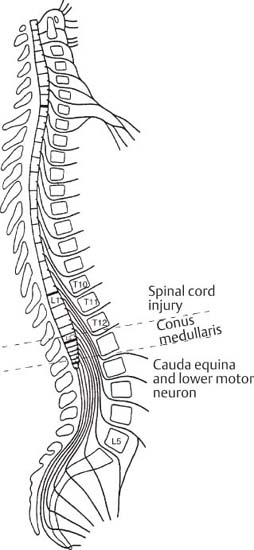
I 1 Anatomy and Surgical Approaches 2 History and Physical Examination 3 Spinal Imaging and Diagnostic Tests 4 Biomechanics of the Spine and Spinal Instrumentation 5 Physiology of Bone Grafts and Bone Graft Substitutes I. Vertebral Column A. The spinal column has specifically adapted anatomic features to maintain stability, protect neural elements, and allow range of motion. B. Stability is augmented by the intervertebral disks, ligaments, and muscles. C. There are 33 vertebrae in the spinal column (seven cervical, 12 thoracic, five lumbar, five sacral, and four coccygeal). D. There are four sagittal curves in the vertebral column. 1. Cervical lordosis 2. Thoracic kyphosis 3. Lumbar lordosis 4. Sacral kyphosis E. The kyphotic curves are called primary because they form during the fetal period. 1. Caused by the wedge-shaped nature of vertebrae F. The lordotic curves are called secondary because they begin to form during the late fetal period and continue to form after birth. Head and body weight contributes to their formation. 1. Caused by differences in the anteroposterior (AP) dimensions of the intervertebral disks. G. Each vertebra consists of a posterior bony arch and an anterior body, both of which surround the vertebral canal. Posterior bony arches between two adjacent vertebrae form a foramen for the spinal nerve roots. Anterior bodies of the lumbar spine support 80% of the axial load on the spinal column. H. Posterior bony arch components 1. Pedicles and laminae a. Form the borders of vertebral canal with the posterior border of the vertebral body 2. Spinous and transverse processes a. Attachment sites for supporting ligaments and muscles 3. Articular processes a. Pars interarticularis is the bony region between superior and inferior articular process an individual vertebra. b. Facet joints between articular processes of adjacent vertebrae support 20% of axial load on the spinal column. II. Intervertebral disks A. Located between vertebral end plates, which are covered by hyaline cartilage and supported by subchondral bone B. The inside of the disk contains the nucleus pulposus, which cushions the axial load. This nucleus is made of mucoid type II collagen. C. The disk is a relatively avascular structure with the outer layers receiving nutrients from the end arterioles and the central portions receiving nutrients by diffusion from vertebral end plates D. Anulus fibrosus 1. Outer portion of the disk 2. Made of type I collagen 3. Lattice made of sheets running in opposite direction that give the disk greater rotational strength 4. Thickest portion is anterior. Thinnest is posterolateral. 5. Outer portions of anulus are continuous with the anterior and posterior longitudinal ligaments. E. Vertebral disks make up one quarter of the spinal column height. The disks expand when the column is horizontal because water and nutrients enter the disk, but they collapse under the stress of prolonged standing. I. Spinal cord A. Gross structure 1. Spinal cord ends at L1-L2 (conus medullaris) a. It may be as high as T12 or as low as L2-L3 b. In newborn infants, the cord ends at L2-L3 2. Length: 45-cm cord and 25-cm filium terminale (10% increase in length with flexion, mostly at C1, T1, and L1, least at C6 and T6) 3. Mean diameter (10 mm, frontal larger than sagittal) 4. Relationship between cord and vertebral segments (Fig. 1–1) (Table 1–1) B. Internal structures (Fig. 1–2) 1. The peripheral white matter and central gray matter a. Gray matter: cell bodies of efferent neurons (1) Posterior horns: somatosensory (2) Anterior horns: somatomotory (3) Intermediolateral horns: visceral (4) Reflex somatic centers
Patient Evaluation and Spine Overview
1
Anatomy and Surgical Approaches
♦ Basic Anatomy of the Spine
♦ Neuroanatomy
| Cord Segment | Vertebral Segment |
| C1 | C1 |
| C8 | C7 |
| T6 | T5 |
| T12 | T8 |
| L2 | T10 |
| L5 | T11 |
| S3 | T12 |
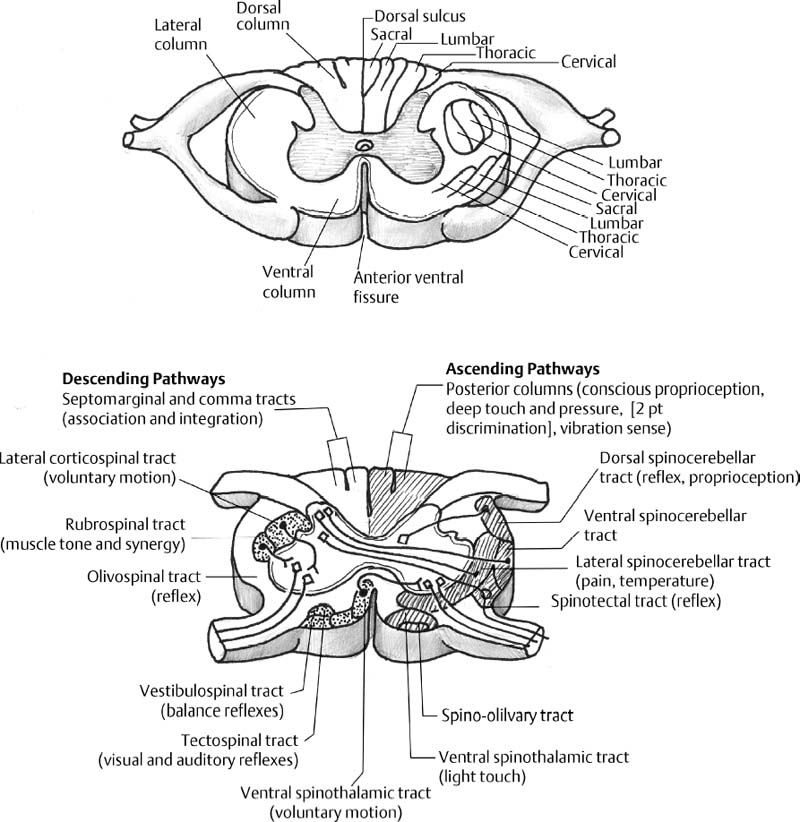
b. White matter: nerve fibers and glia
(1) Posterior funiculus: posterior columns (fasciculus cuneatus laterally and gracilis medially)
(2) Lateral funiculus: lateral corticospinal and lateral spinothalamic fasciculus
(3) Anterior funiculus: anterior spinothalamic tract
2. Central ependymal canal: passage of cerebrospinal fluid
1. Motor function: cerebral cortex, internal capsule, corticospinal tract, pyramidal tract (90% decussate at the medulla to the contralateral lateral corticospinal fasciculus), anterior horn cells
a. Lateral corticospinal fasciculus: tracts for the upper extremities are medial to the lower extremities
b. Central cord syndrome: spares the most lateral tracts in the lateral corticospinal fasciculus (upper extremity motor function) and retains the medial tracts (lower extremity motor function)
2. Sensory function
a. Posterior columns: tactile discrimination, proprioception, and vibration sense (stereognosis, two-point discrimination)
(1) Fasciculus gracilis: lower limbs and above midthorax
(2) Fasciculus cuneatus: upper limbs and below midthorax
(3) Sensory tracts cross to the opposite side in the medulla oblongata and to the sensory cortex
(4) Anterior cord syndrome: only posterior column functions are spared.
b. Lateral spinothalamic fasciculus: pain, temperature, and light touch
(1) Most fibers cross through the ventral commissure to the opposite side and ascend through the lateral spinothalamic tract.
(2) Brown-Sequard syndrome: pain and temperature loss is contralateral, whereas motor and proprioception loss are ipsilateral.
c. Anterior spinothalamic fasciculus
(1) Crude touch
(2) Posterior cord syndrome: only crude touch is spared
D. Vascularity of the spinal cord
1. Cervical spine
a. The anterior spinal artery: the major vessel for anterior and central aspects of the cord
(1) Two medullary feeders at the brain stem by the vertebral arteries
(2) Other medullary feeders from the vertebral arteries and ascending cervical arteries, particularly C2 and C6 from the left and C2, C5, C6 from the right
b. Two posterior spinal arteries from the posterior inferior cerebellar arteries have minimal contribution to the central gray matter.
2. Thoracolumbar spine
a. The anterior spinal artery, two posterior spinal arteries
b. Feeders
(1) Superior intercostal artery: branch of deep cervical artery, which is a branch of the right subclavian artery, feeds the cord at the cervical-thoracic junction.
(2) One to five segmental vessels: tenuous blood supply for the upper thoracic cord (watershed critical zone from T4 to T10)
(4) Anastomotic loop of the conus medullaris from aortic segmental and lateral sacral arteries
3. Venous drainage (azygos and hemizygous veins)
a. Veins of the spinal cord anteriorly and posteriorly
b. Batson’s plexus: from basiocciput to the coccyx
c. Clinical significance: metastatic dissemination and infections
II. Spinal meninges (Fig. 1–3)
A. Dura mater: outer covering of the spinal cord
B. Leptomeninx: pia mater (outer lining of the cord) and arachnoid membrane (transparent sheet containing the cerebrospinal fluid)
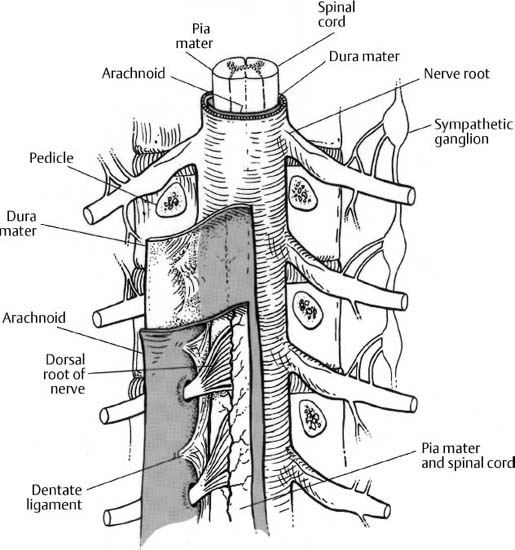
Figure 1–3 Cross section of the spinal cord and meninges. The spinal cord is covered by the pia mater, which is the outer lining of the cord, and transparent arachnoid mater that contains the cerebrospinal fluid. The dura mater is the outer covering of the spinal cord. The spinal cord is anchored to the dura by the dentate ligaments that project laterally from the lateral side of the cord to the arachnoid and dura at points midway between exiting spinal nerves. (From An HS. Principles and Techniques of Spine Surgery. Baltimore: Williams and Wilkins; 1998. Reprinted with permission.)
D. Septum posticum between pia and arachnoid on the dorsal aspect from lower cervical to conus regions
E. Epidural space: space between the bone and dura
1. Space: 2 mm at L3-L4, 4 mm at L4-L5, 6 mm at L5-S1
2. Plica mediana dorsalis durae matris: a median fold at the lumbosacral region
F. Termination of dura/arachnoid envelope varies from S1-S2 to S2-S3, and dura invests the filium terminale and attaches to the coccyx.
III. Spinal nerves
A. Thirty-one pairs of spinal nerves: eight cervical, 12 thoracic, five lumbar, five sacral, one coccygeal
B. Spinal root nerve consists of motor and sensory rootlets, dorsal root ganglion, and spinal nerve.
1. Sympathetic connections by preganglionic (white) rami and unmyelinated postganglionic (gray) rami
2. Branches: sinuvertebral nerve to the anulus of the disk, and dorsal ramus for facets and posterior muscles
a. Sinuvertebral nerve runs back into the spinal canal through the foramen, running cranial to the disk. The gray rami from the sympathetic ganglion join the ventral primary rami. The anterior portion of the lumbar intervertebral disk is innervated by sympathetic fibers, whereas the posterior portion of the disk is innervated by the sinuvertebral nerve. The sinuvertebral nerves innervate the posterior longitudinal ligament, the posterior part of the anulus, and the ventral part of the dura. The sinuvertebral nerves typically ascend to innervate the superior disk as well.
b. The dorsal primary rami gives medial (innervates facet joints above and below, segmental muscles, and interspinous ligament), lateral (innervates iliocostalis muscle), and occasionally intermediate (innervates longissimus muscle) branches.
C. C1 nerve emerges above C1 vertebra, and C8 emerges above T1 vertebra. In the thoracic and lumbar regions, the spinal nerves emerge beneath the pedicles bearing the same number.
D. Spinal nerves in the intervertebral foramina
1. Cervical spine: no intervertebral foramen for C1 and C2, and C3-C8 escape through corresponding foramina occupying ~75% of space.
2. Thoracic spine: thoracic spinal nerves are small and occupy 20% of the foramen and exit below the pedicle.
3. Lumbar spine: large lumbar nerves occupy 33% of the foramen and exit obliquely below the pedicle.
4. Sacrum: anterior rami emerge through the anterior sacral foramina, and posterior rami through the posterior sacral foramina.
E. Dermatomes and myotomes (Fig. 1–4)
1. Motor: C4 (spontaneous breathing and shrug shoulders), C5 (deltoids and biceps), C6 (wrist extension), C7 (triceps and wrist flexion), C8 (finger flexion), T1 (intrinsics), L2 (iliopsoas), L3 (quadriceps), L4 (tibialis anterior), L5 (EHL) Extensor Hallvcis Longus, S1 (gastrocnemius), S2 (bladder sphincter), S3 (anal sphincter)

Figure 1–4 Illustration of anterior and posterior dermatomes. (From An HS. Principles and Techniques of Spine Surgery. Baltimore: Williams and Wilkins; 1998. Reprinted with permission.)
F. Dynamics
1. L5 or S1 nerve roots may slide up to 1 cm during flexion-extension
2. The spinal cord and nerve roots generally stretch in flexion and relax in extension, but the spinal canal and foramen enlarge in flexion and narrow in extension.
G. Cauda equina
1. Lumbar and sacral roots are organized in a specific pattern.
2. Fifty percent compression of the thecal sac leads to dysfunction.
H. Nerve root anomalies (Kadish and Simmons)
1. Type I: intradural anastomosis
2. Type II: anomalous origin of nerve roots
3. Type III: extradural anastomosis
4. Type IV: extradural division
I. Vasculature of nerve root
1. Proximal and distal radicular arteries anastomosis in the proximal one third of the root in the foramen, which may be a vascular deficient area
2. Intrinsic vasculature: interfascicular and intrafascicular vessels with compensating coils and arteriovenous anastomosis allow considerable interfascicular motion and stretch of the root.
3. Thin pia allows exchange of metabolites with cerebrospinal fluid.
4. Mechanical compression causes vascular compression, which manifests in neuroischemic claudication clinically.
K. Plexus
1. Cervical and brachial plexus
a. The ventral rami of C1-C4 form the cervical plexus
b. The anterior rami of C5-T1 form the brachial plexus
2. Sacral plexus
a. Lumbosacral trunk (L4, L5) and S1, S2, S3, and S4 anterior rami
b. Sciatic (L4-S3) and pudendal (S2-S4) nerves
c. Branches: superior gluteal (L4-S1), inferior gluteal (L5-S2), nerve to obturator internus, nerve to quadratus femoris (L5-S2), and posterior cutaneous nerve of the thigh (S1-S3)
d. Anterior coccygeal plexus: S5 and coccygeal anterior rami to become anterior caudal nerve
IV. Autonomic systems (sympathetic and parasympathetic systems)
A. Sympathetic centers
1. C8 to L4 spinal cord
2. Sympathetic trunk and ganglions: cervical to sacral
3. Cardioaccerelator center, sweat glands, vasomotor, bronchopulmonary, abdominal splanchnic, anorectal/bladder continence, and ejaculation center
4. Loss of sympathetic system
b. Horner’s syndrome: drooping of upper eyelid (ptosis), enophthalmos, contraction of the pupil (miosis), absence of sweating (anhydrosis) (injury to cervical or first thoracic sympathetic chain)
c. Urogenital problems: retrograde ejaculation due to improper closing of the bladder neck (injury to the hypogastric plexus)
d. Autonomic dysreflexia
(1) Spinal cord injury above sympathetic splanchnic visceral outflow (T6)
(2) Hypertension, sweating, headache, flushing (return of reflex)
B. Parasympathetic systems: brain stem and sacral spinal cord (visceral and penile erection functions)
♦ Surgical Anatomy (Figure 1–5)
I. Cervical spine
A. Bony anatomy
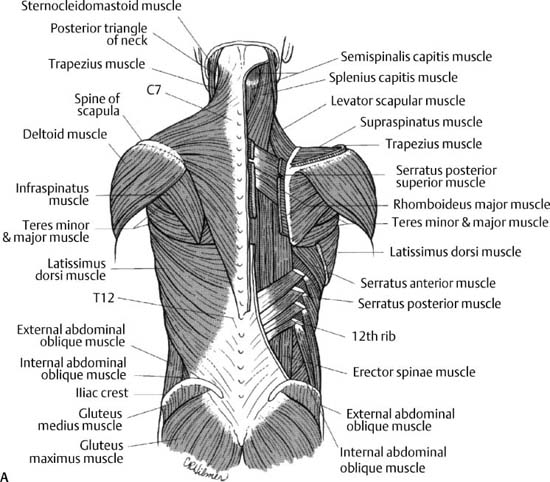
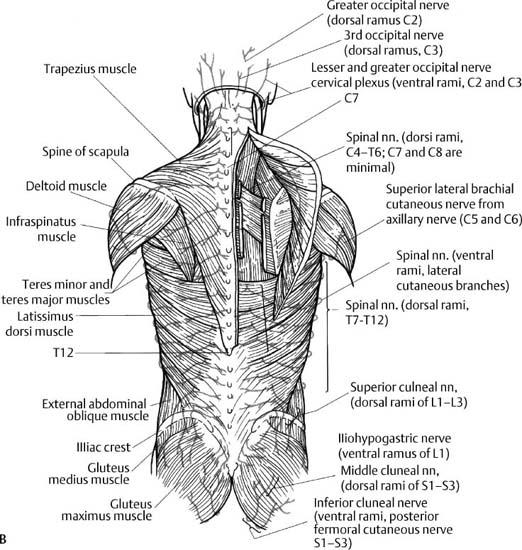
Figure 1–5 The human spine. (A) Posterior musculature of the spine. (B) Posterior musculature of the spine. n., nerve; (From An HS. Principles and Techniques of Spine Surgery. Baltimore: Williams and Wilkins; 1998. Reprinted with permission.)
a. Posterior neural arch fuses at 3 years and anterior neural arch (two sites) fuses at 7 years
b. The atlas has large transverse processes, where the superior and inferior oblique muscles attach. The transverse foramen is located within the transverse process, through which the vertebral artery passes.
c. Posterior arch has groove along its superior border for vertebral artery that runs along it on its way to the foramen magnum of the skull.
e. Inferior articular facet contributes to the atlantoaxial joint.
2. Axis: odontoid process with oval articular facet anteriorly, making a synovial joint with the anterior arch facet and large spinous process (rectus major and inferior oblique muscle attachment)
a. Synchondrosis between the dens and arch and neurocentral cleft between the body and arch fuse at 3 to 6 years
b. The pedicle of axis is large and projects medially at 30 degrees and superiorly at 20 degrees.
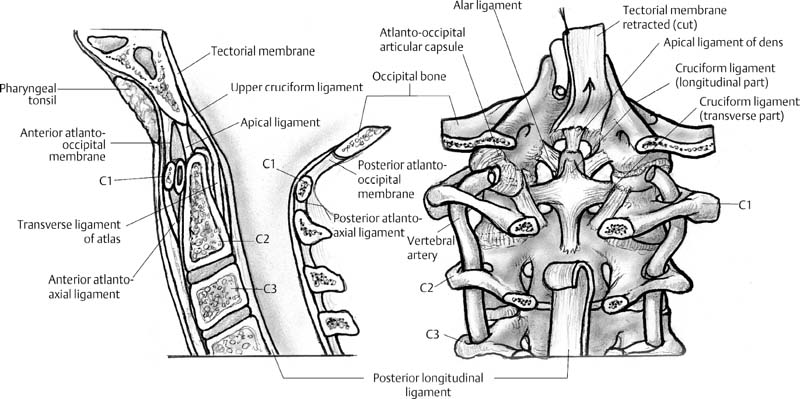
c. Transverse ligament secures dens to the anterior arch of the atlas. Extension of this ligament superiorly and inferiorly creates the cruciform ligament.
d. Responsible for the majority of cervical rotation around the axis.
e. Alar ligaments
1. Connect odontoid to the occipital condyles, further stabilizing the joint
f. Transverse processes also contain the transverse foramen with the vertebral artery.
3. C3-C6 vertebrae: bifid spinous processes, pedicle, laminae, articular processes, lateral mass (between the articular processes), transverse processes with anterior and posterior tubercles and transverse foramen (“carotid tubercle for C6 anterior tubercle and vertebral artery in the foramen”), uncinate processes (“joints of Luschka”), and triangular vertebral foramen
a. Superior surfaces of cervical vertebrae are concave, and the inferior surfaces are convex.
b. Cervical vertebrae have small bodies compared with the vertebral canal.
c. Facets gradually become steeper and oriented more sagittally as one progresses down the cervical spine.
1. Lateral masses are bony regions between the cervical facets just lateral to the laminae.
d. Vertebral artery travels within the transverse foramina, dividing it into posterior and anterior tubercle between which passes the exiting nerve root.
4. C7 vertebra: large, thick spinous process and not bifid
a. Transitional vertebra with unique characteristics
b. Inferior surface larger than superior surface
c. Taller and shallower lateral masses
d. Pedicles enlarge starting with C7 and going down the spine.
e. Spinous process is the site of attachment of the ligamentum nuchae
f. Has transverse foramina but vertebral artery only passes through them in 5% of the patients.
B. Ligamentous anatomy and articulation
1. Atlanto-occipital articulation: articulation between the condyles of occipital bone superior facets of the atlas, supported by anterior and posterior occipital membranes (continuation of anterior longitudinal membranes and ligamentum flavum respectively), and capsule (flexion, extension, and lateral motion)
2. Atlantoaxial articulation (Fig. 1–6)
a. Rotational movement between the odontoid process and anterior arch of the atlas (responsible for 50% of cervical rotation)
b. Ligaments
(1) Anterior and posterior atlantoaxial ligaments
(2) Transverse ligament: across the arch of atlas to hold dens against anterior arch of atlas (cruciform ligament of atlas: transverse ligament plus superior and inferior extension)
(3) Alar ligament (sides of dens to condyles of occipital bone) and apical ligament (from apex of dens to foramen magnum as remnant of notochord in this area)
(4) Tectoral membrane: continuation of the posterior longitudinal membrane
3. C2-C7 articulation
a. Flexion and extension motion
b. Facet joint and capsule: horizontal plane (45 degrees oblique) of the joint and weak capsule allow more mobility than lumbar and thoracic vertebrae
c. Ligaments
(1) Anterior and posterior longitudinal ligaments
(2) Ligamentum flava: from posterior aspect of lamina below to anterior aspect of lamina above with deficiency in the midline
(3) Interspinous ligament: oblique orientation from posterior superior aspect to anterior inferior aspect
(4) Supraspinous ligament
(5) Ligamentum nuchae: fibroelastic septum from the occiput to C7
d. Intervertebral disks: anulus fibrosus and nucleus pulposus
C. Muscles
1. Posterior muscles
a. Superficial: trapezius (from external occipital protuberance and C7 to T12 spinous processes to insert at lateral clavicle, acromion, and spine of scapula)
b. Intermediate: splenius capitis and cervicis
c. Deep: semisplenius capitis, semisplenius cervicis, and mutifidus with rotators
2. Suboccipital muscles
a. Rectus capitis posterior major: C2 spinous process to inferior nuchal line
b. Rectus capitis posterior minor: C1 posterior tubercle to inferior nuchal line
c. Obliquus capitis inferior: C2 spinous process to transverse process of C1
d. Obliquus capitus superior: C1 transverse process to occipital bone between superior and inferior nuchal lines