Chapter 41 Anterior Lumbar Stabilization
INTRODUCTION
In the anterior reconstruction of the lumbar spine, there are several anatomical and biomechanical features unique to the lumbar spine.1 The important points are the large size and high weight-bearing demand of the lumbar vertebral bodies; greater mobility than the thoracic spine; lordotic curvature; restricted access to the lower lumbar spine because of the pelvic ring; and functional importance of the lumbar nerve roots compared with those of the thoracic spine. Although the upper lumbar segment (L1, L2 level) is considered to be the transitional zone between the rigid thoracic spine and the mobile lumbar spine, thoracolumbar instability is not a common problem after anterior-only reconstruction or circumferential decompression and stabilization at these levels. For L5 lesions, it is impossible to apply anterior stabilization because of the pelvic ring, which may be the case even in L4 lesions. In these cases, the stabilization should be performed with the posterior approach. The commonly used fixation site is the lateral surface of the vertebral body in the lumbar spine because of the midline location of the great vessels.
TECHNIQUE
PSOAS MUSCLE DISSECTION
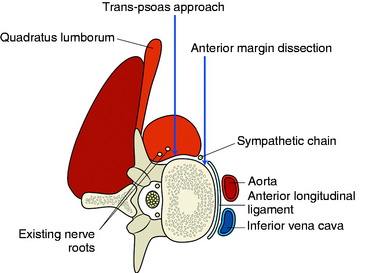
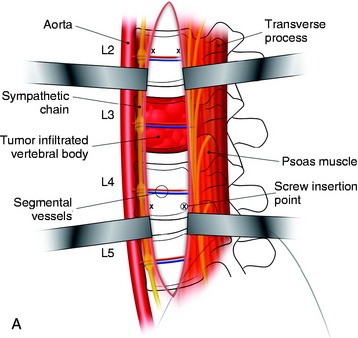
The stabilization procedure is carried out after retroperitoneal exposure of the lateral surface of the vertebral bodies. When the anterior instrument is implanted on the lateral surface of the lumbar vertebral body, the psoas muscle should be dissected. The psoas muscle covers the lateral surface of the vertebral body from the base of the transverse process to the lateral margin of the anterior longitudinal ligament (Fig. 41-1). The anatomical safe zone is the middle one-third of the width of the psoas muscle belly. In the anterior margin, the sympathetic chain lies underneath the psoas muscle and the exiting nerve roots are around the foramen. There are two ways to dissect the psoas muscle from the bony surface. First, the dissection starts from the anterior margin of the psoas muscle and continues to the foraminal side (see Fig. 41-1). Second, the dissection starts from the midline of the psoas muscle belly and retracted mediolateral side. During dissection of the psoas muscle, it is important not to injure the underlying extraforaminal nerve roots.
Course of Lumbar Nerve Root on Lateral Surface of the Lumbar Vertebral Body
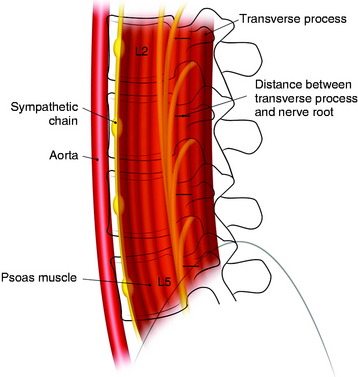
Each lumbar nerve root exits through the superior portion of the corresponding intervertebral foramen. At the beginning of the extraforaminal region, the exiting root runs down the lateral surface of the caudal pedicle, where it traverses the vertical leaf of the intertransverse ligament to take a ventrolateral direction and then join the descending lumbar trunk within the fascia of the posteromedial portion of the psoas muscle. The lumbar trunk runs downward vertically, as a compact cord-like bundle along the surface of the junctional area between the body and the pedicle of the lumbar spine, outside the foramen. The compact cord-like trunk is close to the most dorsolateral surface of the vertebral body and the intervertebral disc space. The width of the nerve trunk gradually increases in the lower lumbar level. The lumbar nerve trunk is topographically arranged dorsoventrally with the L5, L4, L3, and L2 nerve roots, in that order (Fig. 41-2).
The mean distances from the anterior border of the transverse process to the upper segment of the lumbar nerve root are estimated to be 5.1 to 6.4 mm (range 3–8 mm) at L2–5.2 There is little variation between the upper and lower levels. When surgeons dissect the psoas muscle, the expected location of the nerve roots is near the foramen.
Anterior Margin Dissection Method
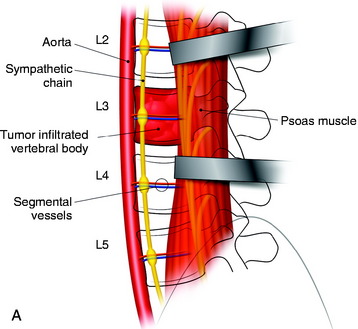
The spine is exposed, following the anteromedial slope of the psoas muscle. The genitofemoral nerve, which passes along the psoas muscle, must be preserved. The anterolateral attachments of the psoas muscle are sharply dissected from the vertebral body. Care is used not to injure the underlying sympathetic chain and the segmental vessels. As in the vertebral bodies of other levels, the segmental vessels are arranged on the mid-portion of the vertebral body. On the axial view, the anterior margin of the psoas muscle corresponds to the anterior one-third of the vertebral body (see Fig. 41-1). When the medial half of the psoas muscle is swept away from the vertebral body, the posterior cortex of the vertebral body is visible (Fig. 41-3). For complete decompression, the pedicle should be palpated and the foramen should be recognized. The extraforaminal nerve roots are enclosed in the fascia of the muscle, so the possibility of nerve injury is small. However, because of the bulkiness of the psoas muscle, sufficient exposure of the lateral body surface may sometimes be difficult.
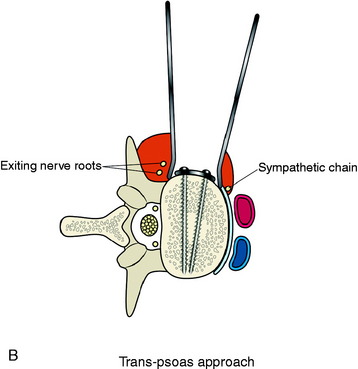
Trans-Psoas Dissection Method
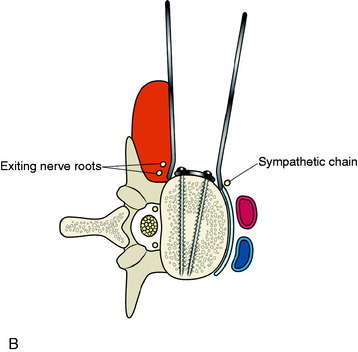
When the psoas muscle is split longitudinally on the mid-portion of the muscle belly, the line of access corresponds to the posterior two-thirds of the vertebral body (Fig. 41-4). This approach route has a greater possibility of injuring the exiting nerve roots.
If the psoas is accessed correctly, the muscle fiber is dissected in the longitudinal plane.3 The dissection approaches to the vertebral body surface, and the muscle fascia is peeled off from the body surface. Once dissection through the psoas muscle is complete, the corpectomy is started.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree