Angioplasty and Stenting of Atherosclerotic Disease
Key Points
Carotid endarterectomy is the established treatment of choice for symptomatic carotid artery bifurcation disease in most patients.
Intracranial angioplasty/stenting with bare or drug-eluting stents has a role to offer in some patients, although the hazardous nature of the procedure warrants extreme caution.
Carotid Artery Angioplasty and Stenting
Carotid artery atheromatous disease accounts for approximately 10% to 20% of ischemic stroke (1,2). Several randomized controlled trials have established that carotid endarterectomy is the standard of care for symptomatic carotid artery disease of moderate or severe degree, compared with best medical management (3,4,5). Timely endarterectomy of severe (>70%) stenosis within 2 weeks of onset of symptoms brings about an absolute risk reduction of 15.6% and a relative risk reduction of 52% over medical therapy. For symptomatic carotid artery stenosis >50% in degree, the benefit of endarterectomy is a reduction in the absolute risk of stroke of approximately 8% per year. The relative risk reduction of approximately 52% compared with medical management sounds substantial, but this is a reduction of an uncommon event, and thus the absolute benefit to an asymptomatic patient in whom this event is even less common than among symptomatic patients is even more marginal (6,7). In fact at the time of these studies, endarterectomy could only be rationally recommended for the symptomatic and asymptomatic populations if perioperative (30 day) death and stroke risks could be confined below 6% and 3%, respectively. Moreover, it is worth realizing that the margin of benefit to patients from endarterectomy has probably narrowed significantly since the 1990s because of substantial improvements in the medical and pharmaceutical options which have become mainstream since that time. This would imply that the stringent performance standards for endarterectomy complications, <6% complication rates for symptomatic, <3% for asymptomatic patients, have been shaved down substantially since the time when these landmark studies were completed.
Since it was first approved under stringent conditions by the U.S. Food and Drug Administration in 2004 for patients at high risk for endarterectomy, carotid artery angioplasty and stenting has grown substantially in use as an alternative definitive revascularization procedure for carotid occlusive disease. The reasons for this change are unclear, but likely manifold. The novelty of the procedure, the wider pool of participating physicians interested in the procedure, the general conventional wisdom that minimally invasive procedures are better and less costly than surgical procedures especially for older patients, the perception that avoidance of general anesthesia must be a good thing especially for older patients, and the presumption that the improved technology surrounding carotid stenting must translate into safer outcomes are likely all part of the explanation for the change in this standard of practice. None of these factors or assertions has been shown to be valid in the case of carotid stenting, but this trend away from endarterectomy shows every sign of gaining even more momentum in the foreseeable future.
There is no evidence that carotid artery stenting for symptomatic or asymptomatic carotid disease represents an improvement in patient welfare over carotid endarterectomy, and most evidence suggests that stenting is less safe under typical clinical circumstances (1,8,9). It seems reasonable to ask if there might be a place for this procedure in particular situations of risk, for example, radiation injury where surgical dissection and tissue healing are problematic, previous endarterectomy where surgical dissection is hampered by scar tissue, or unusual situations where a contralateral lower cranial nerve injury already exists and the addition of a new nerve injury would represent a significant injury to the patient. However, these situations represent a minority of patients with moderate or severe carotid disease.
Several randomized trials have been performed comparing endarterectomy and carotid stenting (with or without angioplasty) (10,11,12,13,14,15,16,17). All, or virtually all, of these studies of endarterectomy versus stenting have come up with the same answer, which is that under the strict conditions of a rigorously monitored trial with experienced surgeons and thoroughly screened interventionalists, carotid artery stenting is not as safe as endarterectomy (1). Overall stroke
and death rates within 120 days of carotid artery stenting are in the range of 8.9%, whereas endarterectomy patients show a rate of 5.8% based on data from several studies (18). While results for patients under 70 years are more equivalent between the two procedures, these pooled numbers reflect the extreme discrepancy of adverse events in the age group >70 years, 12% complication rates following stenting versus 5.9% following endarterectomy. One major trial was discontinued by its safety committee (15) due to the unacceptably high 30-day incidence of death or any stroke during the progress of the trial, 3.9% following endarterectomy, and 9.6% following carotid stenting. The major trial in the United States, CREST (16,19), evaluated clinical outcome on the basis of an aggregate of the incidence of stroke, death, and myocardial infarction, and found no significant difference between the stenting and endarterectomy groups. However, myocardial infarction was defined as any rise in the postprocedure enzyme assay, which skewed the aggregate score in favor of stenting. Setting cardiac enzymes aside, the risk of stroke or death in the CREST study was significantly higher in the stenting group 6.4% versus 4.7% for the endarterectomy group, while myocardial infarction or enzyme elevations were more common in the surgical group.
and death rates within 120 days of carotid artery stenting are in the range of 8.9%, whereas endarterectomy patients show a rate of 5.8% based on data from several studies (18). While results for patients under 70 years are more equivalent between the two procedures, these pooled numbers reflect the extreme discrepancy of adverse events in the age group >70 years, 12% complication rates following stenting versus 5.9% following endarterectomy. One major trial was discontinued by its safety committee (15) due to the unacceptably high 30-day incidence of death or any stroke during the progress of the trial, 3.9% following endarterectomy, and 9.6% following carotid stenting. The major trial in the United States, CREST (16,19), evaluated clinical outcome on the basis of an aggregate of the incidence of stroke, death, and myocardial infarction, and found no significant difference between the stenting and endarterectomy groups. However, myocardial infarction was defined as any rise in the postprocedure enzyme assay, which skewed the aggregate score in favor of stenting. Setting cardiac enzymes aside, the risk of stroke or death in the CREST study was significantly higher in the stenting group 6.4% versus 4.7% for the endarterectomy group, while myocardial infarction or enzyme elevations were more common in the surgical group.
The conclusion taken from these trials and editorial critiques often seems to be that “carotid stenting is almost as good as carotid endarterectomy and with the correct protective devices and rigorous screening of interventionalists, carotid stenting might come out on top eventually,” or so one might conclude from the observation that ordering still more trials seems to be the outcome whenever carotid stenting fails to outrun endarterectomy. Even at that, however, trial conditions are currently still biased in favor of carotid stenting. The clinical events examined in the trials to date, death and stroke, have dominated attention in this field. Relatively little attention has been paid to more subtle or comprehensive neurocognitive markers of brain performance following one procedure or the other. One randomized study of symptomatic patients (11) with results along the lines of those already discussed found significantly higher clinical rates of stroke within 30 days following stenting (7.4%) versus endarterectomy (4%). However, they also found that DWI brain injuries 1-day posttreatment were seen in 50% of stent patients and only 17% of endarterectomy patients. At 1-month posttreatment FLAIR injuries were present in 33% of stent patients and 8% of endarterectomy patients (20). Within this study, these numbers were even worse (73% of stent patients had DWI findings postprocedure) at centers where cerebral protection devices had been used during the stenting procedures. Several other authors have made similar observations in the comparison of stenting and carotid endarterectomy to the effect that clinically silent DWI injuries are much more common following stenting procedures, 34% to 71% of stent patients, compared with <10% of endarterectomy patients (21,22,23,24,25,26,27,28,29). Furthermore, the extent and number of lesions are greater in the stenting group, with substantial numbers of lesions showing up in alternative arterial distributions following stenting, in contrast to endarterectomy where the lesions are more typically confined to the artery undergoing surgery. The presumed explanation for this observation is the risk posed to the patient by aortic arch disease and navigation of devices across the ostia of major vessels.
So far, the different question of whether carotid stenting is more effective or safer than best medical management, akin to the question asked about endarterectomy in the original ACAS and NASCET studies, has not been addressed.
There are two separate and distinct worlds. There is the domain of rigorously controlled trials in which some attempt at standardization of the patients and the level of training of operating physicians is made, and from this world the data cited above are generated. The real world of medical practice is not the same. When carotid endarterectomy was first demonstrated to be effective, the major paper of the NASCET trial concluded: “Our final results do not justify a large increase in the rate of endarterectomy. We recommend restraint” (3). Such restraint was not forthcoming in the years that followed, and substantial correction to the excessively liberal practice of endarterectomy among Medicare patients, particularly in some geographic areas, eventually proved necessary, reducing the rate of inappropriate surgery from 32% to 8% (30). Based on less convincing evidence than that shown in the NASCET trial, the same phenomenon is likely to take place with carotid stenting in the years to come. Already 30-day mortality rates among Medicare patients undergoing carotid stenting (1.9%) exceed mortality rates in the CREST trial (0.7%) (8). More than 80% of Medicare patients undergoing carotid stenting are >70 years in age, the very group least suited for this procedure in the randomized trials referenced above (31), and nearly one-third of them are >80 years, a group very prone to complications following stenting in controlled trials.
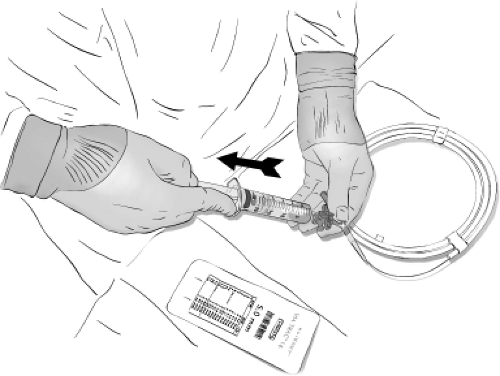
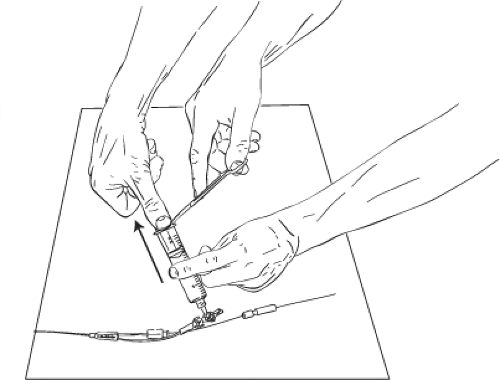
From the point of view of the physician who simply wishes to do a good job for his/her individual patients, there is little to guide one in technical or procedural recommendations (Figs. 31-1–31-9). Some authors are adamantly in
favor of using cerebral protection in the form of balloons or filters and their argument seems cogent (32). It seems to make sense that a 100 μm filtering mesh or complete arrest of flow above the stent site must lend some protection to the brain. Others have analyzed their data and concluded that protection devices have no impact on outcome and could represent a risk of complications independently of other factors (33). Their argument is that crossing an atherosclerotic plaque of dubious integrity with a complex device, deploying that device in the carotid artery, retrieving that device through the stent afterward, or in the case of balloon arrest of flow, advancing a 9F catheter in the aorta and common carotid artery have all got to be hazardous to the welfare of the patient. Use of a filter certainly adds to the complexity of a carotid stent case and may be associated with more showering of hits on transcranial Doppler and DWI changes than unprotected procedures (34,35,36). Even the safest design of stent is not clear. A closed-cell design is advocated by those who believe in the theoretical capacity of the metal struts to pinion down (“scaffolding”) potentially itinerant plaque during vessel expansion or postdilation (32). However, closed-cell design stents have other features such as diminished flexibility and pliability compared with open-cell design, which might be theoretically disadvantageous from the point of view of vessel compliance and distortion of native anatomy, particularly in a tortuous vessel. Comparison of closed- and open-cell design stents on the basis of clinical complications shows no major differences between the two designs in immediate complications or MRI findings (37). Hemodynamic and rheologic differences between closed- and open-cell design stents are measurable, however, in that peak systolic velocities in the carotid artery are more than twice as likely to be in the elevated range following closed-cell design stent placement compared with open-cell design (38). Whether this differential impact of stent designs on vessel compliance and on the hemodynamics of flow has a significant outcome on long-term cerebrovascular health is not known.
favor of using cerebral protection in the form of balloons or filters and their argument seems cogent (32). It seems to make sense that a 100 μm filtering mesh or complete arrest of flow above the stent site must lend some protection to the brain. Others have analyzed their data and concluded that protection devices have no impact on outcome and could represent a risk of complications independently of other factors (33). Their argument is that crossing an atherosclerotic plaque of dubious integrity with a complex device, deploying that device in the carotid artery, retrieving that device through the stent afterward, or in the case of balloon arrest of flow, advancing a 9F catheter in the aorta and common carotid artery have all got to be hazardous to the welfare of the patient. Use of a filter certainly adds to the complexity of a carotid stent case and may be associated with more showering of hits on transcranial Doppler and DWI changes than unprotected procedures (34,35,36). Even the safest design of stent is not clear. A closed-cell design is advocated by those who believe in the theoretical capacity of the metal struts to pinion down (“scaffolding”) potentially itinerant plaque during vessel expansion or postdilation (32). However, closed-cell design stents have other features such as diminished flexibility and pliability compared with open-cell design, which might be theoretically disadvantageous from the point of view of vessel compliance and distortion of native anatomy, particularly in a tortuous vessel. Comparison of closed- and open-cell design stents on the basis of clinical complications shows no major differences between the two designs in immediate complications or MRI findings (37). Hemodynamic and rheologic differences between closed- and open-cell design stents are measurable, however, in that peak systolic velocities in the carotid artery are more than twice as likely to be in the elevated range following closed-cell design stent placement compared with open-cell design (38). Whether this differential impact of stent designs on vessel compliance and on the hemodynamics of flow has a significant outcome on long-term cerebrovascular health is not known.
Extracranial Vertebral Artery Angioplasty and Stenting
Symptomatic extracranial vertebral artery atherosclerotic occlusive disease is a condition with a poor natural history (39). While it has not received the detailed scientific scrutiny accorded to “typical” carotid artery disease in the form of randomized controlled trials, some differences between carotid and vertebral artery disease are evident and are relevant to the clinical decision-making process of whether to attempt endovascular repair in a symptomatic patient.
Symptomatic posterior circulation atherosclerotic disease has an incidence of stroke or death within 1 year of approximately 5% to 11%, and transient ischemic attacks related
to extracranial vertebral artery disease portend a stroke rate of approximately 30% over 5 years (40,41,42,43). The neurologically debilitating nature of even small strokes in the posterior circulation compared with the carotid circulation is not reflected in these numbers, but adds to the urgency of efforts to help patients with these conditions (39).
to extracranial vertebral artery disease portend a stroke rate of approximately 30% over 5 years (40,41,42,43). The neurologically debilitating nature of even small strokes in the posterior circulation compared with the carotid circulation is not reflected in these numbers, but adds to the urgency of efforts to help patients with these conditions (39).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree