Fig. 1
Case 1: 68-year-old man with acute SAH caused by ruptured left posterior communicating artery aneurysm (arrow) with Hunt & Hess grade II, World Federation of Neurosurgical Societies (WFNS) grade I, and Fisher grade 4. On the same day, the patient underwent microsurgical occlusion of the aneurysm. The intraoperative angiogram illustrated severe iCVS (53.2 % stenosis) in the left A1 segment (arrow heads)
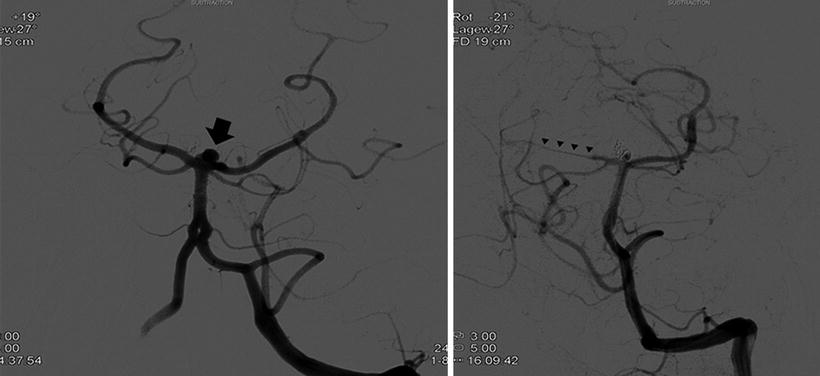
Fig. 2
Case 2: 51-year-old woman with acute SAH caused by a ruptured basilar tip aneurysm (arrow) with Hunt & Hess grade IIb, WFNS grade II, and Fisher grade 4. On the same day, she underwent coiling of the ruptured aneurysm. The angiogram demonstrated severe iCVS (62.9 % stenosis) of the right posterior cerebral artery (arrow heads)
Discussion
The incidence of iCVS in patients undergoing treatment for ruptured intracranial aneurysms has been underestimated, especially during surgical occlusion of ruptured aneurysms. In the present series, we found a rate of iCVS of 30 % in clipped patients and 14 % in coiled patients with SAH. Although this finding fell short of statistical significance (p = 0.07), there was a trend toward a higher rate of iCVS in the surgery group. One of the possible explanations is that surgical manipulation of the larger arterial vessels may lead to vasospasm of the microvasculature [9]. These results are analogous to the data showing that coiling is associated with a lower rate of vasospasm and delayed cerebral ischemia [3]. Moreover, patients who had iCVS also had a higher risk of suffering from delayed cerebral ischemia, suggesting that iCVS reflects vulnerable vasculature that is also prone to delayed vasospasm. Hypothetically, manipulation of vessels may lead to decreased vasoreactivity and, therefore, favor ischemia later on [2]. The causes of iCVS remain controversial, but surgically induced iCVS has to be considered as an important factor. This preliminary series suggests an association between iCVS and CVS or DND. Further studies are warranted to investigate the pathogenesis of iCVS, namely acute CVS, and its influence on the outcome after acute treatment of SAH.
Conclusion
APV exists and is a common finding in patients with SAH. Further studies are warranted to correlate the presence of APV with postoperative ischemia, dCVS, and outcome.
Conflict of Interest Statement
We declare that we have no conflict of interest.






