CHAPTER 7 Bipolar and related disorders
Bipolar mood disorders (BD) are characterised by the occurrence of elevated mood and (usually) depressed mood, either at different times or simultaneously (see Table 7.1 and Box 7.1). The precise delineation between ‘normal’ mood swings, mood instability as part of a personality disorder, and mood swings which are an indicator of bipolar disorder, is complex. As in all mood disorders, the disruption of normal mood is not the only or even necessarily the most prominent element of the disorder.
TABLE 7.1 Features of bipolar affective disorder according to DSM–IVTR and ICD–10
BOX 7.1 Core elements of bipolar disorder
Clinical features
Mania
Mania is a mental state in which motivation, energy, mood and/or thinking are elevated. The need for sleep is reduced, thought content is more grandiose, speed of thinking is increased, but thoughts remain connected (‘flight of ideas’), distractibility is high, libido is increased, behaviour is more socially disinhibited (including excessive spending of money), judgment is impaired and often the person is more physically active than usual. The person is often intolerant of challenge and may become aggressive if frustrated. This can pose a major problem for ‘significant others’ when faced with very inappropriate behaviour.
Depressed phase of bipolar disorder
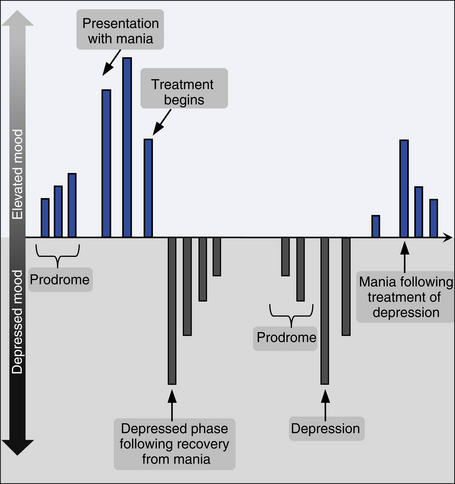
The clinical presentation is essentially the same as in depressive disorders (see Ch 6), but is more likely to be severe, and associated somatic (melancholic) features are more likely. Abrupt onset of a severe melancholic depression in a young person (particularly an adolescent) may be a harbinger of bipolar disorder, and careful monitoring of antidepressant response (to check for manic switch) is required. ‘Atypical’ depressive clinical features are more common in bipolar disorders than other mood disorders. The different phases of illness are shown in Figure 7.1.
Course of bipolar disorders
In bipolar I disorder, episodes of both mania and severe depression occur. Bipolar II disorder is characterised by episodes of hypomania, interspersed by separate and often severe episodes of depression. Rapid cycling bipolar disorder refers to a subset of patients with either bipolar I or bipolar II disorder whose illness includes more than four episodes of both mania/hypomania and depression per year. This form of the illness is particularly disruptive and may be provoked by substances such as antidepressant medications and stimulants.
Depressive episodes are the most common state in bipolar disorders, but a very small group of people will suffer only manic symptoms. The most common sequence is for mania and/or hypomania to be followed by depression, but the reverse also occurs. Depression followed by mania or hypomania is often more resistant to mood stabilisers than the opposite sequence. Manic symptoms become less common with age in bipolar individuals and mixed manic and depressive symptoms more common. Figure 7.2 is a pictorial representation of a patient with bipolar I.
Mixed bipolar states
Manic or hypomanic symptoms may arise simultaneously with depressive symptoms in a mixture which is easily overlooked. Sometimes, manic and depressive symptoms will arise in close succession and at other times symptoms of mania or hypomania may be present and combined with depressed mood or negative thought content. The affect is often irritable rather than euphoric.
Schizoaffective disorder
When an individual has presented with clear features of schizophrenia (see Ch 5) and at other times clear features of mania, a diagnosis of schizoaffective disorder can be considered. This is a controversial concept and illustrates the limitations of our current diagnostic system.