15 Anterior cervical decompression and fusion (ACDF) has demonstrated consistently good outcomes for the management of cervical radiculopathy and myelopathy in the setting of spondylosis.1 Cervical decompression and fusion via an anterior approach facilitates an effective decompression of the spinal canal and neural foramen, and with modern anterior plating, fusion rates are ~95%2,3 for a single-level fusion. It is well recognized that patients undergoing ACDF experience some degree of degeneration at levels adjacent to the fusion.1,4–8 As described by Hilibrand et al,9 this rate is ~3%/year, and at 10 years after ACDF, 25% of patients reported symptoms of adjacent segment disease. It is unresolved if adjacent segment degenerative changes are the natural progression of cervical degenerative disease or if these degenerative changes are potentiated by altered cervical kinematics after a fusion procedure. In large part in an effort to maintain more normal kinematics, cervical disk arthroplasty has been proposed as an alternative to single-level fusion in the appropriately selected patient. The cohort data from the multicenter prospective randomized trials of single-level ACDF and arthroplasty provide an opportunity to directly evaluate the adjacent-level kinematics after each procedure, and any difference (if any) in long-term sequelae. Here we present a review of the literature on adjacent-segment disease, with a focus on levels of clinical evidence. Herkowitz et al10 examined a cohort of patients undergoing either ACDF or posterior laminoforaminotomy for radiculopathy and found significant rates of adjacent-segment degeneration in both populations, but interestingly the patients that underwent posterior laminoforaminotomy had a higher incidence (50 vs 41%). Baba et al5 evaluated a retrospective case series of 106 patients with cervical spondylotic myelopathy that underwent ACDF (42 one-level, 52 two-level, 12 three-level), and found significantly increased motion (flexion-extension) at the interspace cephalad to the fusion. Hilibrand et al9 reported on a consecutive series of 374 patients managed with ACDF for cervical radiculopathy, myelopathy, or myeloradiculopathy and found a rate of adjacent-level disease of ~3%/year, and at 10 years after ACDF, 25% of patients reported symptoms of adjacentsegment disease. Papadopoulos et al11 reported a retrospective case series of 46 patients that underwent three-level ACDF and found that at an average of 17.6 months postoperatively 11/46 patients demonstrated adjacent-level degeneration, five of whom were symptomatic. Similarly, Ishihara et al7 evaluated a cohort of 112 patients that underwent ACDF and found that 19/112 developed symptomatic adjacent-segment disease. Yue et al12 analyzed a cohort of 71 patients with ACDF at an average follow-up of 7.2 years and found that adjacent-level degeneration occurred in 73% of their cohort. Similarly, Clarke et al13 analyzed a cohort of 303 patients that underwent posterior laminoforaminotomy at average follow-up of 7.1 years and found an annual 0.7% rate of adjacent-segment disease and 10-year rate of 6.7%. These findings support the hypothesis that altered bio-mechanics from the fusion are not entirely responsible for adjacent-segment degeneration. To what degree this adjacent-level degeneration occurs as a consequence of the natural progression of cervical spondylosis and to what extent this degeneration may be due to the fusion procedure itself remains somewhat controversial, but the weight of the clinical evidence supports that adjacent-level degeneration occurs at a fairly consistent rate after a fusion procedure. Pearls • There is no level I evidence on the incidence of adjacent-segment degeneration. • Level II and IV evidence indicates that adjacent-segment degeneration occurs after both anterior and posterior cervical procedures. • Segments C5–C6 and C6–C7 appear to be at greatest risk. With fusion and the consequent loss of motion at the index level (s), it is hypothesized that the adjacent levels may experience a compensatory increase in motion. Furthermore, this increased motion may be nonphysiological. Clinical and cadaveric14,15 studies have demonstrated altered motion at spinal segments adjacent to a fusion. Sasso et al16 analyzed the 24-month data from the U.S. Investigational Device Exemption (IDE) trial of the Bryan cervical disk (Medtronic, Memphis, TN) and demonstrated that the arthroplasty level maintained 8 degrees of motion. However, at the adjacent levels there was no significant difference in flexion-extension range of motion between the patients receiving the arthroplasty versus the fusion group. Sasso et al17 reported on their institution’s cohort of 22 patients enrolled in the U.S. IDE trial of the Bryan cervical disk (Medtronic), and noted that in patients undergoing fusion relative to arthroplasty there appeared to be an increased translational component to the motion at adjacent segments, but this was not statistically significant and was not observed in all fusion patients. These results suggest that when analyzing segmental motion one should consider all degrees of freedom, and not just differences in flexion-extension. Robertson et al18 performed a prospective comparative (compared data from two prospective studies) evaluation of patients undergoing Bryan cervical disk arthroplasty (n = 74) or anterior fusion (n = 158) and found a statistically significant increase in adjacent-level radiographic changes in the fusion group (34.5% vs 17.5%), as well as a statistically greater incidence of symptoms related to adjacent-level disease in the fusion cohort. Nabhan et al19 reported 1-year follow-up data for ProdiscC (Synthese, Inc., West Chester, PA) versus ACDF in a randomized cohort of 49 patients (prospective, single-center). Of note, these two cohorts had tantalum markers placed in each vertebra above and below the prosthesis to facilitate accurate radiographic measurements. Over the course of the study there was a progressive decrease in motion in both the arthroplasty and fusion groups at the index level, but this decrease in motion was significantly greater in the fusion group; no analysis of adjacent levels was reported. Goffin et al20 reported intermediate follow-up data for the European Bryan multicenter trial (prospectively collected cohort data, no comparison group). Analysis of adjacent segments was not reported, but of note, of the patients receiving single-level arthroplasty, 12% had motion at the index level of 2 degrees or less, which is indistinguishable from fusion within the error of measurement. Reitman et al21 presented an observational cohort of 21 patients managed with ACDF analyzed utilizing fluoroscopy with algorithms to correct for digital distortion. There were no significant differences in adjacent-level motion after a fusion procedure at a mean follow-up of 13 months.21 In a retrospective case series, Matsunaga et al22 calculated strain distributions in intervertebral disks after ACDF. Strain at segments adjacent to anterior fusion was significantly increased 1 year after surgery in patients that had two- or three-level fusions (no significant changes were observed in patients that underwent single-level fusion); in a subset of the cohort that had direct MRI comparison pre- and postoperatively, increased strain correlated with disk herniation in the postoperative period. In vitro studies do not fall under the classification of levels of evidence for evidence-based practice. However, with respect to analysis of cervical spine biomechanics, select cadaveric studies do offer insight regarding adjacent-segment changes after fusion and are presented here. Eck et al14 demonstrated in a cadaveric model that anterior fusion and plating significantly increased both intradiskal pressure and segmental motion adjacent to the fusion. Similarly, Dmitriev et al23 demonstrated statistically significant increases in intradiskal pressures at the levels adjacent to an anterior fusion. Given the clinical and cadaveric data, there is sufficient evidence to conclude that an anterior fusion procedure may alter the biomechanics of the adjacent levels. However, the cadaveric models referenced did not include the occiput–C1– C2 articulations, and therefore caution should be used in extrapolating results to the clinical situation. The upper cervical spine has significantly more flexibility than C2–T1, and as a result it is possible that in the clinical situation decreased motion secondary to a fusion in the lower cervical spine may be accommodated by motion in the upper cervical spine. When considering the clinical prognosis of adjacent spinal levels after a fusion, it must be recognized that this is a cohort with established spondylitic disease. Patients undergoing ACDF represent a cohort with demonstrated clinically symptomatic cervical spondylosis, and as a group may be more susceptible to degenerative changes at other levels, irrespective of fusion. Degenerative changes at the levels adjacent to ACDF are likely multifactorial. Clearly, this is a patient population with demonstrated cervical pathology, and there may be subclinical disease at adjacent levels that will progress irrespective of treatment modality. The progression of natural disease is supported by studies such as those done by Herkowitz et al10 in which spondylotic patients that underwent posterior procedures (laminoforaminotomies) demonstrated clear adjacent-level progressive degeneration. Similarly, the cadaveric and clinical studies suggest that fusion may subject the adjacent levels to altered motion and increased intradiskal pressures. Although not definitive, Matsunaga et al’s work22 showing that increased adjacent-level strain correlated with postoperative disk herniation is intriguing and supports the thesis that the adjacent-level strain caused by a fusion may accelerate degeneration, particularly if the adjacent level demonstrates early (asymptomatic) degenerative changes at the time of the procedure. Hilibrand et al9 found that the risk of new disease at an adjacent level was significantly lower after a multilevel arthrodesis. One could interpret the findings of Matsunaga and Hilibrand to suggest that an abnormal disk space adjacent to a fusion is at risk for symptomatic degeneration subsequent to the fusion and may be considered for inclusion in the index procedure. The progression of degenerative changes at a level adjacent to a fusion may reflect the effect of altered biomechanics on an interspace that has a degree of underlying pathology. However, the limitation of cadaveric studies and concerns regarding measurement error of flexion-extension measurements in in vivo studies24 suggests that there may be an incomplete understanding of adjacent-level kinematics. Utilizing fluoroscopy with algorithms to correct for digital distortion, Reitman et al found no significant differences in adjacent level motion after a fusion procedure at a mean follow-up of 13 months.21 Reitman et al’s findings would support a hypothesis that adjacent-segment degeneration may be more reflective of progression of underlying spondylosis and not due to adjacent-level increased motion. One hypothesis is that motion lost during a subaxial fusion procedure may be compensated for by the upper cervical spine rather than via increased motion at adjacent levels. The impetus, in large part, for cervical disk arthroplasty is the theory that maintaining motion at the interspace after decompression will eliminate (or decrease) the contribution of the surgical procedure to the progression of adjacent-level disease. If arthroplasty is to mitigate adjacent-level stresses, one would assume that adjacent-level motion would be different in arthroplasty versus fusion cohorts. The historical fusion data suggest a rate of adjacent-segment degeneration that averages around 3% per year, so follow-up periods of longer than 2 years will be needed to ascertain the true outcomes of any prospectively collected cohort. However, the early data from the cervical disk arthroplasty cohorts can provide early indications regarding kinematics, particularly with respect to adjacent-level motion. A component of the hypothesis underlying the prospective comparison trials of cervical disk arthroplasty to ACDF is that disk arthroplasty maintains sufficiently normal motion at the surgical level to preserve normal biomechanics at the adjacent levels. In addition to comparing adjacent-segment radiographic changes, one may also consider rates of new clinical symptoms and rates of reoperation on adjacent segments in both the disk arthroplasty and fusion groups. Mummaneni et al,25 in the report of the 2-year follow-up data for the Prestige IDE trial, found a rate of reoperation of 3.4% in the ACDF cohort compared with 1.1% in the disk arthroplasty cohort. Adjacent-level radiographic changes were not reported. Heller et al,26 in their 2-year follow-up data from their prospective multicenter trial of ACDF (221 patients) and arthroplasty (242 patients), reported smaller differences in the rate of surgery for adjacent-segment disease between arthroplasty and fusion. They found no statistical difference between the groups with respect to the rate of secondary surgical procedures. Motion was maintained at the index level in the arthroplasty group (8 degrees at 2 years); no data were reported regarding motion at levels adjacent to the arthroplasty or fusion. Sasso et al16 reported the outcomes of their prospective multicenter trial of ACDF and arthroplasty, 2-year follow-up data, and found that there was significantly more motion retained with the arthroplasty group than with the fusion group at the index level. However, no detailed analysis of motion at the adjacent segments was presented. Wigfield et al27 compared motion at levels adjacent to either a fusion or a cervical disk arthroplasty (prospective comparative) and found a statistically significant increase in motion at levels adjacent to fusion relative to arthroplasty at 12-month follow-up. Interestingly, the 2-year follow-up data from the U.S. IDE trials of cervical disk arthroplasty have not uniformly demonstrated a significant change in flexion-extension motion in the levels adjacent to the fusion relative to arthroplasty. Rabin et al28 did not find any significant differences in adjacent-level kinematics between fusion and arthroplasty in a matched comparison study. It is interesting to note that in some of the U.S. IDE trials for disk arthroplasty a course of nonsteroidal antiinflamma-tory medication was utilized,26 in part due to the observation in the European trials of ossification at the procedure level with consequent loss of motion.29 Goffin et al20 reported a 12% percent incidence of loss of motion at the arthroplasty level that, in a sense, effectively resulted in fusion (less than 2 degrees of motion). The initial reports of the U.S. IDE data have not demonstrated similar ossification and loss of motion, and it is hypothesized that this is due to the incorporation of nonsteroidal antiinflammatory drugs (NSAIDs) in the postoperative protocol. When considering rates of adjacent-segment degeneration in the setting of anterior fusion compared with arthroplasty, one must also take into consideration the confounding variable of plate positioning and surgical dissection. When placing an anterior plate the screws are placed to engage the cortical bone near the end plate, and surgical dissection consequently may extend closer to the adjacent segment than the dissection for arthroplasty. Inadvertent disruption of Sharpey fibers near the adjacent interspace may consequently be a more common occurrence with anterior plating. The relative size of the anterior plate compared with the interspace has also been shown to affect the adjacent segments. A plate that is within 5 mm of the adjacent level has an increased association of adjacent-level ossification.30,31 Consequently, some radiographic changes adjacent to a fusion may be secondary to plate positioning or surgical dissection and may not necessarily be indicative of biomechanical stresses. Although the decreased rate of reoperation in the arthroplasty cohort may suggest a decreased incidence of symptomatic adjacent-segment disease, the decision to operate on an adjacent segment was made by the surgeons, which introduces potential bias. The Prestige® Cervical Disc (Medtronic Sofamor Danek, Memphis, TN) implant includes a plate and screws placed into the adjacent vertebrae. Revision adjacent to such a structure may be quite challenging, and this may have been an impediment to recommending adjacent-level surgery in the arthroplasty patients in that particular study. It should also be noted that if the surgeons participating in the IDE trials believe that arthroplasty will prevent new disease at adjacent levels, then they may be less likely to “recognize” adjacent-segment disease among their patients undergoing arthroplasty than among those undergoing fusion. When comparing outcomes of the prospective randomized U.S. IDE trials one must be cognizant of the potential for affirmation bias. A significant proportion of patients that elected to participate in the IDE trials declined participation in the study after randomization (e.g., 117 patients declined participation after randomization in the Bryan IDE trial26). Presumably, patients elected to enroll in an IDE trial evaluating disk arthroplasty because they desired to pursue the potential benefits of this technology. Consequently, patients randomized to arthroplasty may have different expectations of outcome than those randomized to fusion, and those randomized to fusion may feel disappointed with their procedure purely on the basis of their randomization—as evidenced by the significant number of patients that elected to remove themselves from the study after randomization to fusion. When a significant portion of subjects decline a study after randomization, the remaining cohorts may no longer be assumed to have equivalent psychometric profiles: a potentially significant confounder when utilizing patient-reported data for outcomes measures. Pearls • Level I, II, and IV evidence demonstrates that cervical arthroplasty maintains motion at the level of the procedure. • There is no consensus (level II and IV evidence) regarding motion at levels adjacent to arthroplasty or fusion.
Avoidance of Cervical Adjacent Segment Disease
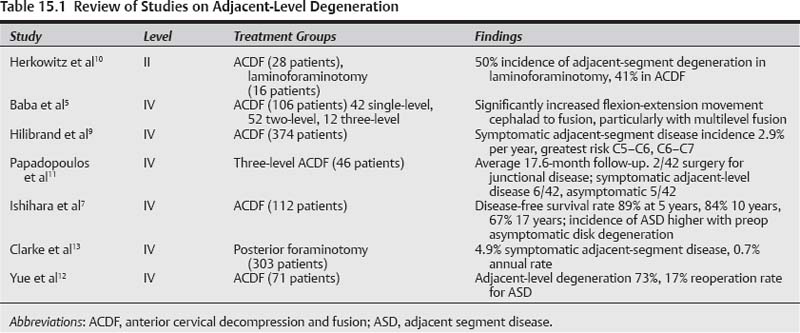
 Adjacent-Level Degeneration (Table 15.1)
Adjacent-Level Degeneration (Table 15.1)
Level II
Level IV
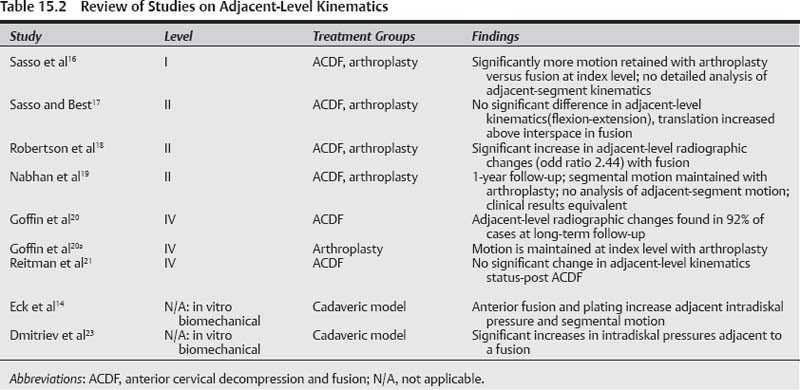
 Adjacent-Level Kinematics (Table 15.2)
Adjacent-Level Kinematics (Table 15.2)
Level I Data
Level II Data
Level IV Data
In Vitro Studies
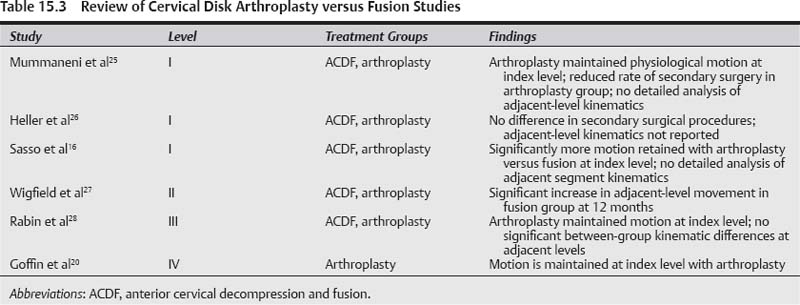
 Cervical Disk Arthroplasty versus Fusion (Table 15.3)
Cervical Disk Arthroplasty versus Fusion (Table 15.3)
Level I Evidence
Level II Evidence
Level III Evidence
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree