1 Anatomy A. Meningeal layers
I. Meninges
Layer | Description |
|---|---|
Dura | Tough layer of connective tissue Composed of two layers External periosteal layer—adheres to the periosteum of the calvaria within the cranial cavity, does not extend beyond foramen magnum (thus, spinal dura has only one layer) Inner meningeal layer—extends beyond foramen magnum and forms the spinal dura, which ends at S2 |
Leptomeninges | Translucent middle layer between the dura and pia, contains tight junctions Composed of fibroblasts, collagen fibers, and some elastic fibers Subarachnoid space = cerebrospinal fluid (CSF) + cerebral arteries + superficial cerebral veins |
Pia | Directly lines the cerebrum and its fissures, lacks tight junctions Composed of two layers: Intimal layer—avascular, receives nutrients from CSF and neural tissues Epipial layer—continous with arachnoid trabeculae, absent over the convexities The outer layer is covered by simple squamous epithelium. Dentate ligament—formed by pia, stretches from midpoint between dorsal and ventral roots on the lateral spinal cord surface to attach to the arachnoid and dura Filum terminale—extension of epipia which condenses and continues from S2 and ends as the coccygeal ligament. |
B. Virchow–Robin spaces—a perivascular potential space, between blood vessels and the surrounding sheath of leptomeninges entering the nervous tissue (brain and spinal cord)
C. Cisterns—regions where the meningeal layers (pia and arachnoid) are widely separated
1. Surrounding the midbrain—interpeduncular, crural, ambient (contains the vein of Galen, posterior cerebral [PCAs] and superior cerebellar arteries [SCAs]), and quadrigeminal cisterns; also, cerebello-medullary (cisterna magna), pontine, chiasmatic, sylvian, and lumbar (maximal at L2) cisterns
D. Meningeal blood supply, innervation, and embryological origins
Blood Supply | Neural Innervation | Embryologic Origin |
|---|---|---|
Anterior meningeal artery (ophthalmic artery) Middle meningeal artery (maxillary branch) Posterior meningeal artery (occipital and vertebral arteries) Blood supply to the tentorium: Cavernous internal carotid artery Superior cerebellar artery Proximal posterior cerebral artery | Supratentorial dura: V1: Anterior fossa V2: Middle fossa V3: Posterior fossa, mastoid air cells | Ectoderm: Leptomeninges Ependyma Neural parenchyma Glia |
Infratentorial dura: Upper cervical roots (C2, C3) Cranial nerve X | Mesoderm: Dura Blood vessels | |
Spine: Recurrent branches of the spine (via interventricular foramina) |
|
II. Cerebrospinal Fluid
A. Function: waste removal, carry nutrition to the brain, cushioning of the brain and regulating various brain functions via neurotransmitters, paracrine and endocrine effects. Hypothalamic hormones are secreted into the cerebrospinal fluid (CSF) and transported by the ependymal cells to the hypophyseal portal system.
B. CSF constituents
Components | Values | Additional Comments |
|---|---|---|
Ions and biochemistry | Comparison with plasma: ↑ in CSF: Cl− ↓ in CSF: K+, Ca2+, uric acid, and glucose Same: Na+, osmolarity Normal values in CSF: Glucose = 45–80 mg/dL (⅔ of serum value) Protein ≤45 mg/dL | β-transferrin: found exclusively in the CSF, used to assess CSF leak Froin’s syndrome: CSF xanthochromia and clotting (due to the presence of fibrinogen) occur when CSF is loculated, usually in the lumbar thecal sac. CSF protein is increased (up to 1000 mg/L). CSF Specific gravity: 1.007 CSF pH: 7.33–7.35 |
Cellular | Lymphocytes: <5 PMNs and RBCs: none | Traumatic tap = 700 RBCs per 1 WBC |
Abbreviations: CSF, cerebrospinal fluid; PMNs, polymorphonuclear neutrophils; RBCs, red blood cells; WBC, white blood cell
C. CSF production
1. Active process—Na+ is actively secreted into the subarachnoid space via Na+/K+ adenosine triphosphate (ATP) pump with H2O from vessels following the Na+ ions
2. Sites of CSF production
a. 70% Choroid plexus
b. 18% Ultrafiltrate
c. 12% Metabolic H2O production
3. Control of CSF production
a. Raphe nuclei send axons (serotonin) to the periependymal vessels.
(1) Carbonic anhydrase inhibitors (acetazolamide)
(2) Norepinephrine (NE)
c. Increased production
(1) Volatile anesthetics and CO2
4. CSF volumes in a 70 kg man
a. 450 mL = CSF production each day. CSF production is 0.3–0.37 mL/minute, 20 mL/h
b. 150 mL = total volume
c. 25 mL = within ventricles
5. Choroid plexus—a single layer of cuboidal epithelial cells surrounding blood vessels, involved in CSF production. Primarily located in
a. Roof of the fourth ventricle
b. Inferior medullary velum and lateral recess to the foramen of Luschka
c. Posterior roof of the third ventricle
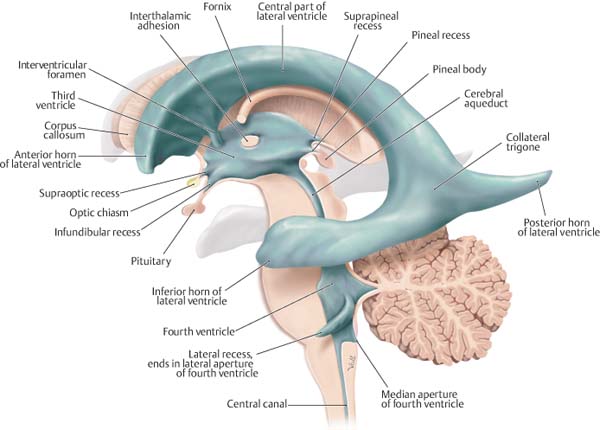
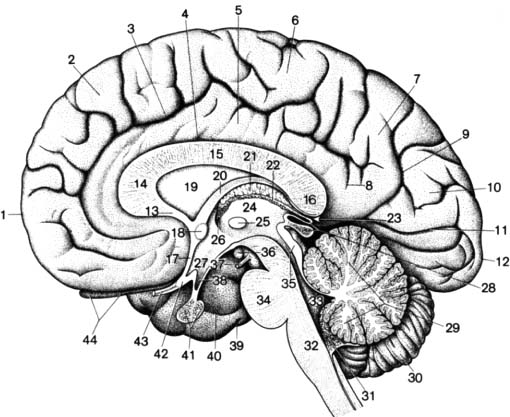
d. Floors of the bodies and roofs of the temporal horns of the lateral ventricles (LVs) (Fig. 1.1)
D. CSF absorption
1. Passive process—absorption by arachnoid granulation cells that transmit CSF in giant cytoplasmic vacuoles via bulk flow into the venous sinuses
Fig. 1.1 Overview of the ventricular system and important neighboring structures. Left lateral view. The ventricular system is an expanded and convoluted tube that is the upper extension of the central spinal canal into the brain. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
2. Control of CSF absorption—pressure-dependent
3. Arachnoid granulations
a. Most abundant at the superior sagittal sinus, contains arachnoid villi
b. A pressure-dependent one-way valve, with collapsing tubules that transmit CSF when intracranial pressure (ICP) is 3–6 cm H2O greater than the venous pressure
E. Intracranial pressure
1. Monro–Kellie doctrine—the closed skull has a fixed/constant volume with
a. 1500 mL brain tissue
b. 150 mL blood (arteries + veins)
c. 150 mL CSF (total volume)
d. Any added volume (brain swelling due to edema, increased blood volume, increased CSF, tumor, hemorrhage, etc.) forces removal of normal inhabitants of the cranial cavity.
2. Normal ICP values
a. <10–15 mm Hg—adults and older children
b. 3–8 mm Hg—younger children
c. 1.5–6 mm Hg—infants
III. Brain Barriers
A. Blood–brain barrier (BBB) formed by
1. Capillary endothelial tight junctions (mainly)
2. Pinocytic activity in endothelial cells
3. Astrocytic foot processes
B. Molecular movement across the BBB
1. Diffusion
2. Carrier-mediated transport (D-glucose, amino acids)
3. Active transport
C. Permeability across the BBB
1. Highly permeable—H2O, CO2, O2, lipid-soluble (ethanol, barbiturates, heroin, and anesthetics)
2. Slightly permeable—ions (Na+, Cl−, and K+)
3. Impermeable—plasma proteins, protein-bound molecules, large organic molecules, and L-glucose
D. Blood–CSF barrier is formed by the tight junctions of choroid cuboidal epithelium (although blood vessels have fenestrated capillaries).
E. Circumventricular organs are midline ventricular system structures of specialized tissues with absent BBB due to fenestrated capillaries.
1. Circumventricular organs (from rostral to caudal)
Feature | |
|---|---|
Organum vasculosum (lamina terminalis) | Outlet for hypothalamic peptides Detect peptides, amino acids, and proteins in blood |
Neurohypophysis | Outlet for hypothalamic hormones (vasopressin and oxytocin) |
Median eminence of the hypothalamus | Release hypothalamic-releasing factors |
Subfornical organ | May be involved in body fluid regulation Located between the foramina of Monro Connected to the choroid plexus |
Subcommissural organ | Function: unknown, located under the posterior commissure The only circumventricular organ with an intact BBB |
Pineal gland | Melatonin production Role in circadian rhythm |
Area postrema | A chemoreceptor that induces emesis when stimulated by digitalis or apomorphine Located on the floor of the fourth ventricle The only paired circumventricular organ |
IV. Blood Supply to the Brain
A. General – The brain constitutes only 2% of body weight (1500 g) but receives 17% of the cardiac output and uses 20% of the body’s oxygen.
B. Cerebral blood flow
Cerebral Blood Flow | Flow Rate (mL/100 g of Brain Tissue per Minute) |
|---|---|
Normal | 50 |
Ischemic penumbra (reversible) | 8–23 |
Irreversible neuronal death | < 8 |
C. Origins of great vessels
1. Brachiocephalic (innominate)—bifurcates into the right common carotid artery and left subclavian artery → vertebral artery → internal mammary artery → thyrocervical trunk → costocervical trunk
2. Left common carotid artery
3. Left subclavian artery gives off vertebral, thyrocervical, and costocervical trunks.
a. Vertebral artery dominance
(1) Left side = 50%
(2) Right side = 25%
(3) Nondominance = 25%
b. The left vertebral artery arises from the aorta in 5% of cases; 40% of the population has a hypoplastic vertebral artery.
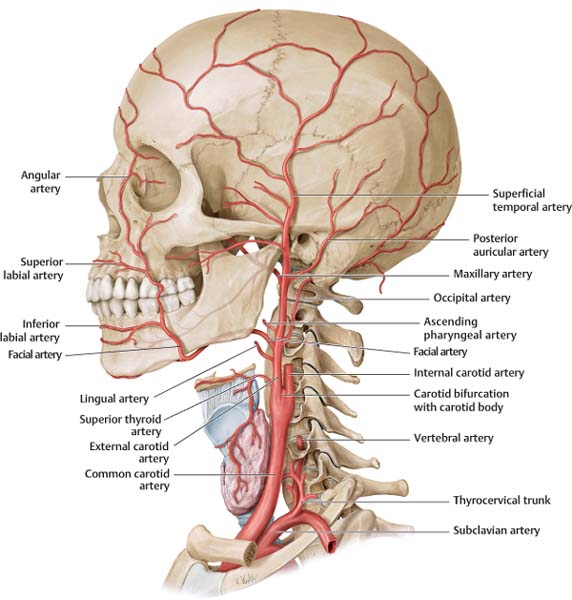
Fig. 1.2 Overview of arteries of the head. Left lateral view. The common carotid artery divides into internal and external carotid arteries at the carotid bifurcation, which is usually at the level of the fourth cervical vertebra. There are eight branches of the external and none of the cervical internal carotid artery. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Karl Wesker.)
D. External carotid artery (ECA)—vascular supply to the brain can be variable depending on several leptomeningeal anastomoses, many of which are from the external carotid circulation. The ECA is anteromedial and smaller than the internal carotid artery (ICA) and has eight major branches (mnemonic: SALFOPS max) (Fig. 1.2).
E. ECA branches
Vascular Supply and Anastomoses | |
|---|---|
Superior thyroid artery (A) | Larynx and upper thyroid Thyrocervical trunk (branch of the subclavian artery) supplies the inferior thyroid and isthmus. |
Ascending pharyngeal artery (M) | Nasopharynx, oropharynx, and middle ear CNs IX, X, and XI Meninges Anastomoses with the vertebral artery branches |
Lingual artery (A) | Tongue and the floor of the mouth |
Facial artery (A) | Face, palate, and lips Angular branch of the facial artery anastomoses with the orbital branch of the ophthalmic artery. |
Occipital artery (P) | Posterior scalp, upper cervical musculature Posterior fossa and meninges Anastomoses with the vertebral artery |
Posterior auricular artery (P) | Pinna, external auditory canal, and scalp |
Superficial temporal artery | Scalp and ear |
Internal maxillary artery | Deep face Gives off the middle meningeal artery (MMA) and accessory meningeal arteries Anastomoses with inferior lateral cavernous sinus trunk and ophthalmic artery through ethmoidal branches |
Branch direction from the ECA (A) = anteriorly, (M) = medially, (P) = posteriorly.
F. Internal carotid artery (ICA)
1. ICA segments
a. Cervical segment (C1)—no branches, originates from the common carotid artery (CCA) at C3–C4 or C4–C5 level. It is the larger of the two terminal CCA branches. ICA initially lies posterolateral to the ECA then becomes medial to the ECA to enter the carotid canal just anteromedial to the internal jugular vein (IJV), separated from it by CNs IX–XII.
b. Petrosal/intraosseous segment (C2)—enters the carotid canal in the petrous temporal bone anterior to the IJV/jugular fossa and lies behind the eustachian tube. This segment is variable and may provide collateral blood flow from ECA during ICA occlusion.
(1) Intraosseous segment of the ICA:
(a) Vertical segment—10 mm in length, begins where the ICA turns anteromedially to the tympanic cavity and cochlea and anterior to IJV
(b) Genu – slightly inferior and anterior to the cochlea and tympanic cavity
(c) Horizontal segment – almost 20 mm in length, exits the canal at petrous apex superior to the cartilage-filled foramen lacerum
(2) Intraosseous branches of the ICA:
(a) Caroticotympanic artery—embryonic hyoid artery remnant, rises near the genu to pass superiorly to supply the middle and inner ear. Aberrant course can cause a retrotympanic pulsatile mass (differential diagnosis [DDx] = glomus tympanicum tumors). Anastomoses with inferior tympanic artery (ascending pharyngeal artery branch).
(c) Periosteal arterial branches: Persistent arteries of the petrosal/intraosseous segment:
Anomalous Artery | Feature |
|---|---|
Persistent stapedial artery | Embryonic stapedial artery that fails to involute (primitive hyoid branch of the internal carotid artery) Course: from the vertical segment, it exits through a bony canal on the cochlear promontory and traverses the footplate of stapes to terminate as the middle meningeal artery If persistent stapedial artery is present, foramen spinosum is either small or absent with enlarged geniculate fossa (Y-shaped) |
Persistent otic artery | Primitive otic artery that fails to involute Embryonic carotid–basilar anastomoses Connects petrous internal carotid artery to embryonic dorsal longitudinal neural arteries; very rare |
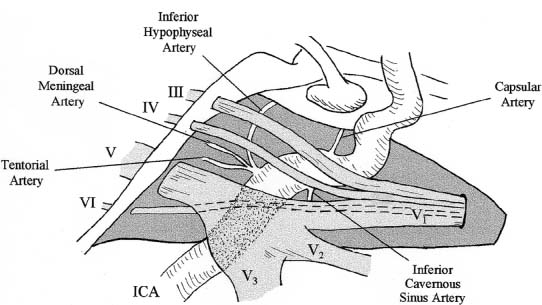
c. Intracavernous segment (Fig. 1.3)—extends from the ICA at exit from the carotid canal and terminates at the entrance into the subarachnoid space adjacent to the anterior clinoid. It travels in the cavernous sinus and is covered by the trigeminal ganglion. CN VI lies inferolaterally, CN III, IV, V1, and V2 are lateral (within the lateral dural wall).
Fig. 1.3 Branches of the cavernous segment of the internal carotid artery (ICA).
(1) Intracavernous segment of ICA (proximal → distal):
(a) C5: ascending portion—entrance into the cranium to the genu
(b) C4: posterior genu—between C5 and C3 segments
(c) C3: horizontal portion—between the genu
(d) C2: anterior genu
(e) C1—remainder of the ICA segment
(2) Intracavernous branches of ICA:
(a) Meningohypophyseal trunk (posterior trunk) has three branches:
(i) Tentorial artery (of Bernasconi and Cassinari)—tentorium
(ii) Inferior hypophyseal artery—neurohypophysis
(iii) Dorsal meningeal artery (clival branch)—CN VI and part of the clivus
(b) Inferolateral trunk (artery of the inferior cavernous sinus) travels to
(i) Inferolateral cavernous sinus wall
(ii) Tentorium (via tentorial branch)
(iii) Foramen ovale and spinosum to supply CN III, IV, VI, and gasserian ganglion
(iv) The most important anastomoses include
• Maxillary artery (via artery of the foramen rotundum)
• MMA and ophthalmic artery
(d) Medial trunk (McConnell’s capsular arteries)—supplies the anterior and inferior pituitary gland, present only in 28% of the population, the most distal branch from the C3 and C2 segment
(i) Anterior capsular artery—courses medially over the sellar roof
(ii) Inferior capsular artery—courses inferomedially, supplies the sella floor
(3) Persistent arteries of the intracavernous segment
Anomalous Artery | Feature |
|---|---|
Persistent trigeminal artery | Most common primitive internal carotid artery–basilar anastomosis 0.02–0.06% of all cerebral angiograms Associated with higher incidence of vascular abnormalities (25%), aneurysms most common |
Intracavernous anastomoses | Internal carotid artery aplasia; very uncommon |
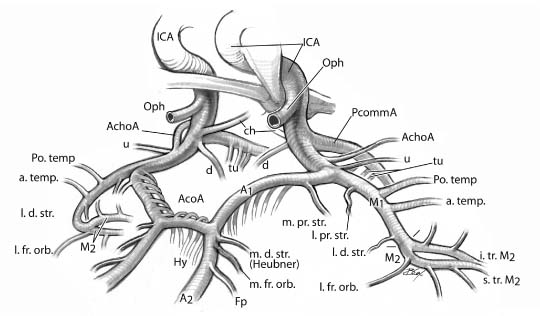
d. Intradural segment/supraclinoid ICA (Fig. 1.4 and Fig. 1.5)—Branches of the extracavernous intradural segment include the ophthalmic, superior hypophyseal, posterior communicating, anterior choroidal branches, and branches to the hypothalamus, optic nerve, and chiasm.
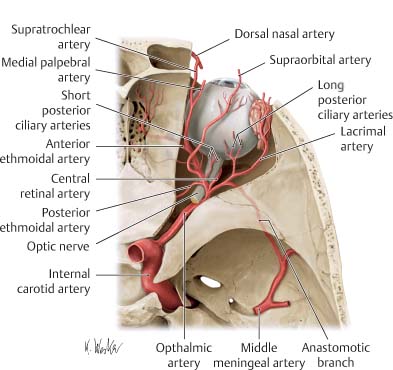
(1) Ophthalmic artery (OA)—supplies the orbit (additional minor contributions from the infraorbital branch of the maxillary artery that anastomoses with OA) (Fig. 1.6)
(a) Usually the first intracranial ICA branch (intradural origin in 93%)
(b) Course—arises superomedial or anteromedial to the ICA and under the anterior clinoid process (rarely OA originates within the cavernous sinus). OA initially lies inferolateral to CN II, and medial to CN III and VI. It crosses between CN II and the superior rectus muscle to the medial orbital wall between the medial rectus and superior oblique muscles.
(c) In 0.5% of cases, OA arises from the MMA (with risk of blindness after embolization of the MMA if not detected).
(d) Aneurysms arise from the superior wall of the ICA distal to the origin of the ophthalmic artery and point upward against the optic nerve.
(e) OA branches:
(i) Ocular branch—includes central retinal artery and ciliary artery, to supply the retina, choroid of the eye, and portions of the ON
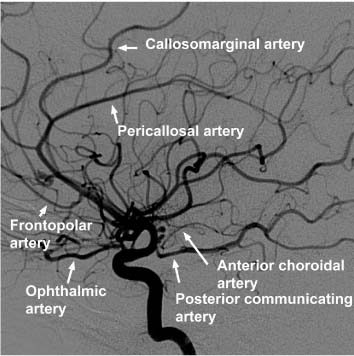
Fig. 1.4 View of the anterior circle of Willis as it would be seen from a right pterional approach.
(ii) Orbital branches:
• Lacrimal artery—supplies lacrimal gland and conjunctiva. The most significant branch of the lacrimal artery is the recurrent meningeal artery, which turns backward through the superior orbital fissure to anastomose with the MMA.
• Muscular artery—supplies extraocular muscles and the orbital periosteum
(iii) Extraorbital branches—include supraorbital, anterior and posterior ethmoidals, dorsal nasal, medial frontal, palpebral, and supratrochlear arteries. These branches possess extensive anastomoses with the ECA (via ethmoidal and anterior falcine artery) for collateral intracranial flow during proximal ICA occlusion.
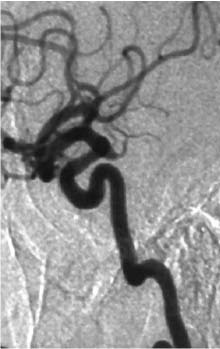
Fig. 1.5 Lateral internal carotid artery catheter angiogram.
(2) Superior hypophyseal arteries—several small arteries arising from the posteromedial portion of the intradural ICA
(a) They course beneath the optic nerve to supply:
(i) Pituitary (anterior pituitary lobe, pituitary stalk) and tuber cinereum
(ii) Optic nerve and chiasm (inferior surface)
(b) These arteries anastomose with the arteries of the contralateral as well as the inferior hypophyseal arteries to form the hypophyseal portal system.
(c) Aneurysms arising from this region point inferiorly and medially.
(a) Perforators— ~ Seven perforators evenly distributed along the PcommA course superomedially to supply the posterior hypothalamus, anterior thalamus, subthalamic nucleus, and posterior limb of the internal capsule (IC). The largest perforator (anterior thalamoperforating artery) terminates between the mamillary bodies and optic tracts.
Fig. 1.6 Branches of the ophthalmic artery. Right orbit, superior view after opening of the optic canal and orbital roof. The ophthalmic artery is a branch of the internal carotid artery. It runs below the optic nerve through the optic canal to the orbit and supplies the intraorbital structures, including the eyeball. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Karl Wesker.)
(b) PcommA variants are observed in 50% of cases, including absent or hypoplastic (30%), fetal origin (20%), duplicated or triplicated:
(i) Fetal origin of the PCA (“fetal PCA”)—when PcommA diameter is the same as PCA. Failed regression of fetal PCA leads to dominant blood supply of occipital lobes from ICA (via fetal PCA) rather than from the vertebrobasilar system (20% unilateral and 8% bilateral).
(ii) Infundibulum—a funnel-shaped dilatation observed at the junction between PcommA’s origin and ICA. Dilatation is usually <2 mm in diameter with wide base at the ICA origin (DDx = ICA–PcommA aneurysm); seen in 10% of PcommAs (Fig. 1.7).
(c) Aneurysms usually arise from the posterior wall of the carotid artery just distal to the PcommA’s origin and point posteriorly toward CN III. The PcommA is on the inferomedial side of the aneurysm. The anterior choroidal artery (ChA) is superior/superolateral to the aneurysm.
(4) Anterior choroidal artery—arises from the posteromedial surface of the ICA, 2–4 mm distal to the PcommA’s origin. Aneurysms tend to be located superior or superolaterally to the origin of the anterior ChA. It anastomoses with the lateral posterior ChAs and has two segments:
(a) Cisternal segment—courses posteromedially within the suprasellar cistern beneath (inferior and lateral) the optic tract, then turns posteromedially around the uncus
(b) Intraventricular segment—continues from the cisternal segment. Prior to reaching the lateral geniculate body, it turns posterolaterally through the crural and ambient cisterns to enter the choroidal fissure (plexal point) of the temporal horn. Perforators (3–10) supply:
(i) Visual system—inferior optic chiasm, posterior portion of the optic tract, optic radiation, lateral geniculate body
(ii) Temporal lobe—uncus, parahippocampal gyrus, amygdala
(iii) Choroid plexus in the temporal horn and atrium
(iv) Basal ganglia—globus pallidus medius, tail of caudate, internal capsule (genu)
(v) Diencephalon—subthalamus, lateral ventroanterior (VA) and ventrolateral (VL) thalamic nuclei
(vi) Midbrain—middle third of the cerebral peduncle, upper red nucleus, substantia nigra
(5) Dural artery—a small branch that arises from the ICA 3–5 mm proximal to the bifurcation; courses anteriorly to supply the dura of the anterior clinoid process
(6) Carotid siphon—intracavernous and supraclinoid segments of the ICA
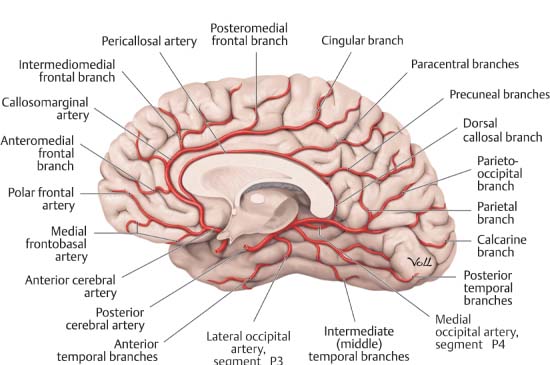
G. Anterior cerebral artery (ACA) (Fig. 1.8)
1. ACA segments
a. A1—horizontal/precommunicating segment
b. A2—vertical/postcommunicating segment
c. A3—distal ACA and cortical branches
d. Anterior communicating—connects right and left ACAs at level of A1–A2 junction
2. Precommunicating segment (A1)—1–12 perforating arteries called the medial lenticulostriate arteries (medial proximal striate arteries)
Fig. 1.7 Posterior communicating artery infundibulum. Lateral internal carotid artery angiogram demonstrates the artery arising from the tip of a pyramidal dilation.
a. Course posterosuperiorly through the anterior perforated substance to supply:
(1) Optic nerve (superior surface) and optic chiasm
(2) Anterior hypothalamus
(3) Septum pellucidum
(4) Anterior commissure
(5) Pillars of the fornix and the anteroinferior striatum
b. Note: Medial distal striate artery = recurrent artery of Heubner (RAH)
3. Anterior communicating artery (AcommA)—located in the cistern of the lamina terminalis
a. Two or more perforators arise from the AcommA that supply:
(1) Infundibulum
(2) Optic chiasm
Fig. 1.8 Anterior cerebral artery. The major branches are the orbitofrontal (medial frontobasal), frontopolar (polar frontal), anterior internal frontal (anteromedial frontal), callosomarginal, middle internal frontal (interomedial frontal), posterior internal frontal (posteromedial frontal), paracentral (cingular), superior parietal (paracentral), and inferior parietal (precuneal). (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
(4) Preoptic hypothalamus
b. Perforators include the subcallosal artery and medial artery of the corpus callosum.
c. Aneurysms usually arise at the point where the dominant A1 bifurcates at the AcommA and point toward the opposite side.
4. Postcommunicating segment (A2)
A2 | Feature |
|---|---|
Recurrent artery of Heubner (medial distal striate artery) | Arises just proximal or more commonly, distal to the anterior communicating artery and courses back toward the proximal A1, hence the term recurrent It enters the anterior perforating substance. Vascular territory: Head of the caudate Anterior limb of the internal capsule Anterior putamen and globus pallidus Septal nuclei Inferior frontal lobe |
Orbitofrontal artery | Gyrus rectus, medial orbital gyri Olfactory bulb and tract |
Frontopolar artery | Medial frontal lobe Lateral surface of the superior frontal gyrus |
Anterior internal frontal artery | Anterior medial frontal lobe |
5. Distal segment (A3)—distal to the pericallosal–callosomarginal junction
A3 | Feature |
|---|---|
Callosomarginal artery | Cingulate gyrus and paracentral lobule Second most common site for anterior cerebral artery aneurysms (junction of the pericallosal artery) Aneurysms usually point distally. |
Pericallosal artery | Medial parietal cortex and the precuneus |
Middle internal frontal artery | Medial frontal cortex |
Posterior internal frontal artery | Medial posterior frontal cortex |
Paracentral artery | Medial cortex around the central sulcus |
Superior parietal artery | Medial superior parietal lobe |
Inferior parietal artery | Medial inferior parietal lobe |
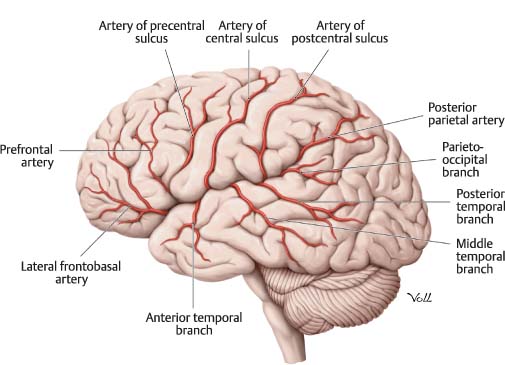
H. Middle cerebral artery (MCA) (Fig. 1.9)
1. MCA segments
a. M1—horizontal segment extends horizontal and lateral beneath the anterior perforated substance, proximal to the bifurcation (50%) or trifurcation (25%)
b. M2—insular segment extends from the bifurcation to the genu which courses around the island of Reil and heads posterosuperiorly into the sylvian fissure
c. M3—opercular segment, opercular branches emerging from the sylvian fissure, a continuation of M2 branches
d. M4—cortical segments
2. M1 segment
M1 | Feature |
|---|---|
Uncal artery | More frequently arises from the distal internal carotid artery (compared with proximal M1) Supply: uncus and underlying white matter |
Temporopolar artery | Supply: anterior pole of the superior, middle, and inferior temporal gyri |
Anterior temporal artery | Supply: anterior pole of the superior, middle, and inferior temporal gyri |
Lateral lenticulostriate arteries | Perforators (2–15) from superior surface of M1 Vascular territory: Substantia innominata Anterior commissure (lateral portion) Putamen (majority) Globus pallidus (lateral segment) Internal capsule (superior half) Head and body of the caudate (except anteroinferior portion) |
Fig. 1.9 Middle cerebral artery. The major terminal branches are the orbital frontal (lateral frontobasal), prefrontal, precentral (artery of the precentral sulcus), central (artery of the central sulcus), anterior parietal (artery of the postcentral sulcus), posterior parietal, angular (parietooccipital branch), posterior temporal, middle temporal, anterior temporal, and temporopolar arteries. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
M2 | Feature |
|---|---|
Superior trunk |
|
Orbitofrontal branch | Supply: orbital portion of the middle and inferior frontal gyri and the inferior pars orbitalis |
Prefrontal branch | Supply: superior pars orbitalis, pars triangularis, anterior pars opercularis, and most of the middle frontal gyrus |
Precentral branch | Supply: posterior pars opercularis, middle frontal gyrus, and inferior and middle portions of the precentral gyrus |
Central branch | Supply: superior postcentral gyrus, upper central sulcus, anterior part of the inferior parietal lobule, and the anteroinferior region of the superior parietal lobule |
Anterior parietal branch | Supply: superior parietal lobule |
Inferior trunk |
|
Posterior parietal branch | Supply: posterosuperior and inferior parietal lobule and inferior supramarginal gyrus Occlusion: cortical sensory loss and hemianopsia |
Angular branch | Supply: posterior aspect of the superior temporal gyrus, portions of the supramarginal and angular gyri, and superior aspect of the lateral occipital gyrus The largest cortical branch of the middle cerebral artery |
Temporooccipital branch | Supply: posterior half of the superior temporal gyrus, posterior extreme of the middle and inferior temporal gyri, and the inferior lateral occipital gyrus |
Posterotemporal branch | Supply: middle and posterior portion of the superior temporal gyrus, posterior ⅓ of middle temporal gyrus, and posterior extreme of the inferior temporal gyrus Occlusion: Wernicke’s aphasia and hemianopsia |
Middle temporal branch | Supply: superior temporal gyrus near the level of pars triangularis and pars opercularis, central part of the middle temporal gyrus, and middle and posterior parts of the inferior temporal gyrus |
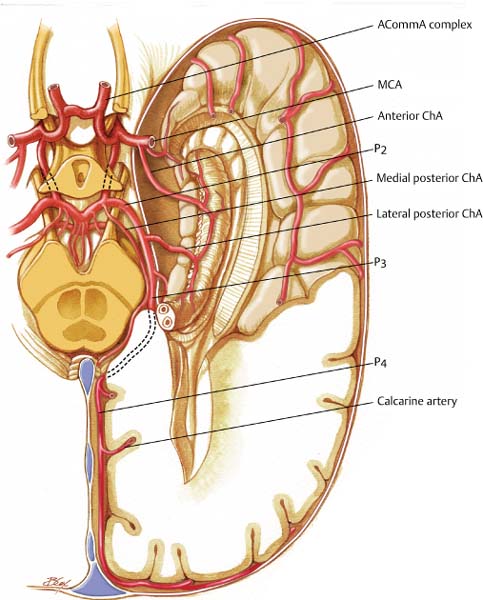
I. Posterior cerebral artery (PCA) (Fig. 1.10)
1. PCA segments
a. P1—precommunicating segment, extends from the tip of the basilar artery to PcommA origin, within the interpeduncular cistern
b. P2—ambient segment, extends from the PcommA to the dorsal aspect of the midbrain (P2A and P2P, anterior and posterior, respectively)
c. P3—quadrigeminal segment, extends from the lateral portion of the quadrigeminal cistern (origin of the posterior temporal artery) to the anterior limit of the calcarine fissure
d. P4—terminal cortical branches
2. Vascular territory—parietooccipital sulcus (medial) and inferior temporal sulcus (lateral)
Fig. 1.10 Posterior cerebral artery. View of inferior surface of brain.
3. P1 segment
P1 Segment | Feature |
|---|---|
Posterior thalamoperforator arteries | From the basilar artery and P1, travels through the posterior perforated substance behind the mamillary bodies Supply: thalamus, hypothalamus, subthalamus, and midbrain (cranial nerves III and IV) |
Medial posterior choroidal arteries | Travels anteromedially along the roof of the third ventricle Supply: midbrain tectum, posterior thalamus, pineal gland, and tela choroidea of the third ventricle |
Meningeal branches | Supply: tentorium and the falx |
P2 Segment | Feature |
|---|---|
Lateral posterior choroidal artery | Main branch of P2, courses over the pulvinar and through the choroidal fissure Supply: posterior portion of the thalamus and choroid plexus (temporal horn and atrium) |
Thalamogeniculate arteries | Medial geniculate body, lateral geniculate body, pulvinar, superior colliculus, and crus cerebri |
Cortical branches | Inferior temporal artery group Supply: inferior portion of the temporal lobe |
5. P3 segment
P2 Segment | Feature |
|---|---|
Posterior temporal artery | Posterior temporal lobe, occipitotemporal and lingual gyri Anterior temporal artery branch travels to the inferior temporal lobe to supply the inferior cortex. Anastomoses with middle cerebral artery |
Internal occipital artery |
|
Parietooccipital artery | Located in the parietooccipital sulcus Supply: posterior ⅓ of the medial hemispheres, cuneus, precuneus, superior occipital gyrus, and precentral and superior parietal lobules Anastomoses with anterior cerebral artery |
Calcarine artery | Located in the calcarine sulcus Supply: occipital pole and the visual cortex Anastomoses with middle cerebral artery |
Posterior pericallosal artery | Supply: splenium of the corpus callosum Anastomoses with anterior cerebral artery |
Choroidal Arteries | Feature |
|---|---|
Anterior ChAs | Arise from the ICA Course: goes through the choroidal fissure → temporal horn of LV Vascular territory: Choroid of the LVs (especially in the lateral horn) Hippocampus, amygdala, uncus Globus pallidus, caudate tail, putamen Thalamus (VL) IC (posterior limb and retrolenticular) Optic tract, lateral geniculate nucleus, optic radiation Historically, this artery was sacrificed to treat Parkinson’s disease: decreased tremor likely due to decreased blood supply to VL thalamus. |
Posterior ChAs (medial and lateral) | Arise from the PCA Medial branches supply pineal gland, tectum, thalamus, choroid of the third ventricle Lateral branches enter the choroidal fissure and anastomose with the anterior choroidal arteries forming variable anastomotic network |
Abbreviations: ChAs, choroidal arteries; IC, internal capsule; ICA, internal carotid artery; LV, lateral ventricles; PCA, posterior cerebral artery; VL, ventrolateral
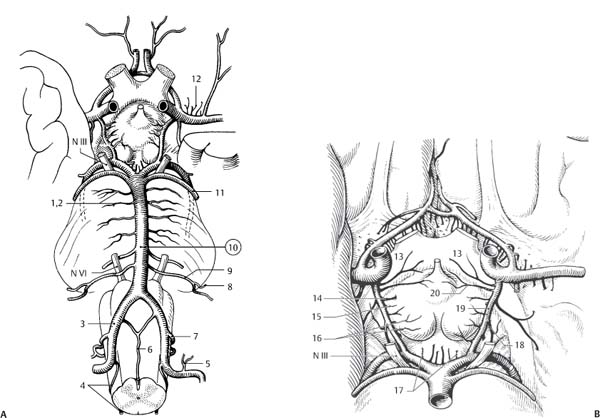
K. Circle of Willis (Fig. 1.11)
1. Arteries that form a polygon encircling the ventral surface of the diencephalon (adjacent to the optic chiasm, mamillary bodies, and infundibulum), located in the interpeduncular fossa, suprasellar and adjacent cisterns. The carotid and vertebrobasilar systems are connected via the circle of Willis. Complete in 25% of individuals, 50% have posterior circulation variations. Consists of the “anterior and posterior circulation”:
a. Anterior circulation—AcommA, A1, ICA
b. Posterior circulation—PcommA, P1, basilar tip
2. Penetrating arteries of the circle of Willis
Arteries | Feature |
|---|---|
Anteromedial arteries | Arise from ACA and AcommA, including RAH Enter the anterior perforated substance Supply: anterior hypothalamus, preoptic nucleus, and supraoptic nucleus |
Posteromedial arteries | Arise from proximal PCA and PcommA Supply: hypophysis, infundibulum, and tuberal hypothalamus Thalamoperforating arteries supply: mamillary bodies, subthalamus, and midbrain |
Anterolateral arteries | Striate arteries from proximal MCA and RAH Enter the anterior perforated substance Supply: head of caudate, lateral globus pallidus, putamen, claustrum internal capsule, and the external capsule |
Posterolateral arteries | Arise from PCA (thalamogeniculate arteries) Supply: caudal thalamus (geniculate bodies, pulvinar, lateral nucleus, and lateral ventral nucleus) |
Abbreviations: ACA, anterior cerebral artery; AcommA, anterior communicating arteries; MCA. middle cerebral artery; PCA, posterior cerebral artery; PcommA, posterior communicating artery; RAH, recurrent artery of Heubner
Fig. 1.11 The circle of Willis with the arteries including main perforating arteries of the brain (A) viewed from inferior and left in situ showing posterior circulation and (B) close-up view of circle of Willis itself. 1. Pontine arteries. 2. Circumferential pontine arteries. 3. Vertebral artery. 4. Posterior spinal artery. 5. Meningeal branches of vertebral artery. 6. Anterior spinal artery. 7. Posterior inferior cerebellar artery. 8. Labyrinthine artery. 9. Anterior inferior cerebellar artery. 10. Basilar artery. 11. Superior cerebellar artery. 12. Mesencephalic arteries. 13. Arteries to optic chiasm. 14. Thalamotuberal artery. 15. Hypothalamic branch. 16. Mammillary arteries. 17. Posterior thalamoperforating arteries. 18. Branch to oculomotor nerve. 19. Posterior communicating artery. 20. Artery of tuber cinereum. (From Dauber W. Pocket Atlas of Human Anatomy. Stuttgart, Germany: Thieme; 2007. Reprinted by permission.)
L. Vertebral artery
1. Course—arises from the subclavian artery, enters the foramina transversarium at C6 in 90%, turns lateral at C2, travels posteriorly along the atlas, entering the skull via foramen magnum
2. Anastomoses—ECA, thyrocervical and costocervical trunks
3. Supply—pyramids inferior olivary nucleus, CNs X and XII, and the reticular formation
Branches | Feature |
|---|---|
Extracranial | Three branches: 1. Segmental spinal branches 2. Muscular branch anastomoses with muscular branch of ECA (ascending pharyngeal, thyrocervical, and costocervical) 3. Meningeal branch Anterior meningeal branch → dura around the foramen magnum Posterior meningeal branch → falx and posterior fossa dura Blood supply to the falx cerebelli = posterior meningeal branches, occipital, ascending pharyngeal and PICA arteries |
Posterior spinal artery | Supply: gracile and cuneate fasciculi and the inferior cerebellar peduncle |
Anterior spinal artery | Supply: pyramid, medial lemniscus, medial longitudinal fasciculus, olive and vagal and hypoglossal nuclei |
PICA | Occasionally arises extracranially, 1–25% of vertebral arteries terminate in the PICA Supply: choroid of fourth ventricle, posterior lateral medulla, tonsils, vermis, and posteroinferior cerebellar hemispheres Five segments: 1. Anterior medullary segment 2. Lateral medullary segment—supply CNs IX, X, and XI 3. Tonsillomedullary segment—forms a large loop 4. Telovelotonsillar segment—between tela choroidea and inferior medullary velum rostrally superior pole of the tonsils caudally 5. Hemispheric branches Occlusion = lateral medullary syndrome (Wallenberg’s) |
Abbreviations: CN, cranial nerve; ECA, external carotid artery; PICA, posterior inferior cerebellar artery
M. Basilar artery
1. Union of two vertebral arteries near the pontomedullary junction, extends along the ventral pons and terminates as paired PCAs (within the interpeduncular cistern)
2. Basilar artery branches
Branches | Feature |
|---|---|
Anterior inferior cerebellar artery | Course: crosses cranial nerve (CN) VI and the cerebellopontine angle cistern to the internal auditory canal and passes anterior and inferior to CNs VII and VIII Supply: CNs VII and VIII, inferolateral pons, middle cerebellar peduncle, flocculus, and anterolateral hemispheres Branches: internal auditory artery, recurrent perforating artery, and subarcuate artery |
Labyrinthine artery | Internal auditory artery Supply: structures of the labyrinth |
Paramedian artery | Supply: ventral pons and midbrain |
Pontine arteries | Long and short circumferential pontine arteries Supply: ventral pons |
Superior cerebellar artery | Course: travels posterolateral around the pontomesencephalic junction below the tentorium, CNs III and IV Supply: superior vermis and cerebellar hemispheres, deep cerebellar white matter, and dentate nuclei |
Posterior cerebral arteries | Refer to above |
Structures | Vascular Supply |
|---|---|
Striatum | Mainly: MCA (lenticulostriate arteries) Rostrally: RAH Caudally: anterior ChA |
Internal capsule | Anterior limb: ACA (RAH, MCA lateral [lenticulostriate arteries]) Genu: ICA perforators, MCA lateral (lenticulostriate arteries) Posterior limb: anterior ChA and PcommA |
Thalamus | PCA by way of posterior thalamoperforators, thalamogeniculate arteries, and the medial posterior ChAs Rostrally from PcommA (anterior thalamoperforating arteries) and basilar bifurcation perforators (posterior thalamoperforating arteries) |
Medulla | Anterior and posterior spinal arteries PICA and vertebral arteries |
Pons | Basilar paramedian branches Short and long circumferential branches of the basilar artery that anastomose with AICA at the middle cerebellar peduncle SCA |
Midbrain | Basilar artery, PCA, SCA, PcommA, and anterior ChA Stroke syndromes include: Weber’s syndrome: CN III palsy with contralateral hemiplegia Benedikt’s syndrome: Weber’s + red nucleus lesion (coarse intentional tremor, hyperkinesias, and ataxia of the upper limb) |
Cerebellum | PICA: inferior cerebellar peduncle, vermis, tonsils, and choroid of the fourth ventricle AICA: middle cerebellar peduncle, choroid of the fourth ventricle, and anterior cerebellum SCA: superior cerebellar peduncle, choroid of the fourth ventricle and the deep nuclei |
Abbreviations: ACA, anterior cerebral artery; AICA, anterior inferior cerebellar artery; ChA, choroidal artery; CN, cranial nerve; ICA, internal carotid artery; MCA, middle cerebral artery; PCommA, posterior communicating artery; PCA, posterior cerebral artery; PICA, posterior inferior cerebellar artery; RAH, recurrent artery of Heubner; SCA, superior cerebellar artery
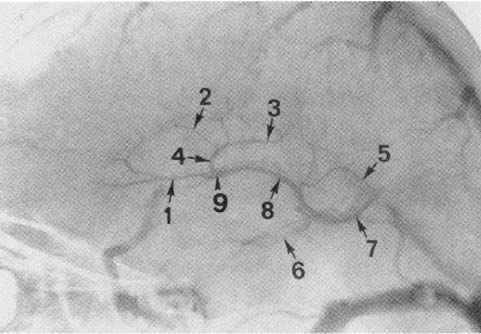
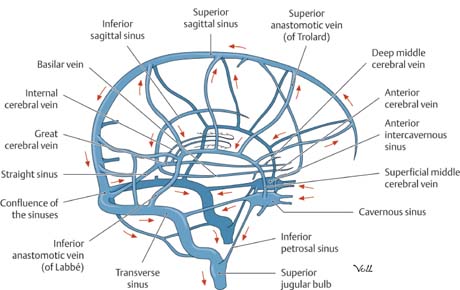
O. Supratentorial venous drainage (Fig. 1.1 and Fig. 1.1)
1. Diploic veins—communicate with the scalp, meningeal veins, and dural sinuses
2. Meningeal veins—epidural vessels of the dura, which follow meningeal arteries. Drainage into dural sinuses or into extracranial pterygoid vertebral plexus
3. Dural sinuses—no valves, communicates with emissary veins
4. Cerebral veins—superficial veins and deep cerebral veins
5. Dural sinuses
Dural Sinus | Feature |
|---|---|
Superior sagittal sinus | Extends from foramen cecum (near crista galli) to the internal occipital protuberance (becomes transverse sinus) Drains predominantly (60%) into the right transverse sinus |
Inferior sagittal sinus | Cortical veins from the medial hemisphere join to form the ISS to join great cerebral vein of Galen to form the straight sinus Drains into → straight sinus → torcula → drains predominantly into the left transverse sinus |
Transverse sinus | From the confluence, courses laterally then curves down the occipitopetrosal junction to become the sigmoid sinus |
Sigmoid sinus | Courses along the posterior aspect of the temporal bone (petromastoid) to become the superior jugular bulb at the jugular foramen and then the IJV Receives blood from the inferior petrosal sinus |
Confluence of sinuses (torcula Herophili) | Dilatation at the internal occipital protuberance that communicates with superior sagittal, straight, transverse, and occipital sinuses |
Petrosal sinuses | Superior petrosal sinus—receives veins from the pons, medulla, cerebellum, and inner ear Inferior petrosal sinus—receives veins from the cerebellum and labyrinthine veins |
Straight sinus | Courses posteroinferiorly along the falx to the tentorium and terminates at the TS Formed by the vein of Galen and ISS |
Cavernous sinus | Drains into: Superior petrosal sinus → transverse/sigmoid sinus junction Inferior petrosal sinus → IJV Communicates with the basilar sinus, pterygoid and pharyngeal venous plexus |
Abbreviations: ISS, inferior sagittal sinus; IJV, internal jugular vein; TS, transverse sinus
Fig. 1.12 Venous anatomy on lateral catheter angiogram. 1. Septal vein. 2. Anterior caudatevein. 3. Terminal vein. 4. Thalamostriate vein. 5. Atrial vein. 6. Basal vein of Rosenthal. 7. Vein of Galen. 8. Internal cerebral vein. 9. Venous angle. (From Alleyne Jr. CH. Neurosurgery Board Review. New York, NY: Thieme;1997. Reprinted by permission.)
Fig. 1.13 Dural sinus tributaries from the cerebral veins (after Rauber and Kopsch). Right lateral view. Venous blood collected deep within the brain drains to the dural sinuses through superficial and deep cerebral veins. The red arrows in the diagram show the principle directions of venous blood flow in the major sinuses. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
Cerebral Veins | Feature |
|---|---|
Superficial veins |
|
Superficial middle cerebral veins | Course along the sylvian fissure Drain into the cavernous sinus Drain into the vein of Trolard → superior sagittal sinus Drain into vein of Labbé → transverse sinus Mnemonic: Trolard = Top, Labbé = Lower |
Superior anastomotic vein | Vein of Trolard, drains from the sylvian fissure → superior sagittal sinus |
Inferior anastomotic vein | Vein of Labbé, drains from the sylvian fissure → transverse sinus |
Deep veins |
|
Internal cerebral veins | Course: located in the tela choroidea of the roof of the third ventricle (velum interpositum), extend from the interventricular foramen, travel over the thalamus and posteriorly to the quadrigeminal cistern, where they join to contribute to the vein of Galen Formed by the union of the thalamostriate, choroidal, septal, epithalamic, and lateral ventricular veins |
Basal vein of Rosenthal | Drains the anterior and medial temporal lobe Course: passes posterosuperiorly through the ambient cistern, joins the internal cerebral vein to form the vein of Galen |
Vein of Galen | Receives both internal cerebral veins, basal veins of Rosenthal, occipital veins, and posterior callosal vein Travels under the splenium and merges with the inferior sagittal sinus to form the straight sinus |
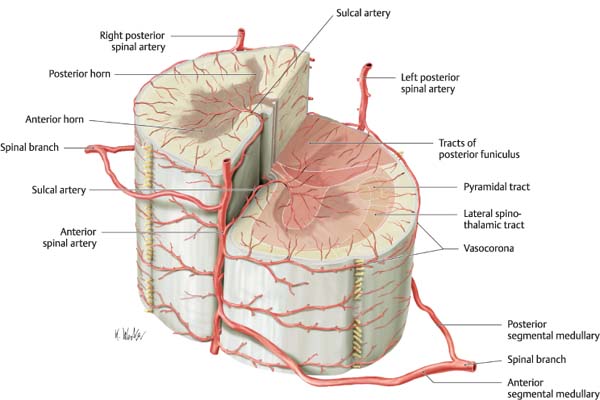
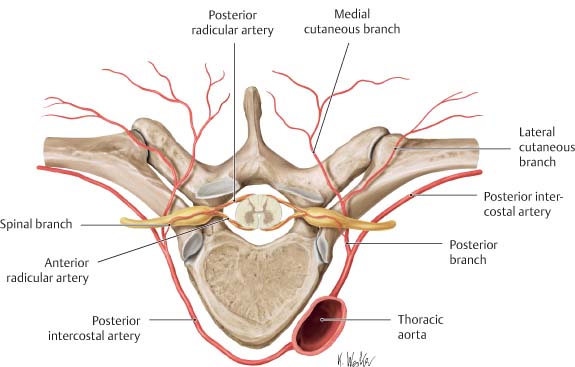
V. Blood Supply to the Spinal Cord
A. Summary of spinal cord blood supply (Fig. 1.14 and Fig. 1.15)
Artery | Vascular Territory |
|---|---|
Vertebral arteries |
|
Posterior spinal artery | Supplies posterior ⅓ of the spinal cord |
Anterior spinal artery | Supplies anterior ⅔ of the spinal cord Two anterior spinal arteries join at the medulla to enter the anterior median fissure as a single artery (to become the anterior median spinal artery) |
Radicular arteries |
|
Anterior radicular arteries | Comprised of 2–17 arteries: Cervical 6, thoracic 2–4, lumbar 1–2 arteries Artery of Adamkiewicz: A major anterior radicular artery originating at the lower thoracic or upper lumbar spine (the largest); travels with the spinal roots Most frequent on the left side (75% of population) Joins the anterior spinal artery |
Posterior radicular arteries | Comprised of 10–23 arteries Divide at the posterolateral spinal cord surface and joins the paired posterior spinal arteries |
Fig. 1.14 Blood vessels supplying the spinal cord. Thoracic vertebra viewed from above. The spinal branches arise from the posterior branches of segmental arteries and divide into an anterior and posterior radicular artery. The radicular arteries supply the dorsal and ventral roots, and peripheral portions of the dorsal and ventral horns. They also communicate with the vasocorona. These arteries have a better developed connection with the anterior spinal artery at some levels and with the posterior spinal artery at other levels. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Karl Wesker.)
Fig. 1.15 Blood supply to the spinal cord segments. In each spinal cord segment, the anterior spinal artery gives off several (5–9) sulcal arteries that course posteriorly in the anterior median fissure. Typically, each sulcal artery enters one half of the spinal cord, supplying the anterior horn, base of the posterior horn, and anterior and lateral funiculi (approximately ⅔ of the total area) in that half; the sulcal arteries tend to alternate direction (left or right) to supply both halves of the spinal cord segment. The paired posterior spinal arteries provide the blood supply to the posterior third of the cord, including the posterior horn and funiculus. All three spinal arteries contribute numerous delicate anastomosing vasocorona on the pial surface of the spinal cord, which in turn send branches into the periphery of the cord. The sulcal arteries are end arteries within the spinal cord and their occlusion may produce clinical symptoms. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Karl Wesker.)
a. Derived from segmental vessels from the aorta, which includes the ascending cervical, deep cervical, intercostals, lumbar, and sacral arteries
b. Passes through the intervertebral foramina to divide into the anterior and posterior radicular arteries to supply the thoracic, lumbar, sacral, and coccygeal spinal segments
c. The anterior ramus of the segmental artery supplies the cord while the posterior ramus branches in the foramen supply the dorsal root ganglion (DRG) and nerve roots via anterior and posterior radicular branches
d. A single thoracic radicular artery (artery of Adamkiewicz) arises from the aorta at T7 (most vulnerable to low flow); 75% arise from T9–T12; 80% arise from the left
2. Posterior arterial system
a. Paired posterior spinal arteries form a leptomeningeal perimedullary network that anastomoses with the anterior system, most prominently at the level of the conus where the anastomotic loop is located.
b. Blood from the posterior medullary arteries flows centripetally in the perforating branches from the leptomeningeal system of the spinal cord surface to the posterior columns and posterior horns.
3. Anterior arterial system
a. Single midline artery that feeds into the anterior medullary artery in the anterior median fissure
b. Flows centrifugally via penetrating branches to the anterior and intermediate gray and via pial radial network to the white matter of the anterior and lateral funiculi
B. Regional arterial supply of the spinal cord
Level | Arterial Supply |
|---|---|
Cervical | Vertebral artery (proximal portion of the subclavian artery) Posterior inferior cerebellar artery Ascending cervical artery (from the thyrocervical trunk) Deep cervical artery (from the costocervical trunk) |
Thoracic | Thyrocervical and costocervical trunk Intercostal artery (aorta: T3–T11) Subcostal artery (aorta: T12) |
Lumbar | Lumbar artery (aorta L4–L5) |
Sacrum | Lateral sacral artery (internal iliac artery) supplies sacral neural elements. Middle sacral artery The aorta and iliac arteries send branches to the thoracolumbar spine. |
1. Segmental arteries → spinal branches (lies ventral to the root) pass through the intervertebral foramina → anterior or posterior radicular arteries → anterior or posterior spinal arteries.
D. Spinal cord ischemia
1. Most vulnerable at transitional regions where the arterial supply is derived from >1 source
2. Border zone region is especially vulnerable at T1–T4 and L1 (e.g., with an intercostal artery occlusion or an aortic dissection) anterior aspect of the spinal cord. Also vulnerable are areas between the anterior and posterior medullary arteries (between the intermediate and dorsal horns and lateral and posterior fasciculi).
E. Venous drainage of the spinal cord—highly variable, typically follows the arterial system
1. Both anterior spinal veins (located in the anterior sulcus) and the posterior spinal veins lie adjacent to the spinal arteries, which eventually drain into the intervertebral veins exiting the spinal canal via intervertebral foramina.
2. Anterior and posterior radicular veins
VI. Intracranial–Extracranial Anastomoses
A. Occipital artery ↔ vertebral (C1 and C2)
B. Ascending pharyngeal artery ↔ vertebral
C. Ascending pharyngeal artery ↔ ICA via petrous and cavernous branches
D. Facial artery (angular branch) ↔ ICA via angular branch of the facial artery to the orbital branch of the ophthalmic artery
E. Posterior auricular artery ↔ ICA via stylomastoid artery
F. Maxillary artery branch ↔ ICA via
1. MMA ↔ ethmoidal branch of the ophthalmic artery
2. Artery of foramen rotundum ↔ inferior lateral trunk
3. Accessory meningeal artery ↔ inferior lateral trunk
4. Vidian artery ↔ petrous ICA
5. Pharyngeal artery ↔ cavernous ICA
6. Temporal branches ↔ ophthalmic artery
7. Infraorbital artery ↔ ophthalmic artery
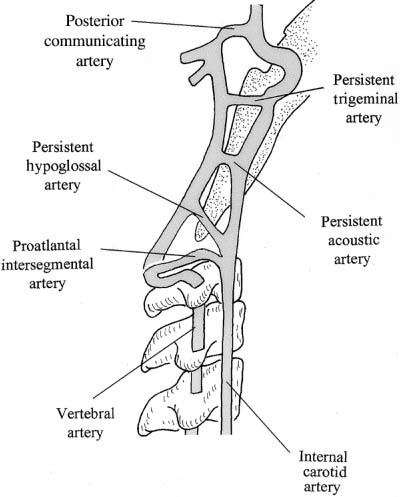
VII. Persistent Fetal Carotid–Basilar and Carotid–Vertebral Anastomoses (Fig. 1.1)
Anastomoses | Feature |
|---|---|
Primitive trigeminal | Most frequent persistent fetal circulation* (besides fetal PcommA) Present in 0.1 to 0.5% of angiograms Connects cavernous ICA with embryonic dorsal longitudinal neural arteries. Typically associated with hypoplastic PcommA and basilar and vertebral arteries proximal to the anastomosis. Increased frequency of aneurysms and AVMs (Fig. 1.17) Arises from: ICA just proximal to the cavernous sinus Meningohypophyseal trunk Curves medially to join basilar artery between SCA and AICA |
Persistent otic/acoustic | Extremely rare, first to disappear Connects petrous ICA via internal auditory meatus to the basilar artery Connects petrous ICA with embryonic dorsal longitudinal neural arteries |
Primitive hypoglossal | Second most frequent persistent fetal circulation, but much less common than the primitive trigeminal artery Present in 0.02–0.3% of angiograms Connects cervical ICA with embryonic dorsal longitudinal neural arteries: arises from the cervical ICA and connects to the basilar artery through the hypoglossal canal Typically bilateral hypoplastic vertebral arteries (thus, this primitive artery may be the main supply to the brainstem and cerebellum) |
Proatlantal intersegmental | Connects ECA or cervical ICA with embryonic dorsal longitudinal neural arteries Suboccipital anastomoses between cervical ICA and vertebral artery Courses between the arch of C1 and the occiput |
Abbreviations: AICA, anterior inferior cerebellar artery; AVMs, arteriovenous malformations; ECA, external carotid artery; ICA, internal carotid artery; PcommA, posterior communicating artery; SCA, superior cerebellar artery
VIII. Cortical Anatomy
A. General anatomy (Fig. 1.18, Fig. 1.19, Fig. 1.20, Fig. 1.21)
1. Contains 14 billion cortical neurons
2. Cells that develop later pass more superficially from the germinal zone and form connections with the cells they pass.
3. Cell types—stellate, fusiform, pyramidal (source of main output)
4. Neurotransmitters
a. Excitatory—glutamate and aspartate
b. Inhibitory—gamma-aminobutyric acid (GABA; stays in the cortex, augmented by barbiturates and anticonvulsants)
5. Neocortex—six layers, distinguished by cell density, type, and their arrangement of cells Allocortex—three layers, located in the olfactory cortex, hippocampus, and dentate gyrus
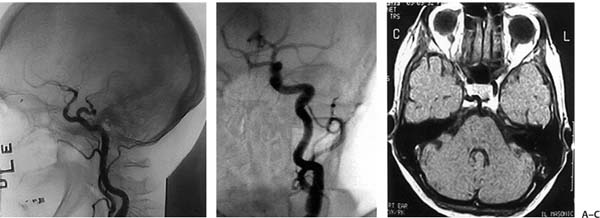
Fig. 1.16 Persistent fetal anastomoses between the anterior and posterior circulations.
Fig. 1.17 (A) Lateral and (B) anteroposterior catheter angiograms, and (C) axial T1-weighted magnetic resonance image of a persistent trigeminal artery.
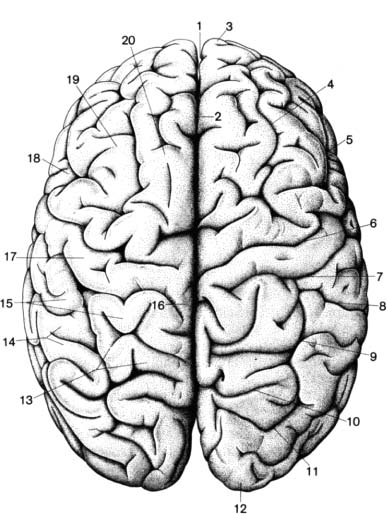
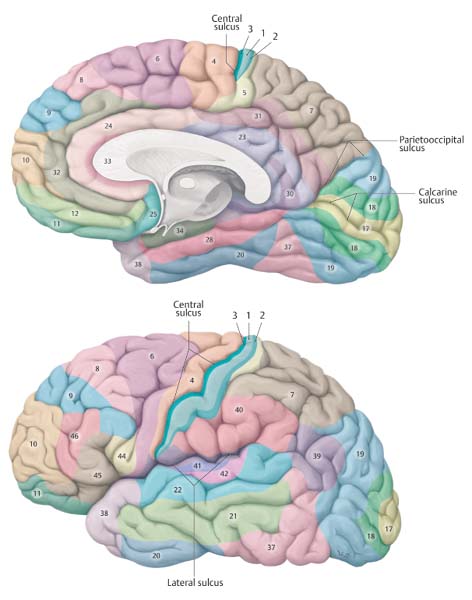
Fig. 1.18 Brain surface anatomy, superior view. 1. Longitudinal fissure of cerebrum. 2. Superior margin of cerebrum. 3. Frontal pole. 4. Superior frontal sulcus. 5. Inferior frontal sulcus. 6. Precentral sulcus. 7. Central sulcus. 8. Postcentral sulcus. 9. Intraparietal sulcus. 10. Parietooccipital sulcus. 11. Transverse occipital sulcus. 12. Occipital pole. 13. Superior parietal lobule. 14. Inferior parietal lobule. 15. Postcentral gyrus. 16. Paracentral lobule. 17. Precentral gyrus. 18. Inferior frontal gyrus. 19. Middle frontal gyrus. 20. Superior frontal gyrus. (From Frick H, Leonhardt H, Starck D. Human Anatomy 2. New York, NY: Thieme, 1991. Reprinted by permission.)
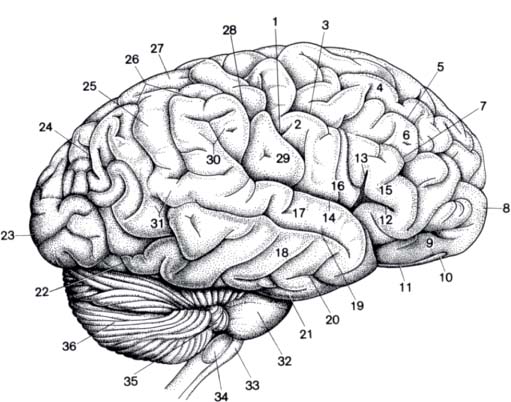
Fig. 1.19 Brain surface anatomy, right lateral view. 1. Central sulcus. 2. Precentral gyrus. 3. Precentral sulcus. 4. Superior frontal gyrus. 5. Superior frontal sulcus. 6. Middle frontal gyrus. 7. Middle frontal sulcus. 8. Frontal pole. 9. Orbital gyri. 10. Olfactory bulb. 11. Olfactory tract. 12–14. Lateral sulcus. 12. Anterior ramus. 13. Ascending ramus. 14. Posterior ramus. 15. Frontal operculum. 16. Frontoparietal operculum. 17. Superior temporal gyrus. 18. Middle temporal gyrus. 19. Superior temporal sulcus. 20. Inferior temporal sulcus. 21. Inferior temporal gyrus. 22. Preoccipital notch. 23. Occipital pole. 24. Transverse occipital sulcus. 25. Inferior parietal lobule. 26. Intraparietal sulcus. 27. Superior parietal lobule. 28. Postcentral sulcus. 29. Postcentral gyrus. 30. Supramarginal gyrus. 31. Angular gyrus. 32. Pons. 33. Pyramid (medulla oblongata). 34. Olive. 35. Flocculus. 36. Cerebellar hemisphere. (From Frick H, Leonhardt H, Starck D. Human Anatomy 2. New York, NY: Thieme;1991. Reprinted by permission.)
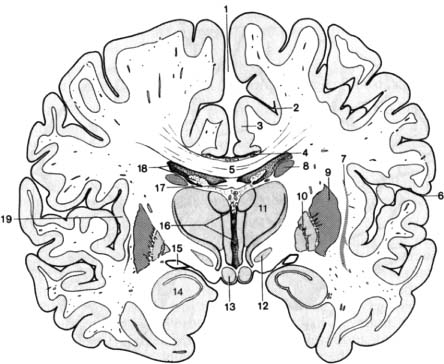
Fig. 1.20 Coronal section through the brain. 1. Longitudinal fissure of cerebrum. 2. Cingulate sulcus. 3. Cingulate gyrus. 4. Sulcus of corpus callosum. 5. Corpus callosum. 6. Lateral sulcus. 7. Claustrum. 8–9. Corpus striatum. 8. Caudate nucleus. 9. Putamen. 9–10. Lentiform nucleus. 10. Globus pallidus. 11. Thalamus. 12. Subthalamic nucleus. 13. Mamillary body. 14. Amygdala. 15. Optic tract. 16. Third ventricle and choroid plexus. 17. Body of fornix. 18. Lateral ventricle and choroid plexus. 19. Cortex of insula. (From Frick H, Leonhardt H, Starck D. Human Anatomy 2. New York, NY: Thieme; 1991. Reprinted by permission.)
Fig. 1.21 Brain surface anatomy, view of medial surface of right hemisphere. 1. Frontal pole of frontal lobe. 2. Medial frontal gyrus. 3. Cingulate sulcus. 4. Sulcus of corpus callosum. 5. Cingulate gyrus. 6. Paracentral lobule. 7. Precuneus. 8. Subparietal sulcus. 9. Parietooccipital sulcus. 10. Cuneus. 11. Calcarine fissure. 12. Occipital pole of occipital lobe. 13–16. Corpus callosum (cut surface). 13. Rostrum. 14. Genu. 15. Body. 16. Splenium. 17. Lamina terminalis (cut surface). 18. Anterior commissure (cut surface). 19. Septum pellucidum. 20. Fornix. 21. Tela choroidea of third ventricle. 22. Choroid plexus of third ventricle (cut edge). 23. Transverse cerebral fissure. 24. Thalamus. 25. Interthalamic adhesion (cut surface). 26. Interventricular foramen of Monro. 27. Hypothalamus. 28. Suprapineal recess and pineal body (cut surface). 29. Vermis of cerebellum (cut surface). 30. Cerebellar hemisphere. 31. Choroid plexus of fourth ventricle. 32. Medulla oblongata (cut surface). 33. Fourth ventricle. 34. Pons (cut surface). 35. Tectal lamina (cut surface) and mesencephalic aqueduct of Sylvius. 36. Mamillary body. 37. Oculomotor nerve. 38. Infundibular recess. 39. Temporal lobe lateral occipitotemporal gyrus. 40. Rhinal fissure. 41. Hypophysis (cut surface) with adenohypophysis (anterior lobe) and neurohypophysis (posterior lobe) of pituitary gland. 42. Optic chiasm (cut surface). 43. Optic nerve. 44. Olfactory bulb and tract. (From Frick H, Leonhardt H, Starck D. Human Anatomy 2. New York, NY: Thieme; 1991. Reprinted by permission.)
B. Neocortical layers (Fig. 1.22)
Layer | Feature | Fibers and Projections | |
|---|---|---|---|
Molecular | I | Most superficial layer Contains horizontal axons, Golgi type II cells, terminal dendritic processes | Receives diffuse afferent fibers from the lower brain to control the excitability of the region |
External granular | II | Contains closely packed granule cells Poorly myelinated |
|
External pyramidal | III | Contains pyramidal neurons, granule cells, and Martinotti cells | Commissural fibers to connect the two hemispheres Ipsilateral cortico-cortico association fibers |
Internal granular | IV | Contains closely packed stellate cells Dense horizontal myelinated plexus forms the external band of Baillarger | Main sensory input Enlarged in the sensory cortex |
Internal pyramidal | V | Contains the largest cells (Betz cells) Contains pyramidal neurons, granule cells, and Martinotti cells Dense myelinated plexus forms the internal band of Baillarger | Main efferents to the brain stem and spinal cord Enlarged in the motor cortex |
Multiform | VI | Contains spindle-shaped cells | Efferent fibers to the thalamus |
Fig. 1.22 Isocortex layers. 1. Molecular layer. 2. External granular layer. 3. External pyramidal layer. 4. Internal granular layer. 5. Internal pyramidal layer. 6. Multiform layer. 1–3. External principle zone. 4–6. Internal principle zone. (From Frick H, Leonhardt H, Starck D. Human Anatomy 2. New York, NY: Thieme; 1991.)
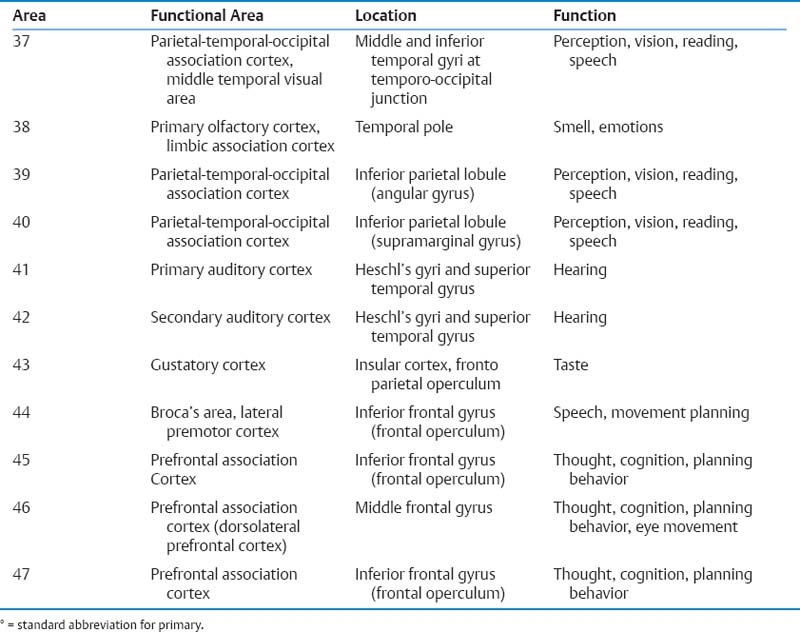
C. Brodmann’s areas (Fig. 1.23)
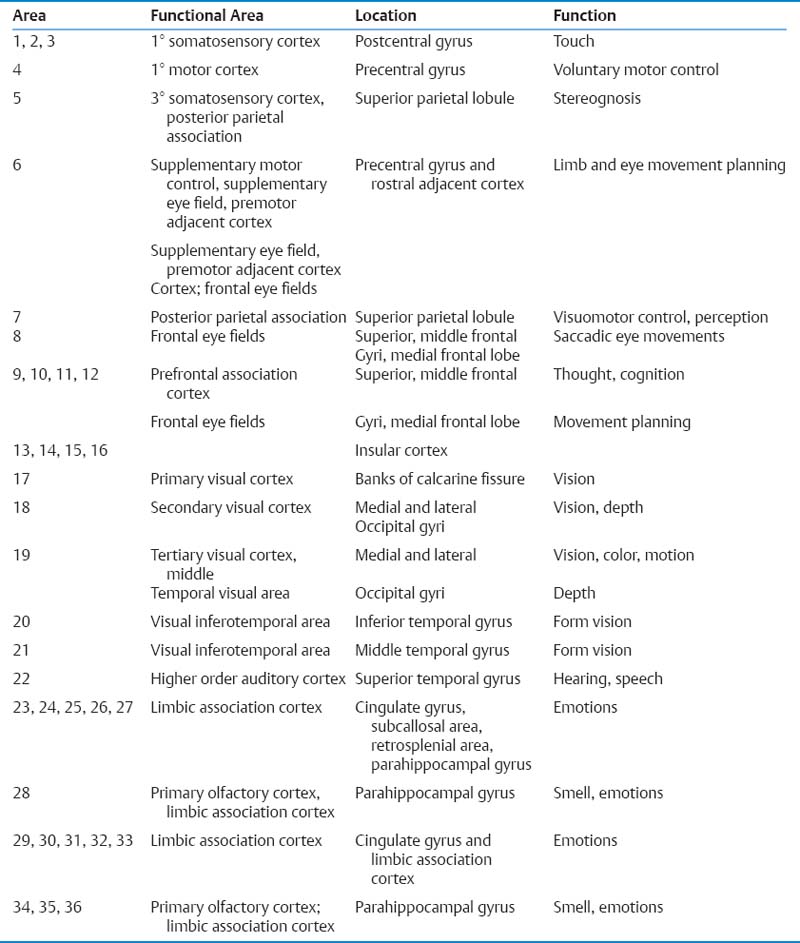
Fig. 1.23 Brodmann areas in the neocortex. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
1. Main sensory areas—somatosensory area (areas 3, 1, 2), visual area (area 17), auditory area (areas 41, 42), gustatory area (area 43), and olfactory area (multiple Brodmann areas, not distinctly localized)
2. Sensory cortex
Sensory Area | Feature |
|---|---|
Primary somatosensory area (S1) | Postcentral gyrus (areas 3,1,2) Input: VPLc and VPM thalamic nuclei (medial lemniscus, spinothalamic, and trigeminothalamic tracts) Input for area 3a: muscle spindles Input for area 3b: cutaneous (skin) Input for area 1: muscle spindles and skin Input for area 2: deep (joint) receptors Course: ML/STT → VPLc/VPM → S1 Face and tongue have bilateral representation (Fig. 1.24). |
Secondary somatosensory area (S1) | Located on the superior bank of the lateral sulcus Input: ipsilateral VPLc and VPM thalamic nuclei Input: bilateral S1 Output: ipsilateral S1 and motor cortex Information is bilateral and the homunculus is inverted (face rostral), processing of the thalamic tracts but not medial lemniscus |
Somatosensory association area | Superior parietal lobule (areas 5, 7) Integrates sensory data; lesion causes tactile agnosias or astereognosis |
Primary visual cortex (V1; area 17) | Located in the walls and floors of the calcarine sulcus, extends around the occipital pole Input: LGB → geniculocalcarine fibers pass close to the outer wall of the lateral ventricles (external sagittal stratum) → calcarine sulcus Output: internal sagittal stratum → corticofugal fibers → superior colliculus and LGB Macula → posterior ⅓ of the calcarine cortex (occipital pole) Vertical meridian has commissural fibers for bilateral representation. Ganglion cell receptive field—a region of the retina that affects the firing of one retinal ganglion cell. It is either “on-center and off-surround” or “off-center and on-surround.” These cells fire at a constant steady rate. LGB also has “on and off” areas that contribute to visual processing. The cortex no longer has concentric receptive fields. The ocular dominance columns have alternating right and left stripes. Orientation columns each represent 180 degrees. Band of Baillarger in the striate cortex is the stripe of Gennari visible to the naked eye; are collaterals of the primary visual cortical axons (the recognizable layer IVb on myelin-stained sections due to dense plexus of myelinated axons) |
Secondary visual cortex (V2, V3; areas 18, 19) | Input: LGB and pulvinar V2 = area 18, V3 = area 19 (more lateral) Lesion causes visual agnosia |
Transverse gyri of Heschl located in the superior temporal gyrus, buried in the temporal operculum of the sylvian fissure; the first cortical structure for auditory information processing The association area 42 surrounds area 41. Input: MGB with fibers that pass through the sublenticular IC Ventral MGB has tonotopic organization (high frequencies medial). Dorsal and medial MGB → ipsilateral area 41 Isofrequency cell columns are present in the cortex. Each cochlea projects bilaterally but more to the contralateral side. Trapezoid body—the only auditory commissure needed for sound localization Unilateral lesion—bilateral partial deafness, but mostly contralateral Area 22 lesion (dominant hemisphere): word deafness or sensory aphasia with normal hearing | |
Gustatory area (area 43) | In the postcentral operculum adjacent to the tongue sensory area Input: ipsilateral nucleus solitarius → VPMpc → area 43 |
Vestibular cortex | Located in the inferior parietal lobule near S1 (head) Bilateral representation, slightly more contralateral |
Abbreviations: IC, internal capsule; LGB, lateral geniculate body; MGB, medial geniculate body; ML, medial lemniscus; STT, spinothalamic tract; VPLc, ventroposterolateral pars caudalis; VPM, ventroposteromedial; VPMpc, ventroposteromedial pars compacta
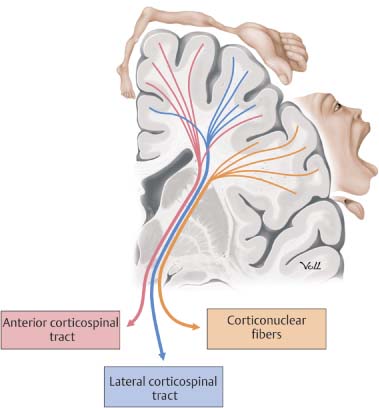
Fig. 1.24 Motor homunculus. Coronal section anterior view of the left hemisphere. Axons for the head area are the corticonuclear fibers and the corticospinal fibers split into lateral and anterior corticospinal tracts below the diencephalon. (From THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, Illustration by Markus Voll.)
1. Main motor areas—primary motor (area 4), premotor (area 6a), supplemental motor (areas 6a), frontal eye fields (area 8)
2. Motor cortex
Motor Cortex | Feature |
|---|---|
Primary motor cortex M1 (area 4) | Precentral gyrus, involved in voluntary motor control, the thickest cortex Pyramidal cells of Betz (layer V) make up 3% of the corticospinal fibers. Output includes corticobulbar and corticospinal fibers: From area 4 (31%), area 6 (29%), and parietal cortex 40% Not somatotopic Unilateral projection, except bilateral to the eye, face, tongue Columns may be present (like those of the visual and somatosensory cortex) Neurotransmitters—glutamate and aspartate (±) |
Premotor cortex (area 6a) | Voluntary motor control for responses dependent on sensory input Located on the lateral aspect of the cortex, anterior to area 4 Input: cortical, VL and VA thalamic nuclei Unilateral lesion: no deficit |
Supplemental motor cortex M2 (area 6a) | Programming, planning, and initiating of motor movements Somatotopic organization of neurons Located on the medial aspect of the hemisphere anterior to area 4, medial superior frontal gyrus Input: bilateral Output: ipsilateral areas 4, 6, 5, and 7, contralateral M2, bilateral spinal cord, caudate, putamen, and thalamus Lesion—hemiparesis/plegia, diminished spontaneous speech, may have volitional movement with effort |
Frontal eye fields (area 8) | Rostral to the premotor area (caudal middle frontal gyrus) Initiate saccades—stimulation causes contralateral eye deviation Occipital eye center (area 17) controls ipsilateral pursuit. Eye fields do not reach CNs III, IV, and VI nuclei directly, but goes to: Rostral interstitial nucleus of the MLF Interstitial nucleus of Cajal Paramedian pontine reticular formation Superior colliculus Lesion causes impaired saccades, especially in the dominant hemisphere. |
Abbreviations: CN, cranial nerve; MLF, medial longitudinal fasciculus; VA, ventroanterior; VL, ventrolateral
F. Input to the motor area
1. Ipsilateral thalamic VL and ventrolateral pars oralis (VLo) → M1
2. Contralateral cerebellum → M1
3. Medial globus pallidus (GP) → ipsilateral thalamic ventroanterior pars compacta (VApc), VLo, centromedial (CM) → M2 and premotor cortex (not M1)
4. S1 (all but area 3) to all of the motor cortex
5. M2 → M1 and premotor cortex
6. Motor cortex has reciprocal fibers with the thalamus (except for thalamic reticular nuclei, which receives afferent fibers from the entire cortex but does not send them back.
G. Cerebral dominance
Dominant Hemisphere | Nondominant Hemisphere |
|---|---|
Usually left hemisphere | Usually right hemisphere |
Language, math, analytical thought Sign language mainly left hemisphere | Spatial analysis, face recognition, music, emotion Pictures may communicate language to the nondominant hemisphere, but letters require the dominant hemisphere for analysis. |
Lesions in the dominant angular and supramarginal gyri: Gerstmann’s syndrome: Right/left dissociation, finger agnosia, acalculia, Fail to appreciate the existence of hemiparesis agraphia | Lesion in the nondominant inferior parietal lobule: Failure to recognize a side of the body (neglect) Fail to appreciate the existence of hemiparesis |
Handedness: Right-handed individuals are nearly always left-brain language dominant. Left-handed individuals are usually left-brain language dominant: 85%: left hemisphere dominance, 15%: bilaterally dominant Rare: right hemisphere dominance Men are more frequently left-handed, dyslexic, and prone to stutter. Handedness may be determined by testosterone during brain development. | |
H. Cerebral topography
Fissure | Surface marking |
|---|---|
Sylvian fissure | Localization: 1. Mark a point ¾ of the way on a line over the superior sagittal sinus from the nasion to the inion. Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|