♦ Preoperative
History and Physical Examination
- Detailed history including prenatal events, birth and developmental history, and possible epilepsy risk factors are obtained.
- Neurologic examination focuses on sensorimotor, language, and visual function.
- Cognitive function should be generally assessed.
- Degree of motor impairment needs to be accurately documented to help counsel parents on what to expect postoperatively. Similarly, presence or absence of a hemianopsia should be assessed and parents need to be counseled about the presence of a contralateral hemianopsia postoperatively.
Clinical Semiology and Video Electroencephalography
- Perform preoperative video electroencephalography monitoring to document seizure semiology and interictal/ictal electroencephalographic (EEG) data. Seizure type(s) and location of epileptic events are documented and characterized.
- EEG findings can be variable with lateralization to the ipsilateral diseased hemisphere or in a bilateral/generalized pattern. Bilateral EEG activity is not necessarily a contraindication for surgery.
Magnetic Resonance Imaging
- Routine magnetic resonance imaging (MRI) including volumetric T1, T2, and fluid attenuated inversion recovery sequencing is performed. MRI also necessary to document the integrity of the unaffected hemisphere.
- Patients with bilateral imaging pathology not necessarily excluded but appropriate caution should be taken.
- Ventricular size, presence of heterotopic cortical dysplasia, anatomy of posterior basal frontal cortex, and location of the midline help define surgical plan.
Other Adjunctive Preoperative Tests
- Perform single photon emission computed tomography and/or 18F-deoxyglucose positron emission tomography scanning (infrequently) to gain additional metabolic information, especially if bilateral disease present on MRI.
- Intracarotid sodium amytal test not routinely performed because of pediatric age considerations and poor baseline language function in some patients. May be of use in the older patient where language transfer might not occur following dominant hemispherectomy.
- Neuropsychologic evaluation should be attempted to gauge developmental delay and establish preoperative baseline. Any associated behavioral problems should also be documented.
Patient Preparation and Anesthetic Issues
- Antiepileptic drugs are not withdrawn and are given the morning of surgery.
- Prophylactic antibiotics and dexamethasone given 30 min before skin incision.
- Premedication with midazolam (0.5 mg/kg) is followed by induction with propofol (5 to 7 mg/kg); anesthesia is maintained with remifentanil (0.2 to 0.3 mcg/kg/min) and isoflurane or sevoflurane.
- Intra-arterial line is placed in the radial or femoral artery. Central venous line is used routinely, especially in small infants with expected larger blood loss (e.g., hemimegalencephaly).
♦ Intraoperative
Positioning
- Head may be positioned in rigid point fixation or resting on a head support, depending on the patient’s age.
- Head turned 90 degrees with ipsilateral shoulder support and the vertex slightly down to allow access to the mesial temporal lobe structures and in-terhemispheric fissure
- Body pressure points are padded and patient covered with warming blankets.
- Head is then shaved and a T-shaped incision planned to allow access from the floor of the middle fossa to the midline of the head.
- Superficial landmarks useful for incisional planning include:
- Anatomic midline from nasion to inion
- The lateral edge of the anterior fontanelle
- Transverse sinus location
- Greater wing of the sphenoid bone
- Z ygo m atic arch
- Transverse sinus location
- Anatomic midline from nasion to inion
Craniotomy (Fig. 63.1)
- T-incision designed by a line at least 0.5 cm from midline and a perpendicular line from the zygomatic root, just anterior to the tragus
- Midline incision extends from the hairline to a point 4 to 5 cm above the inion
- Incision made using a surgical knife with care in the younger patient with an open anterior fontanelle to avoid inadvertent sagittal sinus injury
- All bleeding points carefully controlled with bipolar electrocautery and small hemostatic clips applied to the skin edges. Skin edges are reflected and periosteum and temporalis muscle fascia visualized.
- Incision made using a surgical knife with care in the younger patient with an open anterior fontanelle to avoid inadvertent sagittal sinus injury
- Muscle is mobilized off the underlying bone with a T-shaped incision, reflecting each muscle cuff inferiorly.
- Zygomatic root and anatomic keyhole are identified.
- If applicable, coronal suture should be gently separated from the dura starting from the lateral edge of the anterior fontanelle.
- Burr holes are done at three points:
- The keyhole
- The floor of the middle fossa just above the zygomatic arch
- Along the parasagittal areas just off the midline to avoid sagittal sinus injury (if anterior fontanelle is closed)
- The keyhole
- Optimal craniotomy flap allows exposure to the midline, orbitofrontal base, floor of the middle fossa, and total length of the sylvian fissure.
< div class='tao-gold-member'>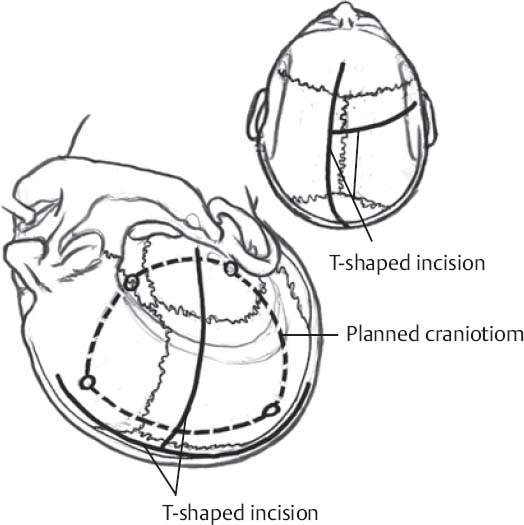
Fig. 63.1 Important superficial landmarks, T-shaped incision, and planned craniotomy.
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





