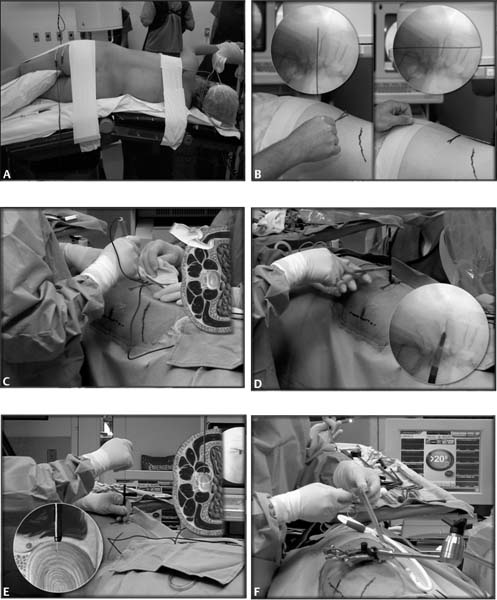
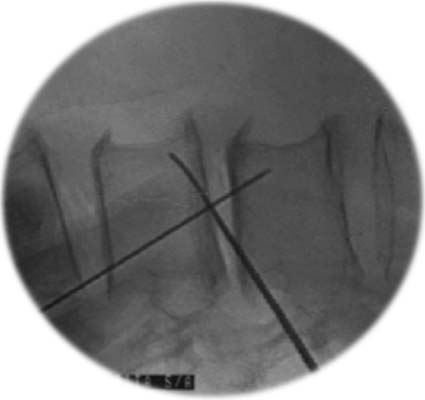
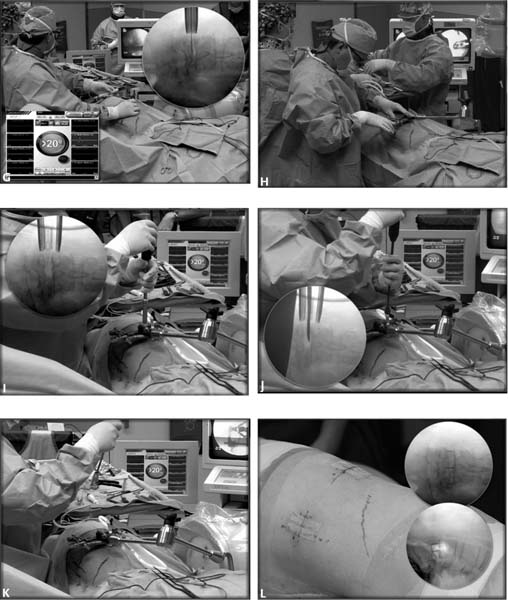
8 Chronic low back pain has been recognized as a complex disorder associated with wide-ranging adverse consequences.1–6 Patients suffering from a painful lumbar motion segment not resolved with conservative management gain benefit from lumbar arthrodesis.7 Lumbar spine fusion has become a commonly performed surgery, and its use continues to rise, with the annual number of spinal fusion operations increasing every year.8 Initially, reconstructive spinal fusion surgery was used for the management of infectious conditions, adolescent scoliosis, and trauma. The indications for spinal fusion among these patients have remained largely unchanged. Based on these experiences, the use of spinal arthrodesis has been extended to treat degenerative lumbar disorders, spondylolisthesis, and disk-related problems.9 Anterior lumbar interbody fusion (ALIF) is the technique commonly used to achieve lumbar interbody arthrodesis. The ALIF allows restoration of disk space, lumbar lordosis, and spinal alignment, without compromising posterior tension bands.10–13 Besides, resection of the disk eliminates a source of diskogenic back pain. Disadvantages of ALIF include the necessity of an access surgeon, high incidence of vascular injury, and retrograde ejaculation. In addition, ALIF is associated with increased operating time and blood loss, as well as prolonged recovery time.14 Minimally invasive surgical techniques have been demonstrated to provide several benefits, which include less tissue trauma, preservation of normal anatomical structures, and a faster recuperative period.15–18 The eXtreme Lateral Interbody Fusion (XLIF, NuVasive, Inc., San Diego, CA) approach may offer various clinical advantages over more traditional techniques for lumbar fusion.19 This minimally invasive procedure realigns the end plates to a horizontal position through bilateral annular release, placement of a large implant across the disk space spanning the ring apophysis, and the effects of ligamentotaxis. The XLIF technique restores disk and foraminal heights, indirectly decompressing the neural elements, and promotes stabilization through an anterior intervertebral fusion. Indications for the XLIF technique are the same as those for any interbody fusion, with the limitation of access only at disk levels above L5. Such patients typically suffer diskogenic pain due to segmental instability, disk degeneration, degenerative scoliosis, and/or grade 1 or 2 spondylolisthesis.20–24 It may also be applied to patients who have failed prior surgery and require interbody fusion, or in cases of adjacent-level disease. Pseudarthrosis and failed lumbar total disk replacements have also been treated using the XLIF approach for retrieval and revision. The XLIF approach has been successfully accomplished for levels above and including L4–5. Approaching the L5–S1 level using this technique is not recommended because of the risk of iliac vessel injury as well as the difficulty of accessing the disk space due to the iliac crest. For the L5–S1 level it is preferable to use a mini–open retroperitoneal approach or minimally invasive posterior approach. Usually the initial x-ray workup begins with flexion and extension films to determine the amount of sagittal instability and the amount of kyphosis flexibility. Oblique views can be useful in this technique as well. A focused lumbar or thoracic view is helpful to evaluate disk height, disk asymmetry, and lateral listhesis. Computed tomographic (CT) scans associated with myelographic study are used to evaluate central and foraminal stenosis. Magnetic resonance imaging (MRI) is useful for evaluating disk degeneration and foraminal stenosis. Other ancillary tests, such as diskography and facet blocks, are done to elucidate which levels should be included in the fusion procedure. For the XLIF approach, the patient is placed and taped in a true 90 degree lateral decubitus position (Fig. 8.1A). A cross-table anteroposterior (AP) image helps to confirm the true 90 degree position. The table and/or patient should be flexed in such a way as to increase the distance between the iliac crest and the rib cage, especially useful at upper lumbar levels and at L4–5. After aseptic treatment of the skin, a K-wire and lateral fluoroscopic image are used to identify the midposition of the disk of interest (Fig. 8.2). A mark is made on the patient’s lateral side, overlying the center of the affected disk space (Fig. 8.1B); a small incision will be created for insertion of atraumatic tissue dilators and an expandable retractor (MaXcess, NuVasive, Inc., San Diego, CA), which will be the working portal (Fig. 8.1C). An incision posterior to this lateral marking is first made to introduce a finger into the retroperitoneal space to sweep open the space and ensure that any lateral attachments of the peritoneum are released to provide safe lateral entry. Fig. 8.1 eXtreme Lateral Interbody and Fusion (XLIF) surgical technique (NuVasive, Inc., San Diego, CA). (A) Patient positioning. (B) Index level identification. (C) Retroperitoneal access. (D,E). Transpsoas access. (F) MaXcess tractor (NuVasive, Inc., San Diego, CA) insertion. (G) NeuroVision Electromyographic System (NuVasive, Inc., San Diego, CA). (H) MaXcess fixation. (I) Diskectomy. (J) End plate preparation. (K) Implant insertion. Fig. 8.2
Alternative Approaches for Lumbar Fusion: eXtreme Lateral Interbody Fusion (XLIF)
Preoperative Evaluation
Indications
Preoperative Imaging
Operative Technique
Patient Positioning
Incision
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree