Anxiety disorders – management
Assessment
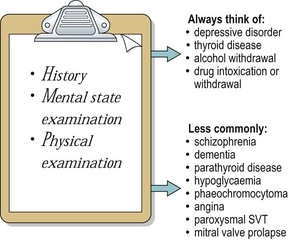
The differential diagnosis of anxiety disorders is shown in Figure 1. It is important to exclude depressive disorder in every case by asking questions about mood, suicidal thoughts, sleep, appetite and energy. Alcohol and substance misuse often occurs as a result of ‘self-medication’ for anxiety disorder and withdrawal states are often accompanied by anxiety. A full blood count and liver function test may reveal covert alcohol problems. Schizophrenia should also be considered. A person with agoraphobia may be unable to go to a supermarket because of the fear of having a panic attack there. In contrast, a patient with schizophrenia may avoid the supermarket because of the delusional belief that their movements in shops are monitored on video cameras by terrorists.
Treatment
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree