Atlanto-Occipital Injuries
Paul A. Anderson
Craniocervical injuries including atlanto-occipital dislocations, craniocervical disassociations, and occipital condyle fractures involve trauma to the complex articulation including the occipital bone, the occipitoatlantal articulation, the atlas, the axis, and the ligaments that span from the axis to occiput. This region is characterized by relatively large hard bony structures and strong ligaments, thus providing excellent stability to protect the brainstem and upper spinal cord. Injury to the craniocervical junction will almost always be caused by high-energy trauma and is associated with other injuries to the head, face, and cervical spine in a majority of cases. In fatal traffic deaths, craniocervical injuries account for 10% to 25% of cases (1).
Prior to the last decade, only bilateral atlanto-occipital dislocations were reported either in autopsy analyses or case reports of rare survivors. However, craniocervical injuries are now recognized as belonging on a spectrum of injury patterns with varying degrees of stability. The use of imaging protocols to identify significant cervical injuries of all blunt trauma patients has led to recognition of a variety of craniocervical injuries. Variants range from occipital condyle fractures with limited risk of instability to bilateral atlanto-occipital dislocations. Cases may be unilateral or only associated with vertical distraction (or diastasis between the skull and cervical spine) without translation. These varieties of injury patterns have changed decision making so that not all patients having craniocervical instability require surgical treatment.
Craniocervical injuries are becoming more commonplace for several reasons. Airbags appear to protect the chest and subaxial cervical spine but may not stop rapid deceleration forces of the head, which can disrupt the craniocervical junction (2,3). This is particularly true in children, which accounts for the higher incidence in that population (4). Increased imaging, especially multidetector CT, had allowed earlier diagnosis and potentially lifesaving early management (5). In questionable cases, MRI can be used to confirm suspicion of injury at the craniocervical junction. Overall improvement in the transport of injured patients, early resuscitation, better training of hospital personnel, and a collaborative approach to care have also improved the survivability of patients from this injury (5).
Although the basic biomechanical understanding of craniocervical injury has not changed since the landmark thesis by Werne (6), the ability to diagnose injury based on plain radiographs and CT has significantly improved. Although accurate diagnosis can be made from plain radiographs, CT is used as the primary screening tool and thus the preferred test to identify a possible craniocervical injury. This has decreased the time to diagnosis and the incidence of delay in diagnosis; however, cases of catastrophic failure to diagnosis and subsequent neurologic deterioration have recently been reported (7,8).
This chapter will review the anatomy and criteria used to diagnose occipital condyle fractures and craniocervical injuries. New classification systems utilizing modern imaging and the increased understanding of the pathophysiology of injury will be used to develop rationale treatment strategies.
ANATOMY OF CRANIOCERVICAL
BONY ANATOMY
Occiput
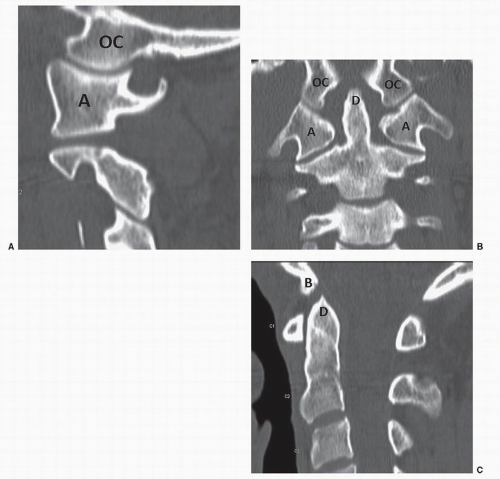
The occiput forms the major portion of foramen magnum. From the anterolateral aspect of foramen magnum, the occipital condyles project caudally on each side. These are semilunar in shape forming almost a 180-degree arc when viewed laterally (Fig. 45.1A). From the frontal view, they are wedge shaped being taller medially (Fig. 45.1B). The occipital condyles articulate with the lateral masses of the atlas forming a synovial joint with a joint capsule. Just lateral and ventral to the occipital condyles are the hypoglossal foramen and the CN XII explaining the high prevalence of injury to these in conjunction with occipital condyle fractures. The ventral aspect of foramen magnum is bounded by the basion, which is the caudal extent of the clival plate. The dorsal boundary of foramen magnum is the opisthion.
Atlas
The atlas forms a ring-shaped structure, which acts like a bushing to facilitate atlantoaxial rotation. The ring is formed from large lateral masses connected together by thin ventral and dorsal arches. The lateral masses viewed
from the front are trapezoidal in shape with the long side facing laterally to create a mirror image of the occipital condyles. The lateral masses form a cup in which lie the paired occipital condyles.
from the front are trapezoidal in shape with the long side facing laterally to create a mirror image of the occipital condyles. The lateral masses form a cup in which lie the paired occipital condyles.
Axis
The axis is an essential component of the craniocervical articulation as all the major restraining ligaments attach between the axis and occiput and not directly to the atlas. The dens tip, which extends behind the ventral arch of the atlas, is held in close relationship to the basion by the alar ligaments (Fig. 45.1C). The lateral masses of the C2 are directly under those of C1 thus directly supporting them.
LIGAMENTOUS ANATOMY
The craniocervical junction is unique by not having ligamentum flava or intervertebral disk, which is characteristic of the rest of the spinal column. The ligamentous structures of the craniocervical junction can be divided into the internal (which lie within the spinal canal) and the external (which lie outside the spinal canal).
The external ligaments include the ligamentum nuchae, the anterior and dorsal occipitoatlantal membranes, and the occipitoatlantal and atlantoaxial facet joint capsules. The anterior and dorsal occipitoatlantal membranes are thin structures and offer little protection to the dura during surgical approach. The facet joint capsules are thin and redundant to facilitate wide range of motion.
The internal ligaments are the major stabilizers between the occiput and C2 and are essential to maintain life. The most important are the alar ligaments, which are paired, strong, thick cord-like structures that project laterally and ventrally from the dens tip to the ventral medial aspect of the occipital condyles. The tectorial membrane is a flat band-like continuation of the posterior longitudinal ligament, which attaches to the basion. The apical ligament is a rudimentary structure extending from the dens to the ventral midpoint of foramen magnum. The cruciate ligament lying behind the dens consists of the transverse ligament and fibers that extend upward to attach to the basion and caudally to the axis.
KINEMATICS
The craniocervical junction, despite its mechanical importance, has a wide range of motion. Werne (6) and others have shown that the occipitocervical motion has 15, 8, and 0 degrees of motion in flexion-extension, lateral bending, and axial rotation (9). Atlantoaxial motion is 10, 0, and 47 degrees in flexion-extension, lateral bending, and axial rotation.
BIOMECHANICS
Careful biomechanical studies have identified the alar ligaments and tectorial membrane as the major stabilizers of the craniocervical junction (6,10). Flexion is limited by impaction of the basion and dens tip while extension is limited by the tectorial membrane. The alar ligaments check both lateral bending and axial rotation of both the occipitoatlantal and atlantoaxial articulations. Distraction is limited by both the alar ligaments and tectorial membrane. The atlanto-occipital joint should always be congruent and should never have greater than 2 mm of joint space.
MECHANISM OF INJURY
High velocity is required to injure the craniocervical junction. These injuries are usually secondary to rapid deceleration or cranial impaction. In a review of 17 cases of craniocervical disassociation, Bellabarba et al. (8) reported that 11 had motor vehicular crashes, three children versus automobile and three from falls from significant height. Although occipital condyle fractures are by far the most common injury, the more serious unstable injuries are secondary to tensile failure of the alar ligaments and tectorial membrane. These occur more often in children due to shallower articulations, greater head size to body mass, and injury mechanism such as vehicular versus pedestrian or from airbags and seat belts where large decelerationacceleration forces to the head occur (4).
DIAGNOSIS
The diagnosis of craniocervical injury should be suspected in all blunt trauma patients. After resuscitation, patients are evaluated for spinal tenderness and by neurologic examination. Because cranial trauma and other injuries are common, distracting injury or impaired consciousness preclude adequate evaluation in many patients. Patients who have spinal symptoms, who are obtunded, or who have distracting injuries should undergo radiographic evaluation. If CT is being performed, then the inclusion of cervical spine CT is timely and cost-effective. Further, the diagnostic sensitivity (especially at the craniocervical junction) is significantly better than plain radiographs. However, the potential for harmful effects of radiation from diagnostic CT should be considered, especially in children. As an alternative, a three-view cervical spine series can be performed.
The physical examination is critical and is performed by palpating the spine from the occiput to sacrum for tenderness. The patient should then be rotated and the neck and back visually inspected. Pain and tenderness in the upper cervical spine will increase likelihood of a craniocervical injury, although it may not be present due to cognitive impairment of the patient. Neurologic examination should include reflexes, level of consciousness (Glasgow Coma Score), the cranial nerves, and motor and sensory function of all four extremities and perineum.
Occipital condyle fractures are rarely visualized on plain radiographs and almost always diagnosed from head or cervical spine CT. Reformations of the occipitoatlantal articulation in coronal and sagittal planes is essential to determine their stability. Displacement indicates rupture of the internal craniocervical ligaments and instability.
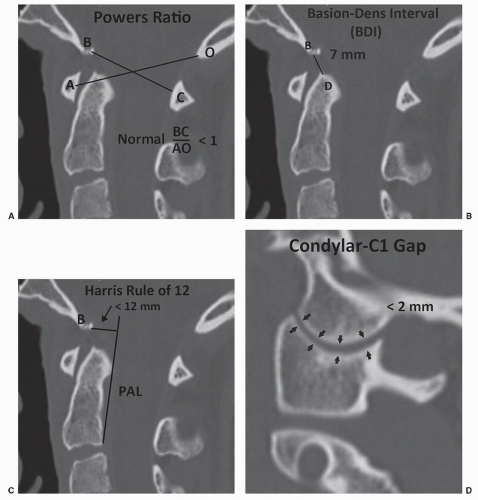
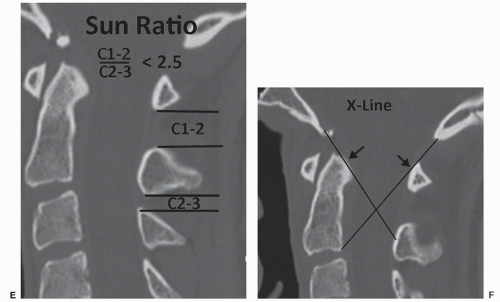
Several methods have been described to identify craniocervical injury. Powers described calculating the ratio of distances from the basion to dorsal arch of C1 and opisthion to the ventral arch of the C1 (Fig. 45.2A and 45.2) (11). This ratio should be less than 1.0 and ratios greater than 1.0 are associated with atlanto-occipital dislocation. Harris described the “Rule of Twelve” based on intervals between the basion to the dens (BDI) and the basion to the posterior axial line (Fig. 45.2B and C) (12). Normally both of these are less than 12 mm. If either of the distances is greater than 12 mm, then atlanto-occipital dislocation is likely present. The condylar-C1 interval (CCI) is the distance between the occipital condyles and C1 lateral masses (Fig. 45.2D) (7,13). The space is congruent on both frontal and lateral projections but can be evaluated only on CT or MRI. Another ratio used in children is the ratio of the interspinous intervals between the C1-C2 and C2-C3 described by Sun et al. (14) (Fig. 45.2E). When this is greater than 2.5, a craniocervical injury should be considered. Lee proposed the X-line method (Fig. 45.2F). This test is positive if the line from basion to the C2 spinolaminar point does not intersect the dens or the line from the dorsolateral corner of C2 to the opisthion does not intersect C1 (15).
Several investigators have evaluated the reliability of these criteria to diagnose craniocervical displacement based on modern imaging (Table 45.1). Dziurzynski et al. (16) compared five methods using both CT and plain radiographs. Plain radiographs were only readable in 40% to 80% of cases while CT was in all cases. The condylar-C1 distance and the basilar-dens interval had 100% sensitivity and 90% specificity. The Powers ratio and Harris rule had poor diagnostic parameters. Pang et al. (7) also compared
five methods and similarly found that the condylar-C1 interval had 100% sensitivity. He, similar to Dziurzynski, reported poor sensitivities and specificities for the Powers ratio, Sun ratio, and Harris rule.
five methods and similarly found that the condylar-C1 interval had 100% sensitivity. He, similar to Dziurzynski, reported poor sensitivities and specificities for the Powers ratio, Sun ratio, and Harris rule.
MRI imaging is highly effective for identifying ligamentous injury to the tectorial membrane and alar ligaments and displacement of the craniocervical articulations. Pang critically evaluated 16 patients with craniocervical injury and documented associated findings including ventral prevertebral edema, subarachnoid hemorrhage along the brainstem, epidural and subarachnoid hemorrhage in the upper cervical spinal cord, transverse ligament rupture,
and distraction of the atlantoaxial joints (7). This latter injury is common and highlights the integral relationship between the occipitoatlantal and atlantoaxial joints, both being prevented from vertical displacements by the alar ligaments and tectorial membrane. In 13 cases, the injury occurred bilaterally, while in three patients the injury was unilateral. The use of coronal views and fat suppression techniques may increase the likelihood of identifying craniocervical ligament injury. However, MRI may be overly sensitive and identify many insignificant areas of hemorrhage or edema.
and distraction of the atlantoaxial joints (7). This latter injury is common and highlights the integral relationship between the occipitoatlantal and atlantoaxial joints, both being prevented from vertical displacements by the alar ligaments and tectorial membrane. In 13 cases, the injury occurred bilaterally, while in three patients the injury was unilateral. The use of coronal views and fat suppression techniques may increase the likelihood of identifying craniocervical ligament injury. However, MRI may be overly sensitive and identify many insignificant areas of hemorrhage or edema.
TABLE 45.1 Sensitivities and Specificities of Diagnostic Criteria for Craniocervical Instability | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree