Figure 7.1
Burr hole. (a) Power drill being used to make burr hole. (b) Completed burr hole with dura mater at the base
Procedure
Burr holes are most commonly placed at the bedside in the intensive care unit. After the patient is properly intubated for general anesthesia, sedated, and the head placed in a neutral position, a point 10 cm posterior to the nasion, which represents the intersection of the frontal bone and the two nasal bones, and 3 cm lateral to the midline, usually at the mid-pupillary line, is marked (Fig. 7.2). This is known as Kocker’s point. A 2 cm area centered on this point is shaved, prepped and draped in sterile fashion. A linear incision is made in the scalp down to the skull. A hand-held twist drill is used to place a hole through the skull. The dura is opened sharply with a scalpel. For intracranial pressure, a ventricular catheter is then passed perpendicular to the skull down and aiming towards the ipsilateral medial canthus and mastoid process towards the ventricular space, which is a fluid filled space within the brain parenchyma, to a depth of 6.5 cm from the outer table of the skull (Fig. 7.3). The drain is used to measure intracranial pressure and to drain cerebrospinal fluid (CSF) to control pressure as needed. The catheter is then tunneled under the scalp, brought out from another puncture site, secured with multiple stitches, and sterilely connected to a drainage system [2–4] (Fig. 7.4).
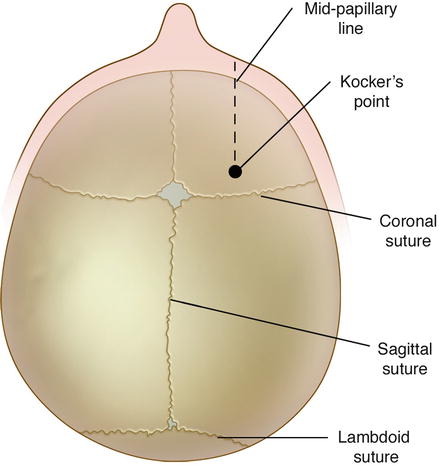
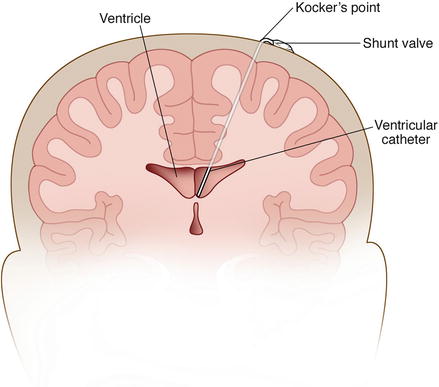
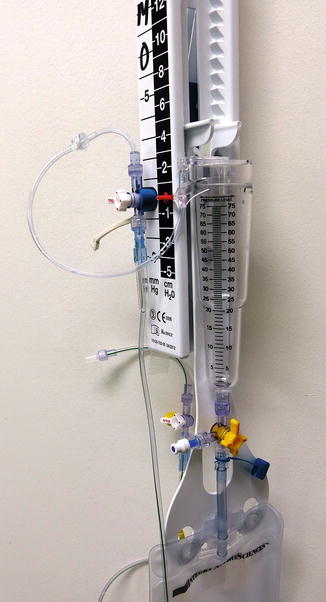
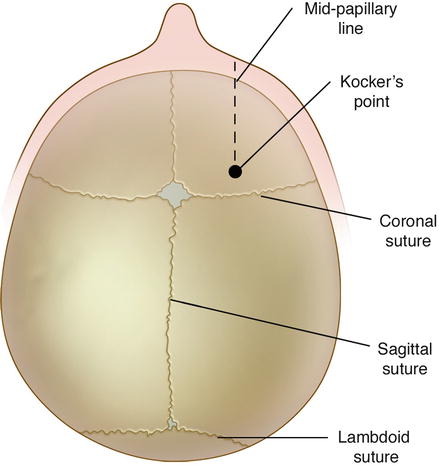
Figure 7.2
View of the skull from the top with bony landmarks
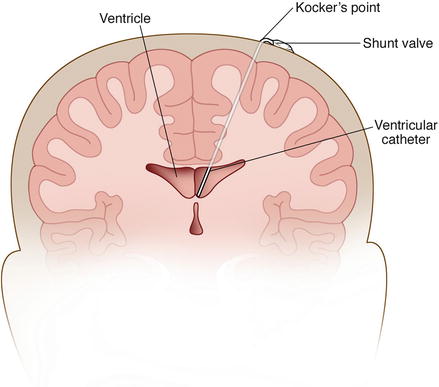
Figure 7.3
Ventricular catheter placed through the Kocker’s point
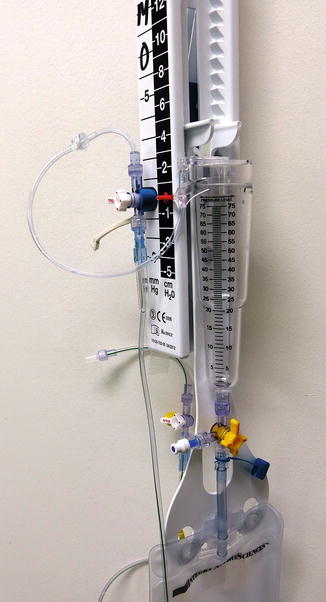
Figure 7.4
Sterile drainage system which connects to the ventricular catheter
Craniotomy
A craniotomy is a surgical procedure that requires removal of a bone flap to access the brain. Several common indications that require a craniotomy include removal of brain tumors, evacuation of intracranial hemorrhages, epidural and subdural hematomas, treatment of central pain syndromes (trigeminal neuralgia, hemifacial spasm), clipping of aneurysms, and removal of vascular malformations (arteriovenous malformations). Bone flaps can be removed from various parts of the skull and are dictated by the location of the pathology within the brain and skull. The names given to craniotomies include bifrontal, frontal, pterional, temporal, parietal, occipital, suboccipital, and far lateral, based on the location [3, 5].
Procedure
The patient is intubated and sedated under general anesthesia. A head clamp, commonly a frame with three points of fixation, is used to position the patient’s head in a rigid position. The patient is positioned appropriately for the craniotomy which is dictated by the side and location of pathology. Often, computerized image guidance systems are used to specifically locate the lesion and plan the incision. Then, an incision is made in the scalp down to the bone, the pericranium is reflected, and a perforator drill is used to make burr holes in the skull. These holes are then connected with a specialized drill bit, and the bone flap is removed (Fig. 7.5). The dura is then incised sharply and reflected off the brain. The pathologic lesion is then removed, and the dura is closed over the brain primarily with suture material. If the dura cannot be closed primarily, grafts are sutured into the dura. The bone is then replaced with titanium plates in adults (Fig. 7.6) and sutures in young children. Finally, the scalp is closed over the bone [2–5].