14 | Ankylosing Spondylitis: Cervicothoracic Osteotomy |
 | Case Presentation |
History and Physical Examination
A 57-year-old man has been followed by several specialists for ankylosing spondylosis (AS). In recent years, he has noted his posture to decline gradually to the degree where it has been affecting his work as an accountant. He has difficulty with grooming, ambulating, and socializing with his coworkers due to his worsening posture. His neurological exam was normal.
Radiological Findings
His most recent x-ray is shown in Fig. 14–1A. Radiographs show cervicothoracic kyphosis and bridging syndesmophytes, typical of AS. His chin-brow angle was 60 degrees with his horizontal gaze unable to compensate for his cervicothoracic kyphosis.
Diagnosis
Diagnosis of decompensated cervicothoracic kyphosis due to AS was made. He eventually agreed to posterior cervicothoracic osteotomy with internal fixation as well as halo immobilization (Fig. 14–1B).
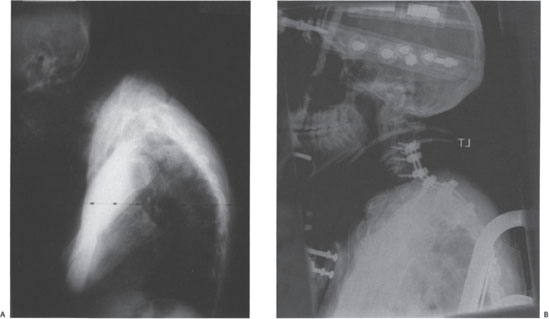
Figure 14–1 (A) Preoperative and (B) postoperative radiographs of a patient with ankylosing spondylitis and cervicothoracic kyphosis.
 | Background |
AS typically affects young adults, most commonly males (M:F = 3:1) in their second through fourth decades. Women tend to have less severe involvement.1 The juvenile-onset ankylosing spondylitis (JAS), with the onset of symptoms earlier than 16 years, has a higher incidence of hip disease. Patients with hip joint involvement show a faster progression of the spinal disease. In absence of hip disease, there is little difference between juvenile-onset and adult-onset AS in severity of spinal and extraskeletal manifestations.2
Peripheral arthritis in AS is seen in 20 to 40% of patients and is oligoarticular, asymmetric, and often affects hips or shoulders. The other less frequently involved joints are the temporomandibular joint, knees, ankles, elbows, and wrists. Involvement of hip joint is far more disabling than spinal rigidity.3 Painful peripheral enthesitis often involves heel insertion of the Achilles tendon and plantar fascia, and less frequently may involve the superior and inferior poles of the patella, the tibial tubercle, pubic attachment of the adductor longus, and the femoral trochanters, humeral epicondyles, and nuchal crests. The extraskeletal manifestations may include iritis, aortic incompetence and conduction defects, and diminished chest expansion (typically < 2.5 cm).
 | Deformity |
As the disease progresses, the spine is gradually ankylosed with a generalized kyphotic deformity. To maintain upright posture the patients hyperextend their hips and flex their knees. Involvement of the hip joints seriously compromises the compensatory postures. At the initial stages of deformity hyperextension of the cervical spine helps in maintaining the forward gaze. In advanced cases, when the cervical spine becomes ankylosed in flexion, the spinal deformity is best described as a global ankylosis and kyphosis. Severe kyphosis of the cervical spine may lead to difficulty in jaw opening. Global kyphosis and ankylosis lead to two distinct problems: loss of sagittal balance [forward shift of the sagittal vertical axis (SVA)] and loss of forward gaze. Clinically these two functional deformities are evaluated as chin-brow angle, gaze angle, and occiput-to-wall distance (Fig. 14–2). Most patients are neurologically normal, with preservation of deep tendon reflexes. A slow, progressive cauda equina syndrome may appear late in the course of the disease.
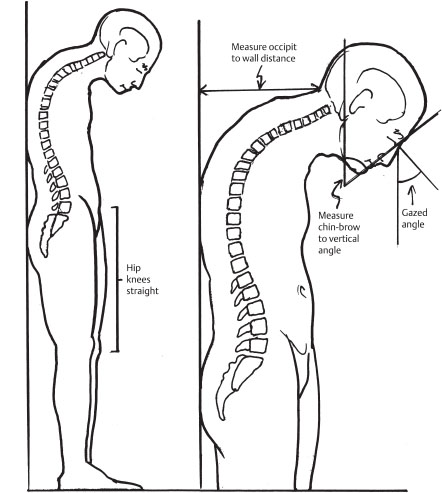
Figure 14–2 A proper assessment of deformity requires standing with hips and knees straight to unmask any compensation. Radiographs should also be obtained in this position. A preoperative chin-brow to vertical angle and occiput-wall distance should be measured, as shown here.
 | Radiological Features |
Radiographic changes are minimal in the early stages. Technetium 99m bone scan may demonstrate the sacroilitis before radiographic changes.4 Symmetric bilateral patchy areas of osteoporosis along the ill-defined sacroiliac joint are often suggestive of early disease. Later, subchondral erosions followed by patchy areas of ossifications develop that eventually leads to obliteration of the sacroiliac joint.
An early radiological feature is squaring of the anterior corners of the thoracic and lumbar vertebrae due to osteopenia at the attachment of the anterior annulus. Vertebral osteopenia also accompanies the loss of normal concavity of the end plates.5 Ossification extends within the substance of the annulus forming syndesmophytes, which bridge the adjacent vertebral bodies and develop into the bamboo spine in late stages.6 Posterior vertebral structures are also ossified. These include the capsule of the facet joints, supraspinous and interspinous ligaments, and ligamentum flavum.
In subaxial cervical spine extensive ankylosis with varying degree of kyphosis is seen in the advanced stages. In contrast, the upper cervical spine may demonstrate hyper-mobility due to atlantoaxial instability.7
 | Assessment of Deformity |
Flexion contracture of the hips, loss of lumbar lordosis, and progressive thoracic and cervical kyphosis all may contribute to the functionally disabling stooped posture of patients with AS. Determining the site of deformity is critical before surgically treating the deformity. Deformity must be assessed both clinically and radiographically as part of preoperative planning. The level of deformity will aid in determining the benefit of total hip arthroplasty (THA) and the level of corrective spine osteotomy and degree of correction necessary.
The chin–brow angle is the angle between the line drawn from the chin to the brow and a vertical line (Fig. 14–2). Occiput-to-wall distance is measured to grossly determine the patient’s sagittal balance. The horizontal distance from the occiput to the wall is measured with the patient’s buttocks and heels against the wall. Clinically, occiput-to-wall distance should be 0 to 2 cm, with hips and knees extended. The degree of hip flexion contracture is determined by placing the patient supine with the lumbar spine pressed flat to the examining table, then measuring the angle that each femur makes with the horizontal.
Normal sagittal balance places the center of mass just in front of the S1 vertebral body. Therefore, radiographically, a plumb line drawn from the center of the C7 vertebral body should just touch the anterior edge of the body of S1 on the lateral radiograph. With global kyphotic deformity of the spine, the plumb line shifts forward, and the horizontal distance of the plumb line from the anterior edge of the S1 vertebral body is a measure of the loss of sagittal balance that requires correction. There is a natural tendency for the sagittal imbalance to be compensated by flexion of the knee and hyperextension of the hips, if these joints are still mobile. It is therefore important to obtain the standing lateral radiograph of the whole spine, with the hips and knees straight, to unmask the true horizontal shift of the plumb line. Because of the deformity, it is often necessary to use two separate x-ray cassettes for taking radiographs of the entire spine.
 | Authors’ Preferred Method of Surgical Management |
Indications for Deformity Correction
Surgical intervention is indicated when kyphosis is decompensated. That means the patient cannot maintain a horizontal gaze when the hips and knees are extended and eyeballs are in the neutral position.8 In practice, however, the general condition of the patient, the feasibility of correction, and, perhaps above all else, the morale and earnest desire of the patient to accept the risks and rehabilitative measures required for correction become more important decisive factors before considering surgery.
Osteotomy of the cervical spine should be limited to patients with rigid deformities. Evidence of recent fracture, characterized by an overt fracture or by new onset of pain in the cervical spine of a person previously without pain, is a contraindication to osteotomy.
Preoperative Planning
Surgical correction of sagittal plane deformity requires careful planning of site, type, and number of osteotomies. The methods of correction of kyphotic deformity may include a large monosegmental lumbar osteotomy, smaller multisegmental thoracic osteotomies, cervical osteotomy, or a combination of these. The goals are (1) restoration of sagittal balance (horizontal posterior shift of the C7 plumb line) (2) correction of gaze angle, and (3) safety of the procedure.
As mentioned earlier, proper estimation of gaze angle and sagittal balance correction will require a full-length standing lateral radiograph of the spine when the patient stands with relaxed hips, without making an effort to correct the spinal balance or forward gaze. The degree of gaze angle correction needed is determined by the chin-brow to vertical angle.9 The sagittal balance correction is estimated from the degree of posterior shift of the plumb line required to bring it back to the sacrum.
A kyphotic deformity located predominantly in the lumbar spine results in loss of sagittal balance, and surgical correction often requires a lumbar osteotomy. Conversely, a predominant flexion deformity in the cervicothoracic region may lead to characteristic “chin on chest” posture, which causes severe restriction of the forward gaze and interferes with jaw opening but does not produce significant problems with the sagittal balance. The corrective osteotomy therefore should be planned at the cervicothoracic junction.
Sagittal balance is restored by redirecting the spine posteriorly at the level of the osteotomy so that the head lies vertically above the pelvis. The angle by which the spine is redirected at the osteotomy site is called the osteotomy angle. The level of osteotomy to correct a global kyphotic deformity has a disparate effect on gaze angle and sagittal balance (Fig. 14–3). The lower the level of osteotomy performed (e.g., in the lower lumbar spine), the greater is the horizontal shift of the plumb line for the same osteotomy angle. In other words, if the osteotomy has to be performed at a higher level (e.g., thoracic spine), a much larger osteotomy angle would be required for the same degree of horizontal shift of the plumb line.10,11 In contrast, the visual angle (by which the gaze is redirected forward) will always be the same as the osteotomy angle, irrespective of the level of the osteotomy.
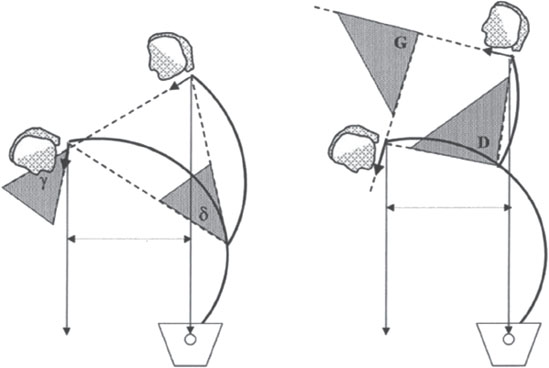
Figure 14–3 Effect that level of osteotomy has on sagittal balance and gaze angle. Restoration of sagittal balance is achieved by posterior shift of the plumb line (X). The correction of the gaze angle (γ and G) is always the same as the corresponding osteotomy angle (δ and D), respectively, δ = γ and D = G. (A) When osteotomy is performed at a lower level (M), an osteotomy angle d is needed for restoration of the sagittal balance (X). (B) When osteotomy is performed at a higher level (N), a larger osteotomy angle (D) is needed (D > δ) for the same degree of sagittal balance restoration (X). Because osteotomy angle is always the same as the gaze angle correction (D = G), the correction of the gaze angle will be larger (G > γ) with a higher level of osteotomy. This may lead to overcorrection of the gaze angle upward.
(From Lippincott Williams and Wilkins, from Sengupta DK, Khazim R, Grevitt MP, Web JK. Flexion osteotomy of the cervical spine: a new technique for correction of iatrogenic extension deformity in ankylosing spondylitis. Spine 2001;26:1068-1072. Reprinted with permission.)



