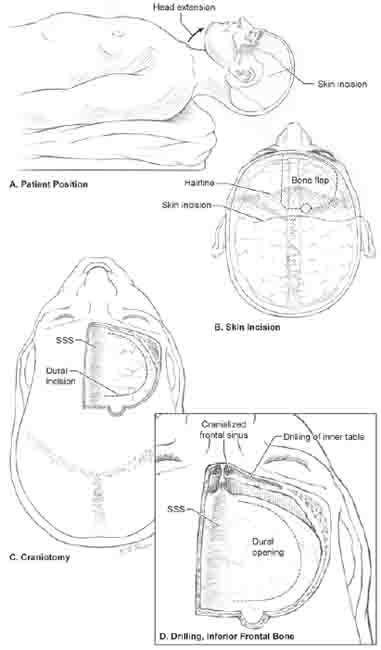
12 Anterior Interhemispheric Approach Pericallosal artery (PcaA) aneurysms originate from a right-or left-sided bifurcation of the anterior cerebral artery (ACA), but are midline aneurysms deep to the falx. Therefore, the anterior interhemispheric fissure needs to be accessed only on one side, and the craniotomy is eccentric to that side. The right side is chosen for these aneurysms to avoid complications in the dominant hemisphere resulting from the craniotomy, venous sacrifice, or retraction. The patient is positioned supine with the head in neutral position (nose up) and the neck extended slightly (Fig. 12.1A). A bicoronal skin incision is needed to mobilize the scalp flap inferiorly enough for a craniotomy cut that runs across the anterior cranial fossa floor (Fig. 12.1B). The incision begins at the right zygoma and ends at the contralateral superior temporal line because the craniotomy is eccentric to the right side. The scalp is folded to expose supraorbital frontal bone from the ipsilateral superior temporal line to the contralateral glabella. Pericranium is harvested during the opening to make it available during the closure to cover the frontal sinus, if it has been entered. It is easier to harvest pericranium as a separate layer as the scalp flap is elevated, rather than to peel it away from a folded scalp flap at the end of the procedure. Pericallosal artery aneurysms are exposed optimally with a craniotomy flap whose medial border crosses the superior sagittal sinus (SSS) to the contralateral (left) side (Fig. 12.1C). Midline exposure enables the dura to be opened to the edge of the SSS and directly accesses the interhemispheric fissure without any overhanging bone. The craniotomy flap is extended inferiorly as close to the anterior cranial fossa floor as possible. Crossing the midline with this cut sometimes requires drilling down the ridge of bone on the inner table in the midline. The lateral cut extends to the superior temporal line, and the temporalis muscle is left undisturbed. The posterior cut extends to the coronal suture. The SSS is crossed carefully with the craniotome. Its epidural location is established visually before crossing the sinus by aiming light into the cut of bone and irrigating enough to see intact dura. If a dural tear is detected, the flap is taken in two pieces. The craniotomy flap can be raised safely as one flap in younger patients with dura that is not adherent to the inner table of the skull, and in many women with a shallow bony sulcus of the SSS. However, this craniotomy flap is raised in two pieces in elderly patients or those with thin, adherent dura. The first piece is a unilateral (right) frontal flap taken up to, but not across the SSS. After removing this bone flap first, dura containing the SSS is dissected from the inner table of the skull under direct visualization to minimize the risks of sinus injury or excessive bleeding from the emissary veins. The second portion of the craniotomy safely crosses the SSS twice, with the dura retracted away from the skull. The inner table of the frontal bone in the inferior midline is drilled until flat (Fig. 12.1D), in a manner analogous to drilling the sphenoid bone for a pterional approach. This additional bone removal increases visualization along the anterior cranial fossa floor for accessing proximal control of low-lying PcaA aneurysms. This bone removal may also enter and cranialize the frontal sinus, which requires coverage with a pericranial graft during the closure. Dura is opened with a semicircular flap based against the SSS. Bridging frontal veins are preserved when they are large and more posteriorly located. A vein that fuses with the dura before reaching the SSS can be saved by dividing the dural flap on both sides of the vein and elevating two flaps instead of one. These cuts fashion a sleeve of dura over the vein that preserves the vein. Venous infarction is a potentially devastating complication that is difficult to predict, which means that bridging veins should be preserved whenever possible. Pericallosal artery aneurysms that lie along the A4 or A5 segments are rare, but their distal location on the body of the corpus callosum allows for a modified anterior inter-hemispheric approach that uses gravity to retract the right hemisphere. The patient is positioned supine with bolsters under the left shoulder. The head is turned 90 degrees to the right with the sagittal midline parallel to the floor, and angled 45 degrees upward (lateral neck flexion) (Fig. 12.2A,B). This position allows gravity to retract the dependent right hemisphere and open the interhemispheric fissure.
 Position, Incision, and Extracranial Dissection
Position, Incision, and Extracranial Dissection
 Craniotomy
Craniotomy
 Dural Opening
Dural Opening
 Gravity Retraction
Gravity Retraction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




