Autism and the Pervasive Developmental Disorders
Fred R. Volkmar
Catherine Lord
Ami Klin
Robert Schultz
Edwin H. Cook
The pervasive developmental disorders (PDDs) comprise a group of neuropsychiatric disorders characterized by specific delays and deviance in social, communicative, and cognitive development, with an onset typically in the first years of life. Although commonly associated with mental retardation, these disorders differ from other developmental disorders in that their behavioral features are distinctive and do not simply reflect developmental delay (1). Although better definitions of the syndrome continue to be needed, the validity of autism as a diagnostic category is now well established. In addition to autism, various other disorders are included with the PDD class in DSM-IV. These include Asperger’s disorder, Rett disorder, childhood disintegrative disorder (CDD), and the “subthreshold” concept of pervasive developmental disorder not otherwise specified (PDD-NOS) (2), The validity of these other proposed PDDs has been more controversial (3). Collectively, these conditions are also often referred to as the autism spectrum disorders (ASDs).
Autistic Disorder
Definition
The DSM-IV (2) definition of autism was developed on the basis of a very large, international, multisite field trial. This definition retains historical continuity with previous definitions of autism but differs from its immediate predecessor in that age of onset (before age 3 years) is included as a necessary diagnostic feature and criteria are more conceptually framed. Diagnostic criteria are presented in Table 5.1.1.1.
The characteristic social and communicative deficits are believed to be aberrant relative to the person’s developmental level (1); consistent with Kanner’s original report and subsequent research, social difficulties in autism are a key diagnostic feature 4,5,6. Complexities for definitions of autism have included the broad range of syndrome expression, changes in syndrome expression with age, and differentiation from other psychiatric and developmental disorders 3,6.
History
Kraeplin’s description of dementia praecox was rapidly extended to children, and the terms childhood schizophrenia and childhood psychosis became synonymous. Early assumptions that all severe childhood disturbance must be a form of schizophrenia were based, in large part, on severity. Kanner’s 1943 (4) description of 11 cases of “early infantile autism” noted various ways in which this disorder appeared to be distinctive. These cases exhibited an apparently congenital inability to relate to other people (in contrast to an apparent ability and overconcern with the nonsocial environment); their language (when it developed at all) was remarkable for echolalia, pronoun reversal, and concreteness. Behaviorally, these children engaged in repetitive, apparently purposeless activities (stereotypy), and were intolerant of change. Kanner’s use of the term autism was meant to convey the unusual, self-centered quality that his cases exhibited, but it was also suggestive of the autism associated with schizophrenia. Although Kanner’s description has been remarkably enduring, early speculations about certain aspects of the condition (e.g., normal levels of intelligence, lack of association with other medical conditions, unusual levels of parental education) proved incorrect (3). The validity of autism was established over the next several decades only, as various lines of evidence became available (3). Autism was included in the landmark third edition of the DSM (DSM-III) (7). The initial definition of the condition in DSM-III lacked an appreciation of developmental change and was modified
in DSM-III-R (8). Unfortunately, while DSM-III-R was more developmentally organized, it proved problematic as it appeared that the diagnostic construct was overly broadened (3). As a result, substantial revisions were made in the DSM-IV (6). Table 5.1.1.2 summarizes historical highlights in the development of the concepts of childhood psychosis and autism.
in DSM-III-R (8). Unfortunately, while DSM-III-R was more developmentally organized, it proved problematic as it appeared that the diagnostic construct was overly broadened (3). As a result, substantial revisions were made in the DSM-IV (6). Table 5.1.1.2 summarizes historical highlights in the development of the concepts of childhood psychosis and autism.
TABLE 5.1.1.1 DSM-IV Criteria for Autistic Disorder (299.0) | ||
|---|---|---|
|
Epidemiology
More than 40 epidemiological studies have been published; in his review, Fombonne (9) reports prevalence estimates in studies conducted since 1987 ranging from 2.5 to 72.6 per 10,000 with a median rate of 11.3 per 10,000. There does appear to be an increase in reported prevalence over time, although several factors complicate the interpretation of this observation. For example, there is more public awareness of autism, and criteria for the condition have been changed and probably effectively broadened the concept. Furthermore, the lay press and public often equate the notion of “autism spectrum disorder” with more strictly defined autism (10). Other factors accounting for discrepancies include differences in screening and ascertainment procedures, and the size of target populations (with higher rates generally reported in studies with smaller samples). Although an increase in reported rates might reflect an actual increase in incidence, other factors, such as case definition and recognition, are important. Thus, newer studies are more likely to adopt broader definitions of autism. Selected epidemiological reports are summarized in Table 5.1.1.3.
TABLE 5.1.1.2 DEVELOPMENT OF DIAGNOSTIC CONCEPTS: CHILDHOOD “PSYCHOSIS” | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 5.1.1.3 SELECTED EPIDEMIOLOGICAL STUDIES OF AUTISM | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Consistent with gender proportion found in clinically referred samples (11), Fombonne (9) reported an average gender ratio across studies of 4.3 males for every female. However, this ratio varies with level of associated intellectual disability, as females are more likely to exhibit associated intellectual disability.
Etiology
Kanner’s initial report of the autistic syndrome emphasized the apparently congenital nature of autism, but also noted the remarkable degrees of occupational success observed in the parents of these first patients, as well as evident deficits in parent–child interaction (4). These latter observations were subsequently taken to suggest some role of parental psychopathology in syndrome pathogenesis. During the 1950s and 1960s, considerable efforts were made to remediate the effects of deviant caregiving practices of cold (“refrigerator”) parents through, for example, extensive child and parent psychotherapy. Various lines of evidence now make it clear that deviant childrearing practices do not account for autism. Parents of children with autism resemble parents of children with other developmental problems; they do not exhibit specific deficits in childrearing practice. Similarly, early studies showing an association of autism with higher social class appear to be artifacts introduced by ascertainment bias; for example, more successful and well educated families are more likely to seek treatment (9). It is clear that the parents of children with autism may be understandably stressed by the experience of caring for a severely impaired child and may suffer from depression and anxiety.
As the validity of autism became more established, various lines of evidence converged to suggest the importance of neurobiological factors in the pathogenesis of this and similar conditions (3). Although the variety and consistency of this evidence are impressive, neither specific biological markers for autism, nor precise pathogenic mechanisms, have been identified. As summarized in Table 5.1.1.4, individuals with autism exhibit an increased frequency of physical anomalies, persistent primitive reflexes, and various neurologic soft signs, as well as increased abnormalities on electroencephalograms (EEGs) (12).
Neurobiological theories in autism have focused on diverse brain regions (12). Theories have also emphasized various brain systems, with differences in emphasis depending on the focus of the research, e.g., those who emphasize difficulty with complex information processing postulate widespread cortical abnormalities with sparing of early sensory and emotional processes, while those focusing on emotional deficits and social difficulties often highlight the role of the limbic system 12,13. Clearly, the severity and pervasiveness of difficulties across multiple areas of development suggest that a functionally diverse and widely distributed set of neural systems is impacted 12,13. However, these affected systems must be discrete, because autism spares certain perceptual and cognitive systems and may, for example, sometimes be observed in individuals with normal IQ or even highly superior skills and talents. Although it is likely that the condition ultimately involves multiple systems, it remains quite possible that the initial insult is relatively circumscribed, with subsequent implications for other aspects of development. Although much work remains to be done, currently available data, including those from postmortem and neuroimaging studies, strongly implicate abnormalities of the limbic system, and circuitry within the temporal and frontal lobes 13,14.
Neuroimaging techniques have become increasingly sophisticated, with improved resolution and measurement precision, and more functional MRI (fMRI) studies have been conducted (13). Structural MRI studies have suggested a possible role of the amygdala, with most studies suggesting that persons with autism have underactive amygdala activity when performing social perceptual and social-cognitive experimental tasks 13,14. This is of interest given the connections and functional relationships of the amygdala to both earlier and later sensory processing systems, as well as to areas of the frontal lobe.
One of the best replicated and more intriguing findings to emerge from the structural MRI literature in the past few years is that overall brain size appears to be increased in autism (by 2 to 10%) (15). Brain size is probably normal at birth and it is not
until the later part of the first year of life that brain size becomes abnormally large. By age 2 to 4 years, brain size is 5 to 10% larger than normal, but after this time, growth may decelerate so that by adulthood brain size may be only slightly larger than normal. It remains unclear whether the increase in brain size is generalized or selective, although recent data suggest that enlargement is greatest in the temporal and frontal lobes, and somewhat greater in the white matter than in the gray (14). One theory suggests that white matter volume increases in autism are caused by overgrowth of short-distance pathways, and that there is actually a decrease in longer-range connections. This abnormal balance of connections is believed to contribute in important ways to the autism neuropsychological phenotype, which includes an inordinate focus on details and difficulties with conceptual understanding. Thus, increased brain size might come at the expense of long-range interconnectivity between specialized neural systems, giving rise to a more fragmented processing structure. Consistent with this theory, several functional neuroimaging studies have now shown abnormal patterns of “functional connectivity.” This type of reduction in neural integration is consistent with one influential theory that attributes autistic symptoms to a lack of “central coherence,” a cognitive processing style that makes the integration of parts into wholes problematic (16).
until the later part of the first year of life that brain size becomes abnormally large. By age 2 to 4 years, brain size is 5 to 10% larger than normal, but after this time, growth may decelerate so that by adulthood brain size may be only slightly larger than normal. It remains unclear whether the increase in brain size is generalized or selective, although recent data suggest that enlargement is greatest in the temporal and frontal lobes, and somewhat greater in the white matter than in the gray (14). One theory suggests that white matter volume increases in autism are caused by overgrowth of short-distance pathways, and that there is actually a decrease in longer-range connections. This abnormal balance of connections is believed to contribute in important ways to the autism neuropsychological phenotype, which includes an inordinate focus on details and difficulties with conceptual understanding. Thus, increased brain size might come at the expense of long-range interconnectivity between specialized neural systems, giving rise to a more fragmented processing structure. Consistent with this theory, several functional neuroimaging studies have now shown abnormal patterns of “functional connectivity.” This type of reduction in neural integration is consistent with one influential theory that attributes autistic symptoms to a lack of “central coherence,” a cognitive processing style that makes the integration of parts into wholes problematic (16).
TABLE 5.1.1.4 NEUROBIOLOGICAL FINDINGS IN AUTISM | |
|---|---|
|
The best replicated functional neuroimaging finding concerns underactivation during face perception tasks of a region on the ventral surface of the temporal lobe during face perception tasks— the fusiform gyrus (17). Because of the specificity of this area for faces, it has come to be known as the fusiform face area (FFA). (Figure 5.1.1.1)
Nearly a half a dozen studies by different groups have shown that older children, adolescents, and adults with autism have reduced levels of responsivity to the human face in the FFA, especially in the right hemisphere. These data are consistent with an extensive psychology literature documenting performance deficits in face and facial expression recognition in autism (18), and they provide an important key to understanding the core social deficits in autism. Studies now show that this cortical tissue processes a wider range of person-related information, and thus it might more accurately be
called the fusiform “person” area. This observation may also be relevant to the observation that individuals with autism have particular difficulties in processing certain facial features/ information, e.g., the tendency of more able individuals with autism to focus on mouths rather than eyes when they observe social interaction (Figure 5.1.1.2) (19).
called the fusiform “person” area. This observation may also be relevant to the observation that individuals with autism have particular difficulties in processing certain facial features/ information, e.g., the tendency of more able individuals with autism to focus on mouths rather than eyes when they observe social interaction (Figure 5.1.1.2) (19).
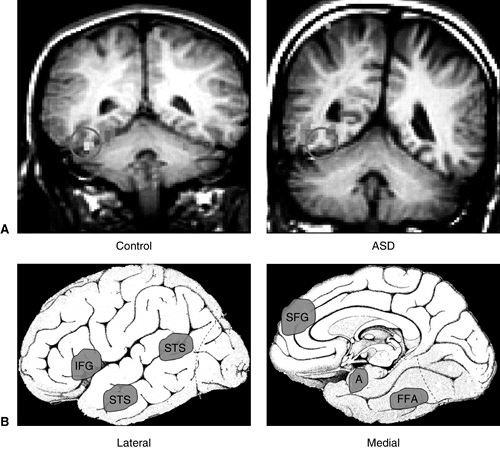 FIGURE 5.1.1.1. Functional MRI abnormalities observed in ASD. A. These coronal MRI images show the cerebral hemispheres above, the cerebellum below, and a circle over the fusiform gyrus of the temporal lobe. The examples illustrate the frequent finding of hypoactivation of the fusiform gyrus to faces in an adolescent male with ASD (right) as compared to an age- and IQ-matched healthy control male (left). The red/yellow signal shows brain areas that are significantly more active during perception of faces; signals in blue show areas more active during perception of nonface objects. Note the lack of face activation in the boy with ASD, but average levels of nonface object activation. B. Schematic diagrams of the brain from lateral and medial orientations illustrating the broader array of brain areas found to be hypoactive in ASD during a variety of cognitive and perceptual tasks that are explicitly social in nature. Some evidence suggests that these areas are linked to form a “social brain” network. IFG = inferior frontal gyrus (hypoactive during facial expression imitation); pSTS = posterior superior temporal sulcus (hypoactive during perception of facial expressions and eye gaze tasks); SFG = superior frontal gyrus (hypoactive during theory of mind tasks, i.e., when taking another person’s perspective); A = amygdala (hypoactive during a variety of social tasks); FG = fusiform gyrus, also known as the fusiform face area (hypoactive during perception of personal identity) 13,14. (See color insert.). |
Although relatively few in number and sample size, postmortem studies have revealed various abnormalities, including a significant decrease in the number of Purkinje cells and granule cells in the cerebellum, likely of prenatal origin (12). However, early reports of decreases in the midsagittal area of cerebella vermal lobules VI and VII have not been independently replicated in studies that control for age and IQ (13). Postmortem studies also have implicated the limbic system, with decreased neuronal size, decreased dendritic arborization, and increased neuronal packing density of neurons in the amygdala, hippocampus, septum, anterior cingulate, and mammillary bodies 12,13. These regions are strongly interconnected, and comprise much of the limbic system— a system that supports social and emotional functioning. Orbital and medial prefrontal cortices have dense reciprocal connections with the amygdala, providing the architecture for a system that can regulate social-cognitive processes. A parallel set of amygdala-cortical circuitry in the temporal lobes focuses on social-perceptual processes. One hypothesis is that autism is largely caused by abnormalities in both of these amygdala-cortical loops. These abnormalities are believed to cause faulty social orientation during early infancy (a failure to attend adequately to interpersonal interactions), which in turn cause failures in social and emotional learning, leading to the hallmark symptoms of autism (13).
Animal models of autism have been attempted. For example, lesion studies of the amygdala in nonhuman primates reveal that lesions made just after birth to the amygdala and/or the hippocampus produce some of the cardinal features of autism over the first year of life, including social isolation, lack of eye contact, expressionless faces, and motor stereotypes. However, the specificity of these findings remains unclear, since the lesions are intrinsically relatively crude and the lesioned animals are also deprived of normal social interactions, since they are reared in isolation. Finally, similar lesions in adulthood fail to produce autistic-like sequellae, strongly suggesting that these circuits may only have a critical early role in social learning 12,13,14.
The role of genetic mechanisms in autistic disorder is suggested by the observation that siblings of affected persons are at a 22-fold or greater risk of autism than the general population and are at higher risk of developing various language and cognitive problems; studies of monozygotic and dizygotic twins have shown an increased concordance for autism in monozygotic twin pairs 20,21. There presently are promising leads on several chromosomes. It appears that multiple genes are likely implicated.
Although considerable interest has centered on the possible role of environmental agents, e.g., heavy metals or MMR immunization, the available evidence is highly limited 9,10. Some work has centered on investigation of potential models of autism based on effects of teratogens, e.g., thalidomide (22).
Diagnosis and Clinical Features
Age of Onset
In most cases, the apparent onset of autism occurs within the first or second year of life. Common presenting concerns include delayed language development, social unrelatedness, or unusual sensitivities to the environment. Although Kanner (4) believed that autism was present from, or shortly after, birth, subsequent work has suggested that the disorder sometimes can be observed after some months, or even a few years, of relatively normal development (23). The study of developmental regression in autism has been complicated by several issues, including variables that complicate
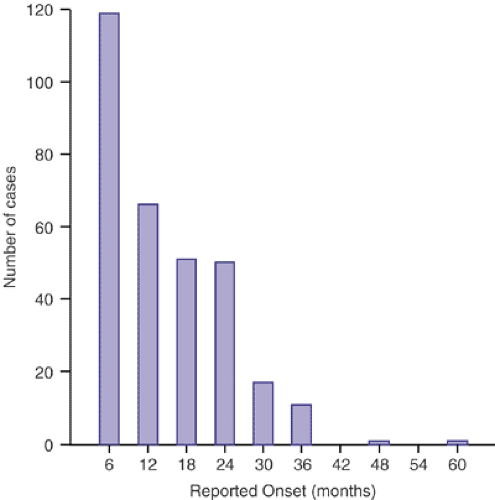
interpretation of parental reporting. About one-fourth of parents of children with autism spectrum disorders report that their child had a few meaningful words and then stopped talking and/or regressed in social abilities (3). The area of early diagnosis is an important topic for research, since good data indicate that for many children outcome improves with early detection. Figure 5.1.1.3 depicts the onset of cases with clinical diagnoses of autism in the DSM-IV field trial.
interpretation of parental reporting. About one-fourth of parents of children with autism spectrum disorders report that their child had a few meaningful words and then stopped talking and/or regressed in social abilities (3). The area of early diagnosis is an important topic for research, since good data indicate that for many children outcome improves with early detection. Figure 5.1.1.3 depicts the onset of cases with clinical diagnoses of autism in the DSM-IV field trial.
Social Disturbance
Autism was initially described by Kanner as a disturbance of affective contact. Social dysfunction in autism is distinctive; it is not explicable in terms of cognitive delay alone and is a, if not the, central defining feature of the disorder (18). Social and adaptive abilities, language level, and nonverbal intelligence are important predictors of independence and long-term prognosis (24). As Kanner emphasized, normally developing infants are remarkably social, even in the first few weeks of life (18). They exhibit an apparent predisposition to form social relationships; this predisposition appears to be an important foundation for the development of other skills. The social development of children with autism is distinctive in many ways. The human face holds little interest for many autistic infants; lack of eye contact, fewer socially directed behaviors such as facial expressions, vocalizations, or pointing, and a lack of interest in other children are typical (18). Early difficulties seen in children with autism include absence or diminution of babbling, failure to respond to their names, and delayed pointing to express interest (not just to request). Deficits in social interaction in autism change somewhat over the course of development but remain an area of great disability even for the highest functioning adults with autism.
Communication
Deficits in the development of expressive language are one of the more frequent sources of initial concern for parents of children later diagnosed with autism. Communication problems appear to be a central aspect of the syndrome. Previous studies have indicated that approximately half the patients with autism never used speech as their primary method of communication, although this number may be decreasing with earlier, more effective intervention (25). Those who do speak exhibit language that is distinctive in several ways, including for use of stereotyped phrases and immediate and delayed echolalia, idiosyncratic language (e.g., saying, “Time for bed, honey” as a request to leave the office), pronoun reversal, lack of usual prosody, impaired semantic development, literalness, and failure to use language for social interaction (26). Immediate echoing (i.e., repeating right back what someone just said) is also observed in normally developing children who are acquiring language and in autism may represent an area that can be used to help build the child’s language. Deficits in pragmatic communication, particularly the ability to have a back-and-forth conversation, are typical. The language and communicative deficits in autism differ from those seen, for example, in the developmentally language-disordered child 25,26.
Cognitive Development
Kanner’s initial impression that children with autism exhibited normal levels of intelligence was based on their intelligent appearance and the observation that they performed quite well on certain parts of traditional tests of intelligence; this proved incorrect and many individuals with autism, probably about half, exhibit some degree of intellectual deficiency (mental retardation). IQ scores are relatively stable and predictive of outcome (27), although it is again important to note that with earlier detection and intervention, rates of associated mental retardation may be decreasing (24). Marked scatter in performance on tests of intelligence is common and differs from the usual pattern observed in nonretarded children with autism. Islets of unusual ability (e.g., rote memory or block design) may be present (28). A few persons with autism exhibit truly remarkable, isolated abilities or “splinter skills,” for example, in musical or drawing talent, or in exceptional feats of memory, such as the ability to name days of the week corresponding to dates several years in advance (“calendar calculators”) (28). In autism, deficits in abstract thinking and in sequencing and processing information are common. Lower levels of intelligence are associated both with a greater risk of developing a seizure disorder in adolescence and with a worse outcome (24). The pattern of verbal and nonverbal (performance) IQ (VIQ and PIQ, respectively) may help differentiate persons with autism (VIQ<PIQ) from those with Asperger’s disorder (VIQ>PIQ) (27).
Cognitive deficits may begin to become apparent in infancy (29), and scatter in developmental examination during the preschool years (30). In general, children with autism do best with tasks that involve motor and perceptual–motor skills and worst with tasks that involve symbolic information and verbal skills (28).
Behavioral Features
The contrast between the response of a child with autism to the inanimate environment (seeing the credits flash by on television) and the lack of response to social cues (the voice of a parent) is often quite striking (30). A child may show relatively little differentiation of his sibling from other children, but be particularly attached to an unusual object, such as a spongy puzzle piece. Although parents may initially be concerned that their child with autism is deaf, often the child is quite sensitive to certain nonspeech sounds (the vacuum cleaner or a jingle on the radio). Interest in nonfunctional aspects of objects (taste or feel) and stereotyped (purposeless and repetitive) movements are common and include hand flapping, toe walking, spinning objects, and the like. These observations are quite consistent with Kanner’s original report, which contrasted the relative lack of social interest with the overconcern with environmental (nonsocial) change. Such activities appear to be preferred modes of behavior and can consume much of the child’s time. Unusual
affective responses are also common; a child may become panicked in response to new situations, such as having to walk across a porch to a door, or by regularly recurring stimuli such as singing in church. Play skills are typically quite deviant, accompanied by deficits in imaginative play. These aspects of the disorder are shared with many children without autism who have severe or profound mental retardation, but they appear to be more common in autism and occur even in affected children who have normal intelligence (3).
affective responses are also common; a child may become panicked in response to new situations, such as having to walk across a porch to a door, or by regularly recurring stimuli such as singing in church. Play skills are typically quite deviant, accompanied by deficits in imaginative play. These aspects of the disorder are shared with many children without autism who have severe or profound mental retardation, but they appear to be more common in autism and occur even in affected children who have normal intelligence (3).
Physical Characteristics, Pathology, and Laboratory Examination
Over the years, a number of potentially causal medical associations have been reported for autism (31). However, on close examination, many such associations appear weak (32). The strongest connection appears to be with epilepsy; about 20% of individuals develop recurrent seizures, with a bimodal pattern of onset with peaks in early childhood and adolescence (33) (Figure 5.1.1.4). There are also higher than expected proportions of individuals with autism and with fragile X syndrome or tuberous sclerosis (9). Other potential associations include other genetic disorders such as phenylketonuria, maternally inherited deletions (Angelman’s syndrome), and duplications of chromosome 15q11–q13 (21). As noted above, overall brain size appears to be increased in autism in toddlerhood, although by adulthood brain size may be only a few percentile fractions larger than normal (15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree