Author (reference no.) |
Year |
Extract/Formulation/Dosage |
Study Length |
N |
Outcome Measure/Result |
Study Design |
|---|
Kesselkaul (105) |
1957 |
Remifemin 60 drops |
2 wk |
63 |
Alleviation of climacteric complaints in 95% of patients |
Case series |
Schotten (106) |
1958 |
Remifemin 20 drops |
3 to 4 wk |
22 |
Alleviation of neurovegetative and psychic complaints associated with menopause and premenopause |
Case series |
Foldes (50) |
1959 |
Remifemin, 3 tablets per day |
Unknown |
41 |
31 patients of the verum group responded to the treatment with a decrease in menopausal complaints. |
Placebo-controlled, open, crossover, patient self-assessment |
Starfinger (107) |
1960 |
Remifemin, 3 to 20 drops per day |
1 yr |
105 |
Decreased climacteric complaints without incidence of side effects or resulting in nonphysiologic bleeding. |
Case series |
Brucker (108) |
1960 |
Remifemin, tablets, variable dose |
Variable |
87 (517) |
Alleviation of menopausal complaints |
Case series |
Heizer (109) |
1960 |
Remifemin, 3 to 6 tablets per day |
2 to 18 mo |
66 |
Alleviation of menopausal (neurovegetative and psychic) complaints in 47% of patients with intact uteri and 35% with hysterectomies |
Case series |
Gorlich (110) |
1962 |
Remifemin, tablets, variable dose |
Variable |
41 (258) |
Alleviation of climacteric and vascular symptoms in 85% of patients |
Case series |
Schildge (111) |
1964 |
Remifemin, fluid extract 60 drops per day |
Variable |
135 |
Euphoric and mild sedative-calming effects in all pts |
Case series |
Stolze (112) |
1982 |
Remifemin, fluid extract 80 drops per day |
6 to 8 wk |
629 |
Alleviation of neurovegetative and psychologic menopausal symptoms in 80% of patients |
Open, physician and patient self-assessment |
Daiber (113) |
1983 |
Remifemin, fluid extract 80 drops per day |
12 wk |
36 |
Alleviation of climacteric complaints (hot flashes, insomnia, sweating and restlessness) |
Open, KMI, CGI |
Vorberg (114) |
1984 |
Remifemin, fluid extract 80 drops per day |
12 wk |
50 |
Significant or highly significant alleviation of menopausal (neurovegetative and psychic) complaints, study included subjects contraindicated to hormone therapy. |
Randomized, open, KMI, CGI, POMS |
Warnecke (115) |
1985 |
Remifemin, fluid extract 80 drops per day |
12 wk |
20 |
Significant alleviation of symptoms (psychic and neurovegetative) in the black cohosh, conjugated estrogen anddiazepamgroups. Vaginal cytology of treatment group was comparable to estrogenic stimulation. |
Randomized, open, KMI, HAMA, SDS, CGI, Karyopyknosis index, Eosinophil index. |
Stoll (116) |
1987 |
Remifemin, tablets equiv. to 8 mg extract per day |
12 wk |
26 |
Significant alleviation of climacteric symptoms (vaginal atrophy, neurovegetative, and psychic complaints) in comparison with estrogen and placebo groups |
Double-blinded, randomized, placebo-controlled, KMI, HAMA, VMI (vaginal epithelium) |
Petho (117) |
1987 |
Remifemin, tablets, unspecified dose |
6 mo |
50 |
KMI decreased significantly from 17.6 to 9.2, correlates with a significant reduction in neurovegetative symptoms. Severity of subjective self-assessments of subjects physical and psychologic symptoms decreased. |
Open, KMI, patient self-assessment |
Lehman-Willenbrock and Riedel (118) |
1988 |
Remifemin, tablets equiv. to 8 mg extract per day |
6 mo |
15 |
Significant alleviation of climacteric symptoms in black cohosh and drug treatment groups. No significant change in gonadotropin (FSH, LH) levels. |
Randomized, open, KMI |
Düker et al. (70) |
1991 |
Remifemin, tablets equiv. to 40 mg dried herb per day |
2 mo |
110 |
LH suppression |
In vitro study using blood from menopausal women taking black cohosh |
Baier-Jagodinski (119) |
1995 |
Cimisan T Tropfen, variable dose |
4 to 8 wk |
157 |
89% of patients showed symptom improvement after 4 wk. At final visit, the efficacy was assessed as follows: very good, 40%; good, 41%; sufficient, 12%; inadequate, 7% |
Open, uncontrolled |
Mielnik (66) |
1997 |
Uncharacterized extract, 4 mg per day |
6 mo |
34 |
Alleviation of climacteric (neurovegetative) symptoms in 76% of patients after 1 mo |
Open, KMI |
Georgiev and Iordanova (67) |
1997 |
Uncharacterized extract, unspecified dose |
3 mo |
50 |
Alleviation of climacteric symptoms in 90%. of patients. Increase in vaginal cell proliferation (VMI) in 40% of treated women |
Open, KMI, HAMA, VMI |
Nesselhut and Liske (120) |
1999 |
Remifemin, tablets equiv. to 136 mg dried herb per day |
3 mo |
28 |
Good to very good alleviation of 10 menopausal symptoms in 80% of study participants. |
Open, postmarket surveillance |
Jacobson et al. (59) |
2001 |
Remifemin, tablets equiv. to 40 mg dried herb per day |
60 d |
42a |
No change in median number or intensity of hot flashes |
Double-blinded, randomized, placebo-controlled, patient self-assessment, VAS, MSS |
Liske et al. (65) |
2002 |
Unique C. racemosa preparation, equiv. to 39 or 127.3 mg per day |
6 mo |
152 |
No direct systemic estrogenic effect on serum levels of FSH, LH, SHBG, prolactin, and and 17-β-estradiol. No change in vaginal cytology. Higher dose had a more significant reduction in KM index after 6 mo. Significant reduction with both doses in neurovegatative and psychic complaints. |
Drug equivalence trial, KMI, SDS, CGI |
Hernandez-Munoz and Pluchino (63) |
2003 |
BNO 1055 |
12 mo |
136 |
Combination therapy with tamoxifen (20 mg) reduced severity and incidence of hot flashes. |
Open, randomized, patient self-assessment |
Wuttke et al. (58) |
2003 |
Klimadynon/BNO1055 |
3 mo |
62 |
Equipotent to 0.6 CE for relief of climacteric complaints and for bone resorption. No effect on endometrial thickness. |
Randomized, double-blinded, placebo-controlled, multicenter, MRS |
Verhoeven et al. (121) |
2005 |
125 mg soy extract per day (providing 50 mg isoflavones including 24 mg genistein and 21.5 mg daidzein), 1,500 mg evening primrose oil extract (providing 150 mg gamma linoleic acid), 100 mg A. racemosa L. extract (providing 8mg deoxyacetein), 200mg calcium, 1.25 mg vitamin D, and 10 IU vitamin E, placebo group received 2,000 mg olive oil per day. |
12 wk |
124 |
Subjects were experiencing at least five vasomotor symptoms every 24 h at study entry. At wk 6 and 12, all scores in both groups had improved compared with baseline, though the overall difference in scores between the groups was not statistically significant. |
Multicenter, randomized, placebo-controlled, double-blind study, Kupperman Index and Greene Climacteric Scales |
Nappi et al. (122) |
2005 |
Aqueous isopropanolic extract 40 mg per day |
3 mo |
64 |
Postmenopausal women were recruited. Both CR and low-dose TTSE2 significantly reduced the number of hot flushes per day (P<0.001) and vasomotor symptoms (P<0.001), starting at the first month of treatment. Such a positive effect was maintained throughout the 3 mo of observation, without any significant difference between the two treatments. An identical effect was evident also for both anxiety (P<0.001) and depression (P<0.001) which were significantly reduced following 3 mo of both CR and low-dose TTSE2. Total cholesterol was unchanged by CR treatment but significantly (P<0.033) reduced by 3 mo of low-dose TTSE2. A slight but significant increase of HDL-cholesterol (P<0.04) was found only in women treated with CR, while LDL-cholesterol levels were significantly lowered by 3 mo of both CR (P<0.003) and low dose TTSE2 (P<0.002). Triglycerides were not affected by both treatments, nor was liver function. FSH, LH, and cortisol were not significantly affected after the 3-mo treatment, while PRL (P<0.005) and 17-β-E2 (P<0.001) were increased slightly only by low-dose TTSE2. Endometrial thickness was not affected by either CR or low-dose TTSE2. |
Randomized, controlled clinical study |
Frei-Kleiner et al. (123) |
2005 |
6.5 mg dry rhizome extract; 60% ethanol extraction solvent; dose = 1 cap per day |
12 wk |
122 |
Menopausal women were recruited. The primary efficacy analysis showed no superiority of the tested black cohosh extract compared to placebo. However, in the subgroup of patients with a Kupperman Index ≥20 a significant superiority regarding this index could be demonstrated (P<0.018). A decrease of 47% and 21% was observed in the black cohosh and placebo groups, respectively. The weekly weighted scores of hot flashes (P<0.052) and the Menopause Rating Scale (P<0.009) showed similar results. Prevalence and intensity of the adverse events did not differ in the two treatment groups. |
Multicenter, randomized, placebo-controlled, double-blind, parallel group study |
Pockaj et al. (61) |
2006 |
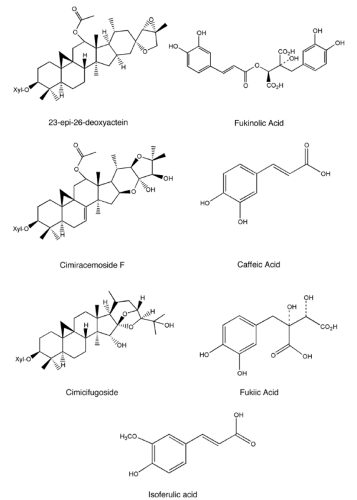
20 mg C. racemosa and rhizome extract standardized to contain 1 mg of triterpene glycosides as calculated by 27-deoxyacetin placebo |
Two 4-wk crossover treatment periods |
132 |
Toxicity was minimal and not different by treatment group. Patients receiving black cohosh reported a mean decrease in hot flash score of 20% (comparing the fourth treatment week to the baselineweek) compared with a 27% decrease for patients on placebo (P=0.53). Mean hot flash frequency was reduced 17% on black cohosh and 26% on placebo (P=0.36). Patient treatment preferences were measured after completion of both treatment periods by ascertaining which treatment period, if any, the patient preferred. Thirty-four percent of patients preferred the black cohosh treatment, 38% preferred the placebo, and 28% did not prefer either treatment. |
Double-blind, randomized, crossover clinical trial. Primary end point was the average intrapatient hot flash score (a construct of average daily hot flash severity and frequency) difference between the baseline week and the last study week of the first treatment
Climacteric Scale |
Newton et al. (HALT) (62) |
2006 |
(a) Black cohosh, 160 mg per day; (b) multibotanical with black cohosh, 200 mg per day, and nine other ingredients; (c) multibotanical plus dietary soy counseling; (d) conjugated equine estrogen, 0.625 mg per day, with or without medroxyprogesterone acetate, 2.5 mg per day; or (e) placebo. |
1 yr |
351 |
Women aged 45 to 55 years with two or more vasomotor symptoms per day were recruited. Vasomotor symptoms per day, symptom intensity, Wiklund Vasomotor Symptom Subscale score did not differ between the herbal interventions and placebo at 3, 6, or 12 mo or for the average over all the follow-up time points (P>0.05 for all comparisons) with one exception: at 12 months, symptom intensity was significantly worse with the multibotanical plus soy intervention than with placebo (P> 0.016). The difference in vasomotor symptoms per day between placebo and any of the herbal treatments at any time point was less than 1 symptom per day; for the average overall the follow-up time points, the difference was less than 0.55 symptom per day. The difference for hormone therapy vs. placebo was −4.06 vasomotor symptoms per day for the average over all the follow-up time points (95% CI, −5.93 to −2.19 symptoms per day; P>0.001). Differences between treatment groups smaller than 1.5 vasomotor symptoms per day cannot be ruled out. Black cohosh containing therapies had no demonstrable effects on lipids, glucose, insulin, or fibrinogen [Spangler et al. (124)]. |
Randomized, double-blind, placebo-controlled trial. Wiklund Vasomotor Symptom scale |
Raus et al. (125) |
2006 |
Dried aqueous/ethanolic (58% v/v) extract CR BNO 1055 of the rhizome of Actaea or CR (black cohosh) |
1 yr |
400 |
Postmenopausal women with symptoms related to estrogen deficiency were recruited. The lack of endometrial proliferation and improvement of climacteric complaints as well as only a few gynecologic organ-related adverse events are reported for the first time after a treatment period of 1 yr. |
Prospective, open-label, multinational, multicenter study; endovaginal ultrasonography |
Sammartino et al. (126) |
2006 |
group A (N=40) was treated with 1 tablet per day per os containing a combination of isoflavones [soy germ extracts, Glycine max, no-OGM SoyLife: 150 mg, titrated in isoflavones (40%) = 60 mg], lignans [flaxseed extracts, Linum usitatissimum, no-OGM LinumLife: 100 mg, titrated in lignans (20%) = 20 mg] and C. racemosa [50 mg, titrated in triterpene (2.5%) = 1.25 mg] (Euclim1; Alfa Wassermann, Italy); group B (N=40) was treated with calcium supplements (Metocal, Rottapharm, Monza, Italy). |
Three cycles of 28 days |
80 |
Healthy postmenopausal women were recruited. At baseline no significant difference was detected in KI between groups A and B; however, after three cycles of treatment, KI was significantly (P>0.05) lower in group A compared with baseline and with group B. |
Double-blind, randomized, placebo-controlled trial, Kupperman Index |
Gurley et al. (127) |
2006 |
Milk thistle (300 mg, three times daily, standardized to contain 80% silymarin), black cohosh extract (20 mg, twice daily, standardized to 2.5% triterpene glycosides), rifampin (300 mg, twice daily), and clarithromycin (500 mg, twice daily) |
14 d |
16 |
Young adults (8 females) (age, mean ± SD = 26 ± 5 years; weight, 75 ± 13 kg) compared with the effects of rifampin and clarithromycin, the botanical supplements milk thistle and black cohosh produced no significant changes in the disposition of digoxin, a clinically recognized P-gp substrate with a narrow therapeutic index. Accordingly, these two supplements appear to pose no clinically significant risk for P-gp-mediated herb-drug interactions. |
Randomized controlled, clinical pharmacokinetic trial |
Rebbeck et al. (128) |
2007 |
Varied |
Case-control design |
949 breast cancer cases; 1,524 controls. |
HRS varied significantly by race, with African American women being more likely than European American women to use any herbal preparation (19.2% vs. 14.7%, P>0.003) as well as specific preparations including black cohosh (5.4% vs. 2.0%, P>0.003), ginseng (12.5% vs. 7.9%, P<0.001) and red clover (4.7% vs. 0.6%, P<0.001). Use of black cohosh had a significant breast cancer protective effect (adjusted odds ratio 0.39, 95% CI: 0.22 to 0.70). This association was similar among women who reported use of either black cohosh or Remifemin (an herbal preparation derived from black cohosh; adjusted odds ratio 0.47, 95% CI: 0.27 to 0.82). |
Population-based case-control study |
Hirschberg et al. (129) |
2007 |
Remifemin (batch no. 229690), one tablet twice daily. Each tablet contains 0.018 to 0.026 mL liquid extract of black cohosh rootstock (0.78 to 1.14:1), corresponding to 20 mg herbal drug (i.e., 2.5 mg dry extract, extraction agent isopropanol 40% [v/v]); 40 mg per day |
6 mo |
74 |
None of the women showed any increase in mammographic breast density. Furthermore, thermore, there was no increase in breast cell proliferation. The mean change ± SD in proportion of Ki-67-positive cells was 0.5% ± 2.4% (median, 0.0; 95% CI = −1.32 to 0.34) for paired samples. The mean change in endometrial thickness ± SD was 0.0 ± 0.9 mm (median, 0.0). A modest number of adverse events were possibly related to treatment, but none of these were serious. Laboratory findings and vital signs were normal. |
Prospective, open, uncontrolled drug safety study |
Chung et al. (68) |
2007 |
Gynoplus (264 mg tablet with 0.0364 mL C. racemosa rhizome, equiv. to 1 mg terpene glycosides; 84 mg dried Hypericum perforatum extract, equiv. to 0.25 mg hypericin, with 80% methanol) |
12 wk |
89 |
Kupperman Index (KI) for climacteric complaints. Vaginal maturation indices, serum estradiol, FSH, LH, total cholesterol, HDL-cholesterol, LDL-cholesterol, and triglyceride levels. Significant improvements in climacteric symptoms and hot flashes, as well as an increase in HDL (from 58.32 ± 11.64 to 59.74 ± 10.54) were observed in the Gynoplus group by 4 wk and maintained after 12 wk, compared to the placebo group. There was no significant impact on superficial cell proportion. |
Randomized, double-blind, placebo-controlled trial. |
Ruhlen et al. (21) |
2007 |
Remifemin R and CimiPure (2.5% triterpenes; 40 mg capsule contains 1 mg 23-epi-26-deoxyactein) |
12 wk followed by 12-wk washout |
61 |
Subjects experienced relief of menopausal symptoms, with reversion to baseline after washout. No effect on serum estrogenic markers. No effect on pS2 or cell morphology in nipple aspirate. |
Open study |
Gurley et al. (130) |
2008 |
Milk thistle (300 mg, three times daily, standardized to contain 80% silymarin), black cohosh extract (40 mg, twice daily, standardized to 2.5% triterpene glycosides), rifampin (300 mg, twice daily), and clarithromycin (500 mg, twice daily). |
14 d |
19 |
Young adults (9 women; age [mean ± SD] = 28 ± 6 years; weight = 76.5 ± 16.4 kg) Milk thistle and black cohosh appear to have no clinically relevant effect on CYP3A activity in vivo. Neither spontaneous reports from study participants nor their responses to questions asked by study nurses regarding supplement/medication usage revealed any serious adverse events. |
Randomized controlled, clinical pharmacokinetic trial |
a All with breast cancer history.
Abbreviations: CGI, Clinician’s Global Impression scale; HAMA, Hamilton Anxiety scale; KMI, Kupperman Menopausal Index; VMI, Vaginal Maturity Index; SDS, Self-Assessment Depression scale; POMS, Profile of Mood States scale; MSS, unspecified menopausal index using the Likert scale; VAS, Visual Analog Scale; Open, open-labeled. (Adapted from Fabricant DS, Farnsworth NR, Black Cohosh (Cimicifuga racemosa). In: Coates P, Blackman MR, Cragg G, Levine M, Moss J, White J, eds. Encyclopedia of Dietary Supplements. New York, NY: Marcel Dekker, Inc.; 2005; pp.41-54.) |