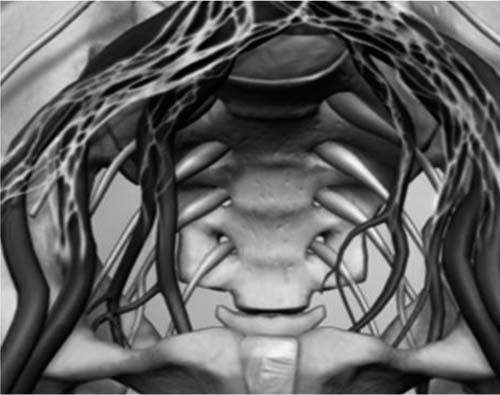
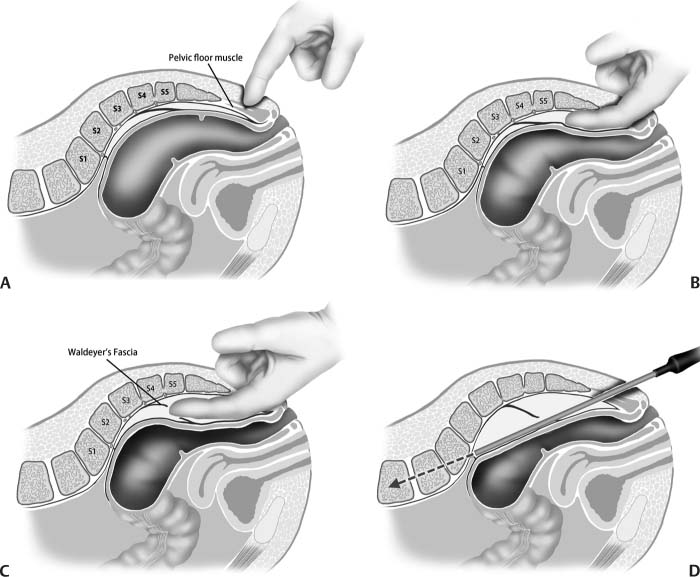
9 Minimally invasive lumbar spine surgery has moved from the feasibility stage in recent years to being achievable due to the development of safe and reproducible advanced access technology and approaches to the lumbar spine. Many innovative surgeons have driven this development by their desire to reduce the iatrogenic morbidity while expediting and improving the fusion and functional outcomes of traditional open spine surgery. On occasion, this can further be expanded to allow the surgeon to treat pathology that before would not have been safe or efficacious to treat. The disadvantages of open lumbar surgery include the need for excessive muscle dissection, nerve retraction, ligamentous and bony dissection, vascular exposure, and disruption of the annulus fibrosus, anterior longitudinal ligament (ALL), and posterior longitudinal ligament (PLL). Traditional fusion approaches can produce undesirable scarring and destabilization of the native anatomy solely related to the exposure. All minimally invasive surgery (MIS) techniques seek to minimize or eliminate these disadvantages. The aim of axial stabilization, using over-the-wire percutaneous techniques, is to provide a similar diskectomy and end plate preparation and to implant an inherently stable fusion construct through smaller incisions and ports. The small axial working channel can make previously open maneuvers, such as access, diskectomy, and implant insertion, more reproducible regardless of the patient’s body habitus. For most MIS techniques, the approach mimics those commonly used in open approaches to the spine, that is, anterolateral, lateral, posterolateral, and extraforaminal exposure of the disk space and incision or excision of the annulus via tubular or expandable retractors. Axial implants and constructs have been used previously in open spine surgery for high-grade slips and corpectomy. The parasagittal fibular strut and vertebral body replacement devices all used this principle.1 A disadvantage of these constructs, however, is the need for open surgery to implant them in patients with degenerative disk disease with or without radiculopathy, including low-grade instability. The approach described here combines the inherent advantages of an axial stabilization and fusion with the least invasive access approach. The spine is a well protected axial column with orthogonal axes defining the sagittal bending, coronal (lateral) bending, and torsional movements. The lumbar spine is surrounded by the viscera anteriorly and the paraspinal musculature, ligaments, and neural elements laterally and posteriorly. The employment of an axial approach avoids these key structures and allows for the design of unique constructs that can achieve the same standard-of-care arthrodesis principles that correspond with currently accepted surgical approaches and biomechanical constructs. An axial approach to the anterior lumbar spine has the potential to improve the biomechanical performance of both fusion and motion-preservation constructs. With this access, posterior instrumentation, and proper technique, a robust axial construct can be placed to restore disk height, sagittal balance, and lordosis with minimal dissection and postoperative pain. Axial disk space entry can simplify the technique of end plate preparation for fusion by reducing the challenges of accessing a collapsed disk space. This muscle-, annulus-, ALL-, and PLL-sparing approach, combined with a completely competent annulus to achieve ligamentum taxis, is another significant potential advantage of the axial technique that may be important in the successful evolution of motion-preserving implants. Before its initial human application, the technique was tested and validated in both cadavers and porcine models. In a series of six porcine models and 15 cadavers, the instruments and technique for percutaneous axial lumbar interbody fusion (AxiaLIF) were developed. Successful axial access to the lumbar spine was achieved in all cases. The instruments evolved to permit fluoroscopically guided access, diskectomy, and stabilization of the L5–S1 motion segment through a single 2 cm incision. In a small access feasibility series of three consecutive patients, biopsy of the lumbosacral disk and vertebral body region was performed for suspected pathological lesions by Cragg et al in May 2002.2 The technique was used with no adverse events. Patients tolerated the procedure well with no significant postoperative pain or morbidity. In the following year a series of three patients underwent an arthrodesis procedure using the axial approach and were observed for 6 months with promising results.2 A human pilot study was initiated with Pimenta et al in November 2003 that included 35 patients with very promising results.3 The first AxiaLIF was performed by Levy (University of Buffalo)4 in January 2005 after U.S. Food and Drug Administration (FDA) regulatory clearance was obtained in late 2004. A group of 10 U.S. spine surgeons initiated treatment of L5–S1 degenerative disk disease patients to validate the pilot work of Pimenta et al, including ~90 patients in 2005. The AxiaLIF procedure was released to the spine community in the United States and Europe in 2006 and has accumulated over 6000 procedures to date and generated 17 peer-reviewed original articles and textbook publications. AxiaLIF is one of the most validated and studied MIS lumbar fusion operations: studies include original articles on anatomy, access, biomechanics, functional outcomes, arthrodesis rates, complications for degenerative disk disease, instability, and adult degenerative scoliosis. Although there are no level I studies and most are small series and level II evidence, the amount of data being compiled and reported is impressive. Preoperative planning is extremely important in AxiaLIF, especially with the addition of the two-level procedure. Radiographic images, including a full sacral view, should be used to determine if the anatomy is suitable. The standard field of view for lumbar magnetic resonance imaging (MRI) and computed tomography (CT) must be expanded to include the coccyx to aid in preoperative planning. For the MRI, the patient should be in a prone position with pelvic elevation. Templates have been developed and are now available to help select appropriate patients and to provide implant sizing and trajectory guidance during preoperative planning as well as during surgery. These templates may be used during surgery following a calibration with one of the access instruments not only to help establish the correct sacral entry point and to guide pin trajectory but also, later on in the procedure, to correctly choose the proper implant size for the patient as well as to help determine how deep to drill in the vertebral body based on the chosen implant. Anterior column fusion via AxiaLIF is achieved via a presacral approach first described by Cragg et al.2 A longitudinal, 2 cm paramedian incision is made ~1 cm off midline. The superior (cephalad) aspect of the incision lies just below the paracoccygeal notch, which is formed by the confluence of the sacrotuberous ligament and sacrospinous ligament. Careful, blunt finger dissection is employed to progress the incision to the parietal fascia. Once crossed, access is gained to the presacral space. The presacral space is bounded anteriorly by the visceral peritoneum of the mesorectum and posteriorly by the parietal fascia covering the sacrum and coccyx. A filmy complex of areolar tissue and fat lies between these fascial layers. The surgeon must exercise caution during dissection to ensure that neither of the fascial borders is compromised. Breaching the mesorectal visceral fascia can lead to colorectal perforation, whereas crossing the parietal, presacral fascia can expose the underlying venous plexus. The rectosacral fascia divides the retrorectal space into inferior and superior compartments. It extends from approximately the third or fourth sacral vertebra to the posterior rectal wall, where it terminates 3 to 5 cm above the anorectal junction in the rectal visceral fascia.5 This fascia can be thick in some patients and require either careful blunt dissection or, in some cases, sharp dissection with an 8 in Kelly/Pean forceps. Several vascular structures are present in the presacral space, although most are avoided by maintaining a midline approach while traversing the sacrum. The primary exception is the middle sacral artery, which courses from the L5–S1 disc space to the coccyx. Parietal branches of the middle sacral artery proceed to the lateral sacral arteries; visceral branches of the middle sacral artery proceed to the posterior rectum. The path of the middle sacral artery has been shown to be extremely variable, however, and may not be encountered at all during the AxiaLIF procedure. A detailed examination of presacral anatomy by Yuan et al6 provides additional insight into proximity of major vascular structures. In this study, the average distance from the sacral midline at the S1–2 level to the left internal iliac artery was 4.3 cm (MRI)/4.0 cm (CT); the average distance to the right internal iliac artery was 3.8 cm (MR/CT). Additionally, the average thickness of the presacral space was found to be 1.2 cm (MR)/1.3 cm (CT). This agrees with Oto et al, whose measurements ranged from 1.06 to 1.62 cm, with significantly thicker presacral widths observed in males (Fig. 9.1).7 The sympathetic plexus is usually found at the L5–S1 interspace and is not encountered in the typical AxiaLIF surgery, where entry to the sacrum most often occurs at the S1–2 level. The operative techniques are detailed in prior literature.8,9 Meticulous preoperative planning must be conducted initially for each patient. Multiplanar imaging facilitated with MRI and plain x-ray films should be utilized for proper patient selection. These studies further delineate the quantity of the mesorectum at plane, the sacral morphology and sagittal trajectory for appropriate guide wire placement. A standard bowel preparation is performed the evening before surgery. In the OR, the patient is to be placed in a prone position on a fluoroscopically compatible surgical table. The sacrum is positioned and raised with flexion and padding of the hips to establish proper posture for axial entry. Optionally, insufflation of air into the rectum is achieved by a rectal catheter, then the operative site is prepared with an adhesive barrier to exclude the perineum. Fig. 9.1 Presacral anatomy—safety zone along midline next to sacrum. Minimally invasive axial access to the lower lumbar spine is via the entry site near the apex of the superior gluteal fold. The paracoccygeal ligamentous notch is palpable and is the entry window into the presacral space. A blunt guide pin is advanced to the arch of the caudal sacrum and directed inferiorly under the arch. The guide pin must be carefully advanced and limited upon entry into the pelvis. The guide pin shaft must be deflected downward after traversing the pelvic fascial layer. Biplane fluoroscopy is necessary to ensure safe advancement of the blunt guide wire in the midline presacral space, while the pin position against the sacrum is maintained by downward pressure on the guide pin shaft. When the pin reaches the S1–2 interspace, the trajectory of entry into the anterior lumbar spine is further defined and confirmed by examination of anteroposterior (AP) and lateral fluoroscopy. A sharp beveled guide pin is tapped into the sacrum, followed by sequential dilation to enlarge the soft tissue plane and the entry tract into the sacrum. Axial disk access is accomplished through the 9 mm working channel, and a cannula maintains the trajectory and safe passage of instrumentation into the disk space (Fig. 9.2). Fig. 9.2 (A–D) Stages of the approach. Expandable nitinol curettes are utilized for debulking the nucleus pulposus, the disk tissue is removed, and the end plates abraded within a defined radius to provide a bleeding bed for fusion. The excised disk material is extracted with a series of wire tissue extractors through the same working cannula. A variable pitch and diameter fixation rod is then inserted through an exchange cannula that provides axial distraction and indirect decompression of the L5–S1 segment. An appropriately selected distraction rod is inserted and the transosseous tunnel engaged from the sacrum to the fifth lumbar vertebrae. This differential pitch creates a distraction of the vertebral bodies at a rate dependent on the difference of the thread pitches. Intervertebral fixation is accomplished through the placement of an appropriately sized single fixation rod. After implantation, the access cannula is removed, the skin closed, and an occlusive dressing placed at the percutaneous access site. If indicated, a mini–open decompression and/or posterior instrumentation with facet screws or pedicle screws, with or without concomitant posterior fusion, can be performed in the routine fashion.
Alternative Approaches for Lumbar Fusion: Axial Lumbar Interbody Fusion (AxiaLIF)
Preoperative Evaluation
Operative Technique with Anatomical Considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree