomal dominant inheritance (Anokhin et al., 1992). Blindness that has been present since early life is another cause for the absence of an alpha rhythm; however, such blindness also can produce an alpha rhythm that occurs inconsistently, extends over a smaller distribution, or has a parietal distribution (Birbaumer, 1970; Cohen et al., 1961; Hari, 1999; Jan and Wong, 1988; Jeavons, 1964). When the alpha rhythm is absent because of blindness, the EEG is similar to a sighted person with eyes opened. Because of the alpha rhythm’s large and uniform field, its amplitude is most accurately measured with a referential montage. Shorter interelectrode distances may result in an appearance of low amplitude due to the differential amplification.
The alpha rhythm’s waveform usually is sinusoidal but may be arciform due to a sharply contoured negative component. Regardless of the waveform for the individual waves, the rhythm occurs as spindles with individual wave amplitudes that build and fall over periods of about 1 second. This spindle pattern is due to superimposition of two frequencies, which also produces the arciform appearance if one of the frequencies is in the beta frequency range (Blume et al., 2002). The frequency of the waves within the spindle’s packet typically is 9 to 10 Hz in healthy adolescents and adults. During childhood, a rhythm is present that is similar to the alpha rhythm in its location and reactivity but has a frequency below the alpha frequency range. Since it is not alpha activity, it is better termed the posterior
dominant rhythm (PDR); however, it commonly is referred to as the alpha rhythm because of its resemblance in others’ feature and its equivalent clinical significance. Similarly, the alpha rhythm in adults may be referred to as the PDR, especially when it is abnormally slow.
dominant rhythm (PDR); however, it commonly is referred to as the alpha rhythm because of its resemblance in others’ feature and its equivalent clinical significance. Similarly, the alpha rhythm in adults may be referred to as the PDR, especially when it is abnormally slow.
The PDR first develops at 3 or 4 months after full-term birth in 75% of infants and it has a frequency of 4 Hz at this age, but the rhythm’s activity often is not sustained (Kellaway, 1990; Niedermeyer, 1999c). By 1 year, its frequency is 5 to 6 Hz in 70% of children. By 3 years, 80% have a true alpha rhythm because the PDR has reached a frequency of 8 Hz. By 9 years, 65% have a frequency of 9 Hz, and by 15 years, 65% have a frequency of 10 Hz (Fisch, 1999; Kellaway, 1990). The alpha rhythm’s frequency in early childhood is highly variable with frequencies between 5 and 10 Hz commonly occurring during the second year (Niedermeyer, 1999b). Frequencies less than 8.5 Hz are abnormal in adults regardless of age (Markand, 1990). The alpha rhythm’s frequency commonly declines by 1 Hz through adulthood, but a decrease below 8.5 Hz is a sign of cerebral dysfunction even in centenarians (Hubbard et al., 1976; Shigeta et al., 1995; Torres et al., 1983). Frequency determination should not include the first 0.5 to 1 second after eye closure because this period may have a brief, higher frequency, which is termed alpha squeak or the squeak effect (Storm van Leeuwen and Bekkering, 1958). The alpha rhythm’s frequency remains stable after this initial, brief period.
The alpha rhythm’s frequency may occur as two normal variants: The slow alpha variant and the fast alpha variant. Both of the variants have the same location and reactivity as the alpha rhythm (Fisch, 1999), (Blume et al., 2002). The slow alpha variant is a subharmonic of the alpha rhythm that may be due to a fusion of adjacent waves (Blume et al., 2002). Its frequency usually is 4 to 5 Hz, that is, it is half of the alpha rhythm frequency present at other times in the same EEG. The waves within the slow alpha variant may or may not have a small bifurcation at the wave’s peak indicating the two component waves that constitute the normal alpha rhythm frequency (Kellaway, 1990; Niedermeyer, 1999b). The slow alpha variant typically does not occur before the age of 8 years, and it is present in approximately 1% of normal EEGs (Aird and Gastaut, 1959; Fisch, 1999; Jabbari et al., 2000). The fast alpha variant is a harmonic of the alpha rhythm and usually has a frequency between 16 and 20 Hz (Fisch, 1999). It also may have a waveform with bifurcated waves, but the bifurcation for the fast alpha variant is at the peaks of the waves in the normal alpha rhythm. Both variants occur as brief repetitions amid the typical alpha rhythm or, occasionally, in place of it.
The alpha rhythm’s distribution always includes the occiput and commonly extends to include the posterior temporal and occipital parietal regions. This extension should be symmetric, and asymmetry can indicate abnormality on the side with a larger field. The normal frequency asymmetry between the sides is less than 1 Hz (Kiloh et al., 1981). Frequency asymmetries greater than 1 Hz are due to the superimposition or admixture of slower activity; thus, the side with the lower frequency is abnormal (Blume et al., 2002).
Asymmetric alpha rhythm amplitude is present for 60% of individuals, but this asymmetry rarely is greater than 20 μV. About 80% of those who have an asymmetry have greater amplitude on the right side (Dietlein et al., 1965). This asymmetry is not related to handedness and conventionally has been ascribed to asymmetry in the skull’s thickness, but an analysis that used MRI measurements of skull thickness did not find this to be an explanation for the asymmetry (Hagemann et al., 2008). When the right side has a higher amplitude, the asymmetry is abnormal when the left is less than 50% of the right (Blume et al., 2002; Fisch, 1999; Kiloh et al., 1981; Niedermeyer, 1999b). Only 1.5% of those with amplitude asymmetry have more than this 50% of the right side difference between the sides. Since greater amplitude on the left side is much less common, the maximum allowable asymmetry is for the right to be less than 67% of the left (Kellaway, 1990), that is, the left should not be greater than 150% of the right. As with all amplitude measurements for the alpha rhythm, determination of symmetry should use a referential montage (Blume et al., 2002). When the amplitude asymmetry is greater than standard normal limits and it is not caused by a breach effect, the side of lower amplitude usually is abnormal side. Occasionally, a space-occupying lesion within the occiput may produce an abnormal increase in the ipsilateral alpha rhythm amplitude.
During drowsiness, the alpha rhythm disappears with a transition that includes a decrease in amplitude, extension of the field anteriorly, a loss of clearly sinusoidal or arceau waveform, and inclusion of more theta frequency range activity (Blume et al., 2002; Santamaria and Chiappa, 1987). Eventually, the rhythm’s predominant frequency decreases to the theta frequency range (Niedermeyer, 1999d). The anterior extension may reach the central and midtemporal regions and becomes frontal in rare instances (Fisch, 1999).
Distinguishing Features
• Compared to Generalized Alpha Activity
In drowsiness, the alpha rhythm may resemble generalized alpha activity because of its extension into the temporal and frontal–central regions; however, it remains distinguishable by its occipital predominance, the brief or unsustained extension of the field to a broad distribution, and its reactivity to visual fixation.
• Compared to Phi Rhythm
The phi rhythm is a brief, paroxysmal, bisynchronous, occipital delta rhythm that occurs within 2 seconds of eye closure and lasts 1 to 3 seconds (Belsh et al., 1983).
Because of these features, it has similarity to the slow alpha variant. It differs from the alpha rhythm because of its consistent occurrence only immediately after eye closure and its absence during periods of sustained eye closure. The slow alpha variant typically occurs throughout the time that the alpha rhythm is present without correspondence to the timing of eye closure.
Because of these features, it has similarity to the slow alpha variant. It differs from the alpha rhythm because of its consistent occurrence only immediately after eye closure and its absence during periods of sustained eye closure. The slow alpha variant typically occurs throughout the time that the alpha rhythm is present without correspondence to the timing of eye closure.
Co-occurring Patterns
The alpha rhythm is present only in wakefulness; thus, it is always accompanied by other EEG signs of wakefulness. This includes both eye blink artifact and muscle artifact; however, the alpha rhythm is absent in wakefulness when blinks are frequent, which indicates that the eyes are open, and when muscle artifact is considerable, which indicates a relaxed state is not present. Other alpha activity may accompany the alpha rhythm, which includes both the mu rhythm and the wicket rhythm. Generalized and frontal–central beta activity and rhythmic midtemporal theta (RMT) activity sometimes also co-occurs, depending on the patient’s level of alertness. Lambda waves also occur during wakefulness and have an occipital distribution. However, they occur when the eyes are open and are therefore independent to the alpha rhythm (Niedermeyer, 1999c).
Clinical Significance
The alpha rhythm is a normal pattern that likely is due to rhythmic cellular interactions between occipital and some parietal cortex and the pulvinar nuclei of the thalamus (Basar et al., 1997; Ciulla et al., 1999; Goldman et al., 2002; Lopes da Silva, 1991; Lopes da Silva et al., 1974; Sadato et al., 1998). Its function likely relates to gated levels of visual attention, perhaps as an active stand-by state (Foxe et al., 1998). Within individuals who are adolescent or older, its frequency is highly reproducible among EEG recordings of the same state. Since drowsiness increases the slowing within the alpha rhythm, determination of whether the EEG includes the maximal wakeful state is important in determining whether abnormal slowing is present. Thus, a consistently slow alpha rhythm within an EEG that does not include the best possible awake state should not be interpreted as abnormal. Notation from the recording technologist describing the observed behavioral state and responses to stimulation are the preferred source of waking state information, but observing movement and ocular artifact also is helpful.
Apparent slowing of the alpha rhythm with inclusion of greater theta activity commonly occurs with encephalopathy, regardless of whether the condition is reversible. Therefore, an alpha rhythm below the alpha frequency range (better termed a PDR) in the best waking state is a nonspecific finding that may indicate either posterior or generalized cerebral dysfunction. The sensitivity of alpha rhythm slowing varies across causes and diseases. The alpha rhythm is normal in Alzheimer’s disease in its early stages, and, in contrast, abnormal changes to the alpha rhythm may be caused by cerebral hypoperfusion in the absence of encephalopathy (Chan et al., 2004; Kellaway, 1990). Improving cardiac output can reverse asymptomatic, abnormal slowing of the alpha rhythm by up to 2 Hz. Fever and hypermetabolic states, including hyperthyroidism and amphetamine intoxication, may increase the alpha rhythm’s frequency (Niedermeyer, 1999c; Strauss et al., 1952). In contrast to adults, high fever in children may increase or decrease the frequency (Fisch, 1999). Hypothyroidism and antiepileptic medications may produce an asymptomatic and minor decrease in the alpha rhythm’s frequency (Salinsky et al., 2002). Marijuana also may produce an increase or a decrease in the alpha rhythm frequency, and this may depend on the psychological effect of the drug on the individual (Strauss et al., 1952).
Failure of the alpha rhythm to block either unilaterally (Bancaud’s phenomenon) or bilaterally usually is due to a structural abnormality but also may occur transiently with migraines or transient ischemic attacks (Westmoreland and Klass, 1990). When unilateral blocking is present, the pathology is ipsilateral to the side that fails to block and usually within occipital lobe or its subcortical gray matter connections (Fisch, 1999). However, it sometimes occurs with lesions of the parietal or temporal lobes (Westmoreland and Klass, 1990). The absence of blocking bilaterally may be due to an occipital or a pontine lesion (Loeb and Poggio, 1953; Loeb et al., 1959; Niedermeyer, 1999c).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree