Artifacts
▲ Cardiac Artifacts
Types
Electrocardiographic
Pacemaker
Pulse
Ballistocardiographic
Descriptions
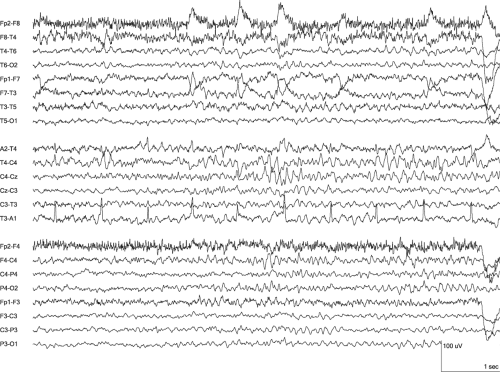
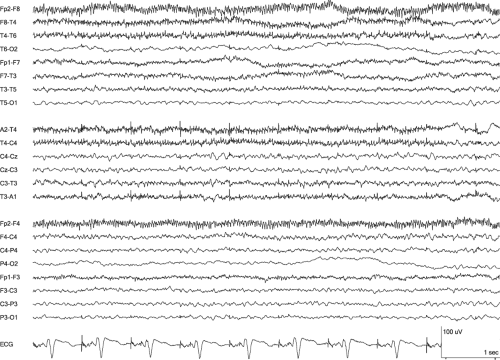
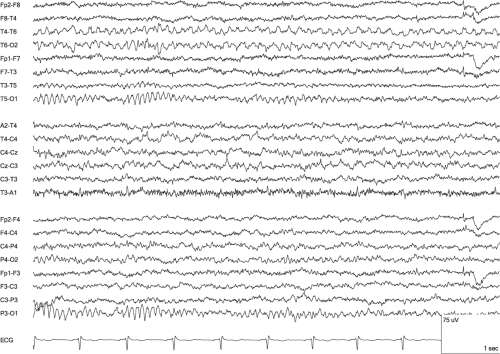
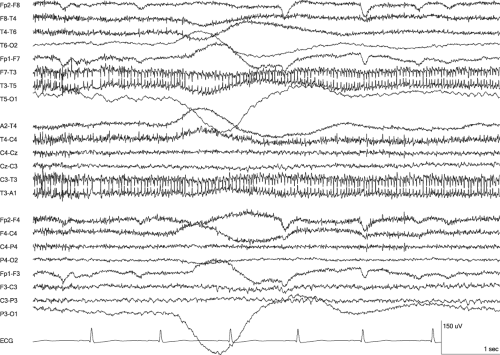
The heart produces two types of EEG artifact, electrical and mechanical. Both types are time-locked to cardiac contractions and most easily identified by their co-occurrence with complexes in the electrocardiogram (ECG) channel. The electrical artifact actually is the ECG, as recorded from head electrodes, but it may not appear as obvious ECG because of the distance from the heart and the suboptimal axis for visualizing ECG complex details. Overall, it is most prominent when the neck is short. Within the ECG artifact, the P wave and T wave usually are not evident, and it appears as a poorly formed QRS complex (Reilly, 1999). Specifically, the QRS more often appears diphasic than triphasic, but it sometimes may be monophasic. Overall, ECG artifact is best formed with referential montages because of the greater interelectrode distances and ECG field’s approximately equal potential across the head. Because of this equipotential field, montages with an average reference have minimal ECG artifact (Cooper et al., 1974). With bipolar montages, ECG artifact occurs with maximum amplitude and clearest QRS waveform over the temporal regions and it often is better formed and larger on the left side (Fisch, 1999). The R wave is most prominent in channels that include the ear electrodes and may demonstrate a transverse dipole across the head with the A1 electrode positive and the A2 electrode negative (Blume et al., 2002). ECG artifact may occur inconsistently, but even when it does not occur with every contraction of the heart, it may still be identified without an ECG channel by observing that the intervals between the artifacts occur in multiples of an essentially similar time interval. This periodicity differs from the periodicity of periodic epileptiform discharges (PEDs), such as periodic lateralized epileptiform discharges (PLEDs), because gaps in the occurrence of PEDs do not have durations that are a multiple of the interdischarge interval. An irregular interval between ECG artifacts also can be caused by a cardiac arrhythmia. For either cause of irregular intervals, the QRS complexes in an ECG channel are particularly helpful to identify the artifact.
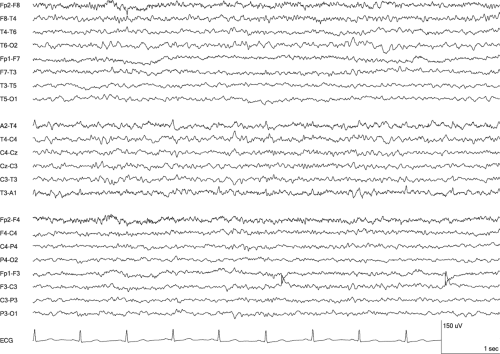
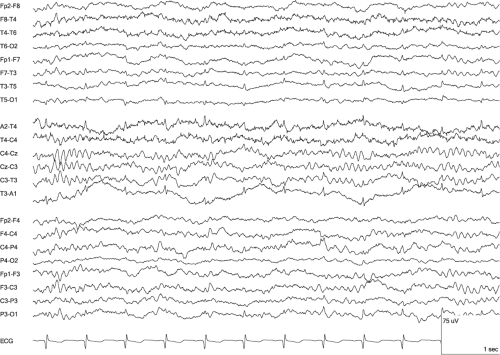
Cardiac pacemakers produce a different electrical artifact. It is distinct from ECG artifact in both its distribution across the head and its waveform. Pacemaker artifact has a broader field and may be generalized. Occasionally, it is present at several, nonadjacent electrode locations, which suggests artifact because of the implausibility of a cerebral generator. The waveform comprises high-frequency polyphasic potentials with a combined duration that is shorter than ECG artifact duration (Fisch, 1999).
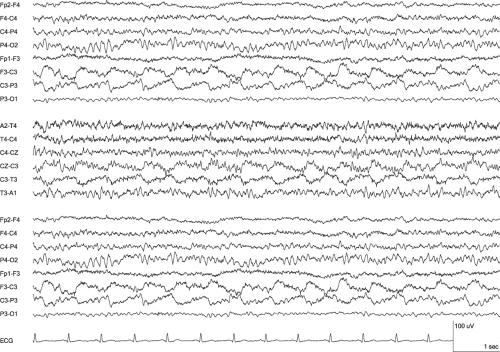
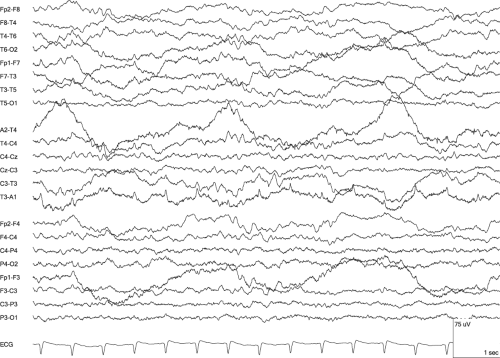
Mechanical artifact from the heart arises from the circulatory pulse and may be considered as a type of electrode artifact. It occurs when an electrode rests over a scalp blood vessel manifesting the pulse and it appears as a periodic slow wave with a regular interval. It typically follows the ECG artifact’s peak by about 200 milliseconds (Blume et al., 2002; Reilly, 1999). Sometimes it has a saw-tooth or sharply contoured waveform (Cooper et al., 1974). Pulse artifact occurs most commonly over the frontal and temporal regions and less commonly over the occiput; however, it may be present anywhere (Fisch, 1999). Touching the electrode producing the artifact can help identify it by both confirming the movement of the electrode with the pulse and altering the artifact’s appearance on EEG as pressure is applied.
Ballistocardiographic artifact is another form of mechanical cardiac artifact. It results from the slight movements of the head or body that occur with cardiac contractions. This may be partly due to the pulsatile force on the aortic arch from the abrupt redirection of blood flow. Ballistocardiographic artifact is similar in waveform to pulse artifact, but is more widespread. If it is due to electrode lead movement, it may involve one or a few electrodes. If it is due to movement of the head when the patient is supine, it includes a collection of posterior electrodes and is altered by repositioning the head or neck on a pillow. Occasionally, ballistocardiographic artifact is generalized.
Distinguishing Features
• Compared to Benign Epileptiform Transients of Sleep
Like benign epileptiform transients of sleep (BETS), ECG artifact typically comprises individual transients that are of low amplitude, are unchanged in waveform, and occur in the midtemporal regions. The temporal correspondence to simultaneously recorded ECG is the best means to differentiate these two patterns. If an ECG channel is not present, identifying the wave in full wakefulness excludes the possibility of BETS, and identifying a regular interval between the waves supports ECG artifact. The interval between waves may vary but should be considered regular if it varies in multiples of a reasonable time interval between heart contractions. Another distinguishing feature is the typical occurrence of ECG artifact bilaterally synchronous. This may occur with BETS but only in a small minority of the occurrences.
• Compared to Focal Ictal and Interictal Epileptiform Discharges
ECG artifact may disrupt the EEG’s background activity similarly to epileptiform discharges. Moreover, it usually is diphasic or triphasic with a fast component that has a duration within the spike range. When the artifact occurs either with a highly regular interval or can be compared to an ECG channel, differentiating it from interictal epileptiform discharges (IEDs) is straightforward. An episodic occurrence pattern requires careful scrutiny of the waveform and location. ECG artifact almost always occurs in channels that include electrodes that are low on the head, especially ear or mastoid electrodes. When a wave only occurs in such channels and has a perfectly conserved waveform, it is likely to be ECG artifact. IEDs show greater variation between occurrences than ECG artifacts even when they recur as the same wave type; that is, they vary more in amplitude, duration, contour, and location than ECG artifact.
Paroxysmal tachycardia may produce ECG artifact that resembles an ictal pattern. Identifying it as artifact relies on the features that are used for distinguishing IEDs, including conservation of waveform and temporal association with the QRS complex in an ECG channel. The regular interval feature also is helpful because the artifact also will likely be present at times between the episodes of tachycardia.
• Compared to Periodic Epileptiform Discharges
The diphasic or triphasic morphology and periodic occurrence pattern are features that PEDs and ECG artifact share. Differentiating these waves is straightforward when comparison to an ECG channel is possible. When an ECG channel is not present, the regularity of the intervals between the transients is the key distinguishing feature. PEDs usually are not nearly as regular in their interval as ECG artifact. This is especially true because the conditions for recording an EEG do not produce significant changes in heart rate. Other distinguishing features are distribution and frequency. Although ECG artifact may be unilateral, it often is bilateral, and PLEDs, by definition, are not bilaterally synchronous. Bilateral periodic epileptiform discharges (BiPEDs) are bilaterally synchronous; however, BiPEDs usually have large, bifrontal fields and ECG artifact is usually maximal in the two temporal regions. The BiPEDs of Creutzfeldt–Jakob disease provide one exception to this distinguishing feature because they may be bilateral without a large field. Frequency is a less reliable means for differentiation. Most ECG artifact will be at 1 Hz or faster because a heart rate slower than 60 beats per minute is unusual. In contrast, PEDs usually occur with intervals greater than 1 second. However, the interval between PEDs varies, especially across different etiologies.
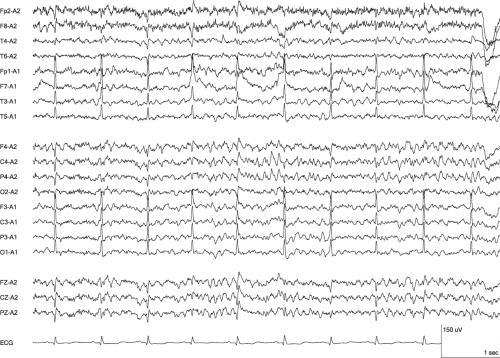 Figure 4-2 ECG Artifact • This segment is the same as Figure 4-1, but presented in an ipsilateral ear referential montage. The ECG artifact remains predominant on the left side, but now also is more evident on the right in channels with greater interelectrode distances. The ear electrodes demonstrate the opposite polarity for the artifact due to the heart’s dipole. (LFF 1 Hz, HFF 70 Hz) |
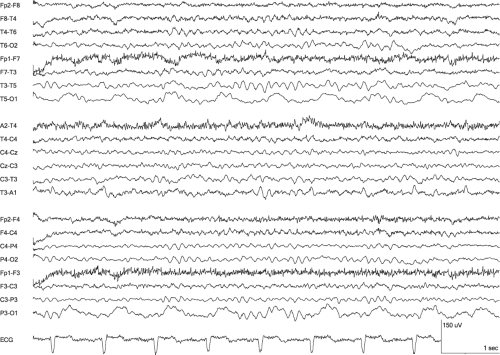 Figure 4-5 Pulse Artifact • Focal slow waves are present at the left occiput. The circulatory pulse cause is not as evident as in Figure 4-4 because of the lower amplitude and location at the end of a bipolar chain. However, the slow waves follow each heart contraction, as indicated in the ECG channel, are limited to the O1 electrode, and were eliminated by repositioning of the O1 electrode. (LFF 1 Hz, HFF 70 Hz) |
▲ Electrode Artifacts
Types
Electrode pop
Electrode contact
Electrode/lead movement
Perspiration
Salt bridge
Movement
Descriptions
Electrode artifacts usually manifest as one of two disparate waveforms, brief transients that are limited to the channels of one electrode and low-frequency rhythms across a scalp region (Tatum et al., 2011b). The brief transients may be due to either spontaneous discharges of an electrical potential that was present between the electrode and the subjacent skin or due to mechanical disturbances to the electrode or its attached lead. The spontaneous discharges are called electrode pops, and they reflect the ability of the electrode and skin interface to function as a capacitor and store electrical charge across the electrolyte paste or gel that holds the electrode in place. With the release of the charge, a sudden direct current (DC) potential appears in all channels that include the electrode (Misulis, 1997). This potential may be superimposed on the background activity or replace it (Blume et al., 2002; Brittenham, 1990). Sometimes more than one pop occurs within a few seconds, which typically indicates a more problematic recording condition. This may be due to a loose electrode, corrosion of the electrode, drying of the electrolyte paste or gel, or a poor connection of the electrode to the amplifier. Electrode pop has a characteristic waveform of a very steep rise and a slower fall. Essentially, it resembles the calibration pulses of analog EEG machines. This shape of a right triangle and field limited to one electrode makes the electrode pop highly recognizable.
Poor electrode contact or lead movement can produce artifact with a waveform that is less consistent across occurrences than the electrode pop’s waveform. Poor contact produces instability in the impedance, which leads to sharp or slow waves of varying waveform and amplitude. These waves often recur as ongoing activity and may be rhythmic if the poor contact occurs in the context of rhythmic movement, such as from a tremor (Fisch, 1999). Just as the electrode pop, it is limited to the channels of the one problematic electrode. Lead movement may include the channels of one or more electrodes, depending on the extent of the movement, and it has a more noise-like waveform that does not resemble cerebrally generated EEG activity. It often includes double phase reversals without a plausible field indicating a cerebrally generated source.
The smearing of the electrode paste between electrodes produces in a salt bridge between electrode locations that electrically merges the locations and results in the equivalent of one larger electrode. The artifact from a salt bridge is channel specific and usually lower amplitude than the background, and this contrasts with the individual electrode artifacts, which are electrode specific and usually higher amplitude than the background. The occurrence of salt bridge artifact in only the channels that include the combined electrodes is due to the differential amplification that generates the output present in the channel. The combining of electrodes results in one potential for the two electrodes, so amplification based on the difference between electrodes produces a cancellation. Salt bridge artifact is flat and can be close to isoelectric.
Perspiration artifact has similarity to salt bridge artifact due to the merging of electrode locations through the salinity of perspiration, but the cancellation is not as complete or as stable. Perspiration artifact is manifested as low amplitude, undulating activity that typically has wave durations greater than 2 seconds; thus, the waves are below the frequency range of clinical EEG (Fisch, 1999). The artifact may appear as an unstable baseline for the other EEG activity, and even may cause adjacent channels to cross in the display despite their low amplitude. The instability is due to shifts in the DC offset potential from the varying perspiration (Cooper et al., 1974). Perspiration artifact typically includes several channels representing the electrodes across a region of scalp. Salt bridge artifact differs from perspiration artifact by being lower in amplitude, not wavering with low-frequency oscillations, and often including only one channel.
Distinguishing Features
• Compared to Ocular Artifact
Slow roving eye movements produce an artifact that has a frequency and field similar to that of perspiration artifact. They are involuntary and repeated horizontal ocular movements that occur in drowsiness with a relatively constant period (Santamaria and Chiappa, 1987). As lateral movements, they demonstrate a phase reversal because of the eyes’ dipoles. With right gaze, the field around the right frontal–temporal electrodes becomes more positive and the field around the left frontal–temporal electrodes becomes more negative. This produces a phase reversal not seen with salt bridge artifact, even when the low-amplitude activity happens to be rhythmic. The key features to differentiate from electrode artifact are the regular rhythmicity, phase reversal, and broad, bifrontal field.
• Compared to Focal Interictal Epileptiform Discharges
Electrode pop resembles IEDs. Both occur as paroxysmal, sharply contoured transients that interrupt the background activity. However, electrode pop involves only one electrode; therefore, it does not have a field indicating a gradual decrease in the potential’s amplitude across the scalp. The lack of a field including multiple electrodes is highly rare for IEDs except in young infants. The waveform of electrode pop also differs from IEDs by having a much steeper rise and a contrasting, slower fall.