♦ Preoperative
Operative Planning
- Location (cervical, thoracic, lumbar) helps determine risks and morbidity of different approaches
- Biopsy proven pathology
- Staging of disease
- Life expectancy should exceed 3 months, unless to prevent paraplegia
- Cardiac and medical clearance
- What type of exposure will patient tolerate
- What level of disease defines surgical options
- What type of exposure will patient tolerate
- Type of decompression/resection
- Palliative
- Start within tumor to the margin of solid bone
- Decompress to dura
- Ventral stabilization
- Cement
- Bone rarely fuses in cancer cases.
- Titanium (not stainless) for vertebral body replacement if cage used
- Expandible cage
- Start within tumor to the margin of solid bone
- Oncological
- Spondylectomy or vertebrectomy
- Clean margins
- Complete removal: may be after posterior first stage procedure to remove the dorsal component of the vertebral segment
- Spondylectomy or vertebrectomy
- Palliative
- Embolization
- Necessary for renal cell, thyroid, myeloma/plasmacytoma
- May be beneficial for other lesions
- Necessary for renal cell, thyroid, myeloma/plasmacytoma
- Localization
- Preoperative placement of radiopaque localizing implant (such as Guglielmi detachable coils [Target Therapeutics, Fremont, CA] placed into costotransverse junction, metallic pin placed on transverse process [so it does not migrate])
- Make identification of level easier if there is no clear intraoperative localizer with intraoperative fluoro (such as isolated epidural disease in the mid-thoracic spine with no obvious local landmarks like a compression fracture, large unique osteophyte, etc.)
- Preoperative placement of radiopaque localizing implant (such as Guglielmi detachable coils [Target Therapeutics, Fremont, CA] placed into costotransverse junction, metallic pin placed on transverse process [so it does not migrate])
- Computed tomography scan (bone windows)
- Magnetic resonance imaging
- Spine x-rays
Operating Room Set-up
- Equipment
- Fluoro compatible table
- Fluoro unit
- Multiaxial reconstruction unit
- Fluoro compatible table
- General anesthetic issues
- If motor evoked potentials monitoring, then recommend total intravenous anesthesia or minimal inhalational
- Small (1 mg/hr) vecuronium if strong potentials
- Large bore catheters
- Central line
- Introducer, if possible
- Not groin line unless for a-line
- Central line
- Multiple units packed red blood cells in operating room before start
- Be prepared for massive transfusion, including factor and even factor 7 transfusion
- Although some advocate using cell saver with tumors using leukocyte filter, but the authors do not recommend this.
- Keep all metallic artifact-generating wires out of the fluoro field circum-ferentially
- If motor evoked potentials monitoring, then recommend total intravenous anesthesia or minimal inhalational
♦ Intraoperative
Cervical
- Anesthetic issues
- Single lumen tube, deflate and re-inflate endotracheal tube cuff once re tractors are in place
- Positioning
- Head toward anesthesia
- Traction may help provide stabilization and minimal decompression
- Head pins may be used, but risk is that the head will be fixed if the spine moves
- Head toward anesthesia
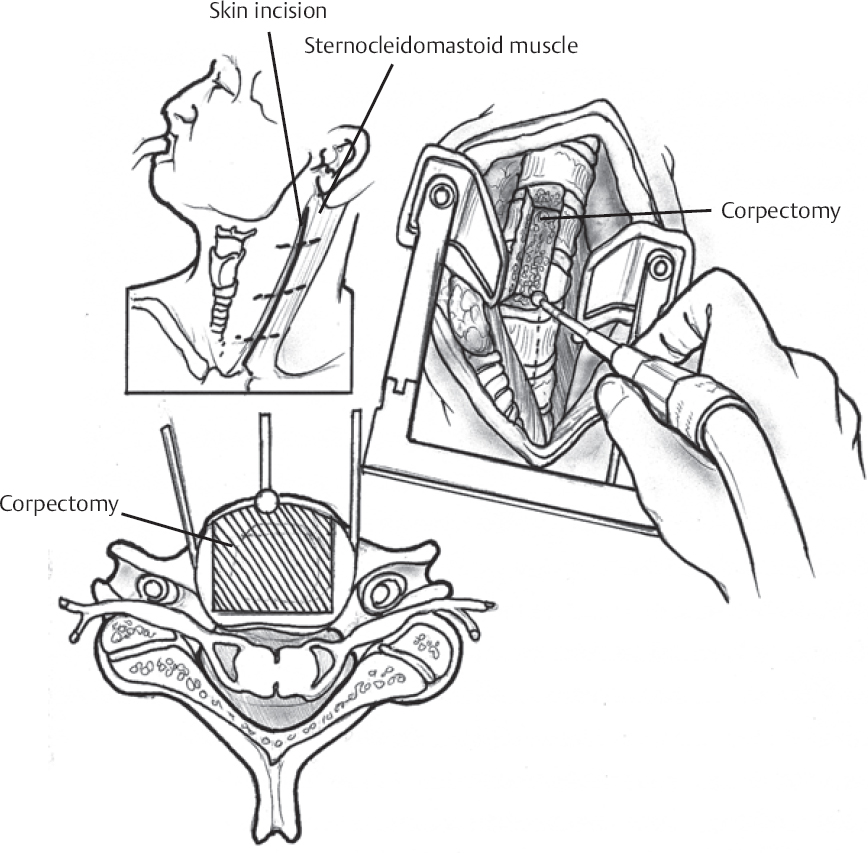
- Approach (Fig. 127.1)
- Ventromedial
- Tumors in body (vast majority of lesions)
- Ventrolateral
- Tumors involving vertebral canal/transverse process
- High retropharyngeal
- Tumors of C2 and C3
- Trans-oral
- Odontoid to clivus region lesions
- Ventromedial
- Stabilization
- Plate
- Cage
- Posterior supplemental stabilization
- Plate
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree