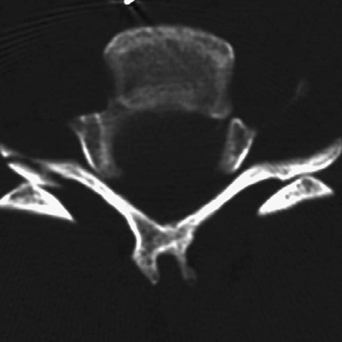
5 A 51-year-old woman was assaulted during a bar fight and became a C5 quadriplegic. Axial CT through the area of injury demonstrates inversion of the normal appearance of the facets-“naked facets” (Fig. 5-1). The C5 inferior facet is located anterior to the C6 superior facet, indicating bilaterally jumped and locked facets. This also indicates an anterolisthesis of 50% or greater. FIGURE 5-1 Axial computed tomography (CT) showing the “reversal hamburger” sign. The orientation of the facets is reversed because C5 is anterolisthesed on C6. FIGURE 5-2 Postoperative lateral C-spine x-ray displaying a 360-degree fusion construct from the patient in Fig. 5-1. FIGURE 5-3 Preoperative spondyloptosis. Traumatic spondylolisthesis with cervical cord injury A 360-degree fusion was done (Fig. 5-2). Bilaterally dislocated facets are a grossly unstable cervical spine injury resulting from severe trauma to the spine. This is a three-column injury. The anterior longitudinal ligament, posterior longitudinal ligament, disc annulus, facet capsules, and interspinous ligaments are all disrupted. These patients commonly present with significant neurologic deficit. A more extreme form of this type of injury is cervical spondyloptosis, which is pictured preoperatively in Fig. 5-3and postoperatively in Fig. 5-4. These patients are quadriplegic, and by definition the upper segment is 100% subluxed in relation to the lower segment. Complete spine precautions must be practiced, and hypoxia and hypotension should be avoided. The rest of the spine should also be evaluated for concomitant injury, especially in these cases. Multisystem trauma can result from the degree of force responsible for this type of injury and must be carefully sought out. Methylprednisolone spinal cord injury protocol should be started if the patient presented within 8 hours of injury. After an emergency magnetic resonance imaging (MRI), if there is no acute disc compressing the cord, closed reduction can be attempted through careful coaxial traction. Because the patient will require operative fixation, open reduction can be achieved surgically, but this takes away the advantage of an immediate postreduction examination. If a compressive disc herniation is identified on MRI, emergency surgery for decompression and stabilization is done. This may require an anterior discectomy, posterior fusion, and then anterior fusion. Alternatively, it may require only an anterior discectomy and fusion, followed by a posterior fusion if reduction has been achieved. Drilling the facets posteriorly and realigning the spine after the anterior discectomy help in posterior reduction. All maneuvering of these patients needs to be done with the utmost care, as all manipulation carries the risk of greater damage to the cord. If reduction is done while the patient is under anesthesia, it is prudent to have neurophysiologic monitoring.
Bilateral Locked Facets
Presentation
Radiologic Findings


Diagnosis
Treatment
Discussion

Bilateral Locked Facets
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








