♦ Preoperative
Imaging
- Computed tomography (CT) with sagittal reconstructions
- Presence of an aberrant vertebral artery or small C2 pars interarticularis may prohibit transarticular screw fixation.
- Bony anatomy such as the length of C1 lateral mass and C2 pars interarticularis should be measured carefully and used as a guide for screw selection in the operating room.
- Presence of an aberrant vertebral artery or small C2 pars interarticularis may prohibit transarticular screw fixation.
- X -ray
- Flexion and extension views to determine the amount of instability and the reducibility of a fracture or abnormality
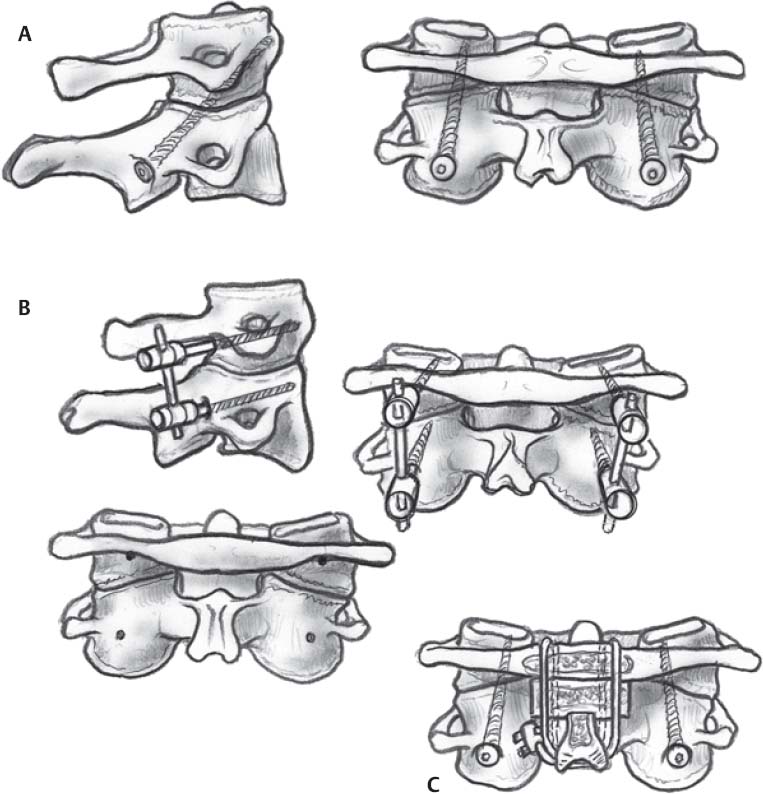
♦ Transarticular Fusion (Fig. 92.1A)
Equipment
- Cervical spine tray
- Mayfield head holder (radiolucent if using frameless stereotaxy)
- High-speed drill
- Triton drill (Medtronic)
- Kirschner wire (K-wire), 1.2 mm
- Cannulated self tapping screw, 3.5 to 4 mm (diameter) by 35 to 50 mm (length)
Operating Room Set-up
- Bipolar and Bovie cauterization
- Neuromonitoring
- Fluoroscopy
- Frameless stereotaxy
Anesthetic Issues
- Coordination between the anesthesia and neuromonitoring teams
- Prone
- Mayfield head holder
- Cervical flexion to help achieve appropriate trajectory for screw placement (fluoroscopic guidance should be used)
- Arms tucked
- Hip area left exposed for graft harvest
Surgical Steps
- Midline exposure from occiput to C4
- Subperiosteal exposure of C1 and C2, including the C1–C2 joint interface and C2 pars interarticularis
- Removal of ligamentum flavum at C1–C2 interface to expose the lateral dural margin and medial portion of the C2 pars interarticularis
- Superior retraction of C2 nerve root
- Localization of the screw insertion point on inferior C2 facet at a position 2 to 3 mm lateral and inferior to the middle of the facet joint
- Pilot hole drilling with a K-wire. Sagittal angulation is determined using lateral fluoroscopy; the screw tip should be aimed toward the middle of the anterior tubercle of C1. Medial angulation is usually 0 to 10 degrees and should be chosen so that the screw travels down the middle of the C2 pars inter-articularis. It may be necessary to place the screws percutaneously through stab incisions at T1–T2 to achieve the appropriate trajectory, especially when cervical flexion is limited.
- Placement of cannulated screw over K-wire under fluoroscopic guidance. The surgeon should feel the vertebrae lock together and stiffen as the screw passes across the C1–C2 joint. When the bone is particularly hard, tapping, drilling, or both over the K-wire is suggested before screw placement.
- Unilateral or bilateral transarticular screw fusions are strengthened by the addition of interspinous fusion.
♦ C1 Lateral Mass and C2 Pars Fusion (Fig. 92.1B)
Equipment
- Cervical spine tray
- Mayfield head holder
- High-speed drill
- 3.5-mm, partially threaded, polyaxial screws for C1 lateral mass (30 mm length norm)
- 3.5-mm, fully threaded, polyaxial screws for C2 pars (16 mm length norm)
- Rod connectors
Operating Room Set-up
- Bipolar and Bovie cauterization
- Neuromonitoring
- Fluoroscopy
- Operative microscope
- Coordination between anesthesia and neuromonitoring teams needs to be maintained
Positioning
- Prone
- Mayfield head holder
- Cervical positioning with neutral (reduced) alignment using fluoroscopic guidance
- Arms tucked
- Hip area exposed for graft harvest (see section on intraspinous fusion)
Surgical Steps
- Midline exposure from occiput to C4
- Subperiosteal exposure of C1 and C2, including the C1–C2 joint interface and the C2 pars interarticularis
- Removal of ligamentum flavum at C1–C2 interface to expose the lateral dural margin and medial portion of the C2 pars interarticularis
- Inferior retraction of the C2 nerve root
- Exposure of C1 lateral masses
- Localization of insertion point for the C1 lateral mass screw in the midpoint of the lateral mass. A slight medial and cephalad screw trajectory is optimal.
- Screw tracts are hand-drilled under fluoroscopy. Then, 3.5-mm partially threaded screws are inserted. Thread length is determined by the dimensions of the lateral mass. Screws should be seated so that ~10 mm of unthreaded length is present posterior to the lateral mass to facilitate rod placement between the C1 and C2 screws.
- Localization of the pars screw insertion point on the inferior C2 facet at a position 2 to 3 mm lateral and inferior to the middle of the facet joint. Medial angulation is usually 0 to 10 degrees and should be chosen so that the screw travels down the middle of the C2 pars interarticularis. A 20-degree cephalad trajectory is used.
- Screw tracts are hand-drilled under fluoroscopy no deeper than the posterior margin of the C2 body as indicated by lateral fluoroscopy.
- Titanium rods are used to connect the fusion construct.
- These fusions are strengthened by the addition of interspinous fusion.
♦ Interspinous Fusion (Fig. 92.1C)
Equipment
- Cervical spine tray
- Mayfield head holder
- High-speed drill
- Iliac crest bone graft harvest set
- Single titanium cable with tensioner and cutter
- Bipolar and Bovie cauterization
- Neuromonitoring
Anesthetic Issues
- Coordination between anesthesia and neuromonitoring teams needs to be maintained
Positioning
- Prone
- Mayfield head holder
- Cervical positioning with neutral (reduced) alignment using fluoroscopic guidance
- Arms tucked
- Hip area exposed for graft harvest
Surgical Steps
- Midline exposure from occiput to C2
- Subperiosteal exposure of C1 and C2
- Removal of the ligamentum flavum and posterior occipitoatlantal membrane at C1 and C2
- Decortication of inferior C1 ring and superior C2 spinous process surfaces that will contact the interspinous graft
- Harvest of iliac crest graft and contouring to make a bicortical graft that fits firmly between the posterior arch of C1 and spinous process of C2. To obtain an appropriate fit, the graft is notched at the point where it contacts the C2 spinous process.
- Passage of a single cable under the arch of C1, around the graft, and over the spinous process of C2
- Tightens cable traps and compresses the graft anteriorly and posteriorly.
♦ Postoperative
- Patients usually wear a rigid cervical collar for 4 weeks.
- Postoperative CT is obtained to verify positioning of the screw.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue