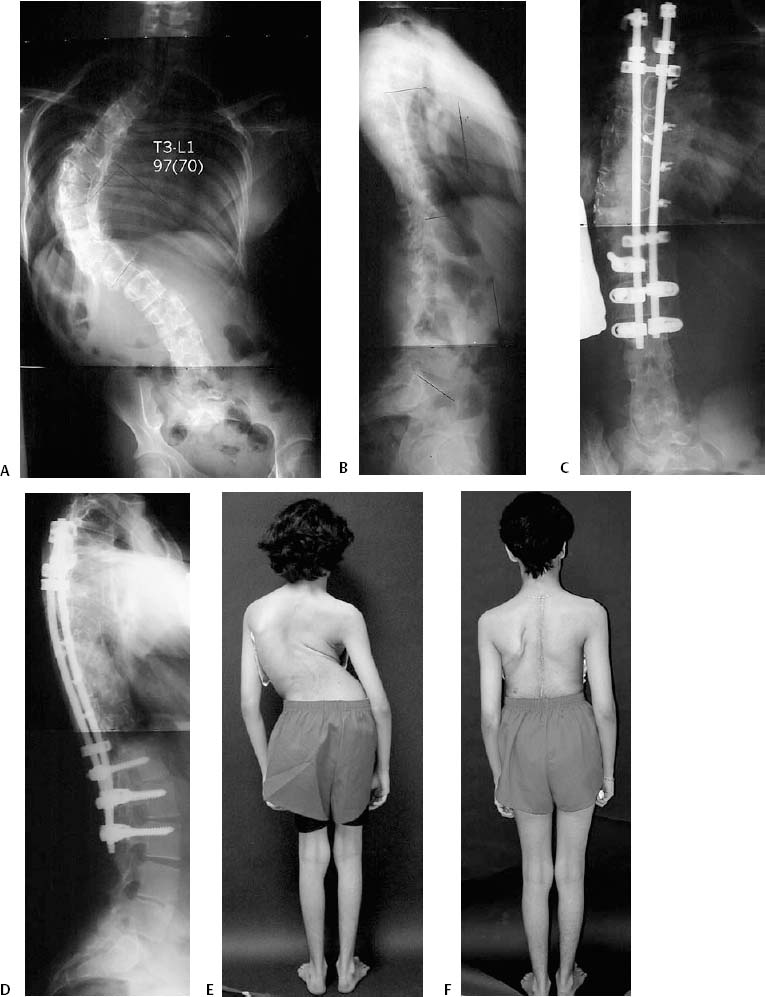
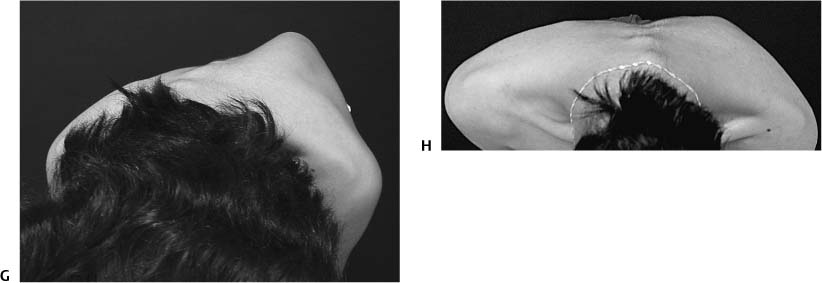
Chapter 17 A significant number of spinal deformities are successfully treated with a single anterior or posterior approach. However, in certain instances, both an anterior and posterior (AP) approach is indicated. Despite the increased morbidity1 of such AP procedures, improved deformity correction and enhanced arthrodesis has been reported.2–8 AP spine fusions may be performed on the same day in a sequential manner under a single anesthesia or under separate anesthesia several days apart, which we shall refer to as a staged procedure. Simultaneous approaches are performed under a single anesthesia at the same time. The simultaneous approach refers to both anterior and posterior procedures occurring at the same time under the same anesthesia. The simultaneous AP approach is not routinely recommended for deformity surgery because multiple vertebral segments may need to be treated, which is difficult given the patient position and resulting restricted access.9 With the developments in thoracoscopic techniques, the simultaneous approach may become more useful in the future. The primary indication for AP procedures is large rigid curves. Rigid curves are generally referred to as those with flexibilities less than 50% based on supine side-bending films or traction films. The approach to treatment in the pediatric patient differs from that of the adult patient. Pediatric patients inherently have improved fusion rates and more flexible curves in comparison with adults. In the pediatric patient with idiopathic scoliosis, successful curve correction may be achieved in patients with curves up to 85 degrees with a single approach.10–13 Although there are several techniques for providing this type of correction, the authors prefer the use of proximal and distal anchors and intervening sublaminar wires that translate the spine to a sagittal rod contoured to the expected sagittal contour of the patient. Proponents of multiple screw constructs suggest that use of screws over the apex of the curve can provide increased correction and improved rotation.10,13 This technique still requires additional validation in multiple centers. Pediatric patients with idiopathic curves greater that 85 degrees and rigid curves require AP procedures14 (Fig. 17–1). In the adult patient, the indication for surgery may include pain in thoracic curves greater than 50 to 60 degrees unrelieved by conservative management; significant deformity unacceptable to the patient; significant curve progression with or without sagittal or coronal imbalance; back pain, radicular or stenosis symptoms associated with lumbar deformity; significant loss in pulmonary function unrelated to parenchymal disease. In the adult patient, cures less than 70 degrees may be treated by surgery performed posteriorly only. Thoracoplasty and or concave rib osteotomies will assist in correction in these cases. Curves greater than 70 degrees with poor flexibility will generally require an AP procedure.15 Adults with thoracolumbar and lumbar curves should consider an anterior fusion for increased fusion rates in addition to poor flexibility. If the spine under consideration has poorly developed transverse processes or a laminectomy for stenosis will be required, the absence of sufficient posterior fusion surface may compromise the spine fusion, and an anterior fusion should be considered. The AP approach may be required in patients with instability, congenital scoliosis, pseudarthrosis, and postlaminectomy defects or to avoid crankshaft deformity in children. The indications for surgery are based on age, curve magnitude, extent of the curve, and etiology. The details in and variation in approaches for each individual etiology would be outside the scope of this chapter. Figure 17–1 Fourteen-year-old female with untreated scoliosis presented with large, aesthetically displeasing deformity. This patient underwent a sequential anterior release with internal thoracoplasty followed by posterior concave rib osteotomies and fusion with instrumentation and autologous bone graft. (A) Preoperative posterior/anterior (PA) standing radiograph demonstrates a rigid right thoracic curve, which measured 97 degrees from T3 to L1 and corrects to 70 degrees on bending. (B) Preoperative lateral radiograph with evidence of hypokyphosis and decreased lordosis with good global alignment. (C) Postoperative PA standing radiograph demonstrates balanced correction of the thoracic curve to 20 degrees. (D) Postoperative lateral radiograph demonstrates excellent sagittal contours. (E) Pre-operative clinical photograph demonstrates a large, left thoracic prominence with coronal malalignment. (F) Postoperative clinical photograph with excellent restoration of balance and reduction in the thoracic prominence. (G) Preoperative clinical photograph of the Adams forward bend test demonstrating a significant prominence. (H) Postoperative clinical photograph demonstrates excellent improvement in the thoracic prominence. Preoperative radiographic evaluation should in include full-length standing spine films in frontal and sagital planes, and 14 in. × 36 in. films are the routine at our institution. This full-length film allows complete assessment of all curves and the patient’s global balance. Bending films to assess the flexibility of the curve are crucial if surgery is being considered. Our preferred approach is with supine bending or traction films for larger curves.16,17 Other approaches including the fulcrum bending18,19 and push-pull films are not used routinely at our institution. Radiographic evaluation should not only include Cobb measurement of the curves but an evaluation of overall balance in the coronal and sagittal planes. MRI and CT-myelogram are common adjuncts particularly in the adult patient. An MRI alone is frequently insuffcient in providing all the necessary information particularly when assessing a large adult curve with stenosis. Diskography although still controversial may be helpful in the adult patient when evaluating the lowest disk to be included in the fusion or the disk that would become the junctional disk. Cardiac and pulmonary preoperative assessment should be part of the initial evaluation. Pulmonary function test should be considered particularly if thoracotomy, thoracoplasty, or concave rib osteotomies are planned. Lenke has described decreased pulmonary function of 27% in adults after thoracoplasty that may not return for up to 2 years.20 These issues need to be evaluated and considered preoperatively. In the pediatric patient, considerable decrease in pulmonary function, though a significant perioperative challenge, should not be considered a contraindication if an experienced team to manage patients in the perioperative period exists.21 Surgery performed on the same day is preferable to staged surgery performed days apart.4,22–24 However, there are technical and medical issues that may dictate a procedure be scheduled as a staged procedure or converted to staged from an intended same-day sequential AP procedure. Technically, the amount of surgery required may be far too great for the allotted surgical time and difficult for the surgical team to complete. If a late start is achieved either due to difficulty with required intubation and line insertion or the surgical approach to the spine is difficult, the procedure may need to be staged. After the anterior procedure, it is customary to consult with the anesthesia team to ascertain whether the patient is stable enough to undergo a second operative procedure. Unforeseen medical events during the first procedure such as significant loss in blood, issues regarding blood pressure, or cardiac events may require conversion to a staged procedure.
Anterior/Posterior (AP) Surgery for Spinal Deformity
♦ Indications for AP Surgery
♦ Preoperative Care
♦ Staging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree