Chapter 19 Brain Tumors, Metastatic Cancer, and Paraneoplastic Syndromes
Varieties
Primary Brain Tumors
Primary brain tumors arise within the brain or spinal cord tissue (parenchyma) or their coverings (meninges) (Box 19-1). Pathologists have named them after their original cell line. The numerous, mostly small, glial cells, which normally provide the structural, biochemical, and immunologic support for the central nervous system (CNS), give rise to most tumors – gliomas. These tumors arise within the substance of the brain, i.e., in intraparenchymal or intra-axial locations. Meningeal cells give rise to the other large category of brain tumors, meningiomas. Because these tumors arise from the coverings of the CNS, rather than from actual brain or spinal cord tissue, they grow outside the brain, i.e., in extraparenchymal (extra-axial) locations. In contrast, CNS neurons rarely form tumors in adults.
Of the various potential etiologies of primary brain tumors, studies have established that only ionizing radiation, certain neurocutaneous disorders (see Chapter 13), and various genetic mutations constitute risk factors. So far, data have not proven that cellphone use constitutes a risk factor.
Gliomas
Parenchymal tumors, gliomas, include oligodendrogliomas and astrocytomas. Oligodendrocytes, which normally produce the myelin covering that insulates CNS neurons,* may give rise to oligodendrogliomas. These tumors, which occur infrequently and grow slowly, produce similar manifestations to the more commonly occurring astrocytomas (see later).
Glioblastomas, the most malignant variety of astrocytoma, are the most frequently occurring brain tumor. They develop almost exclusively in the cerebrum. The prognosis is grim. These tumors not only grow rapidly and relentlessly, they infiltrate widely. Frontal lobe gliomas frequently cross the corpus callosum to produce the infamous “butterfly glioma” (Figs 19-1, A, 20-8, and 20-20). Contrary to many physicians’ expectations that brain tumors, like most other cancers, arise in the elderly, the age of patients at the time of a glioblastoma diagnosis averages only 54 years.
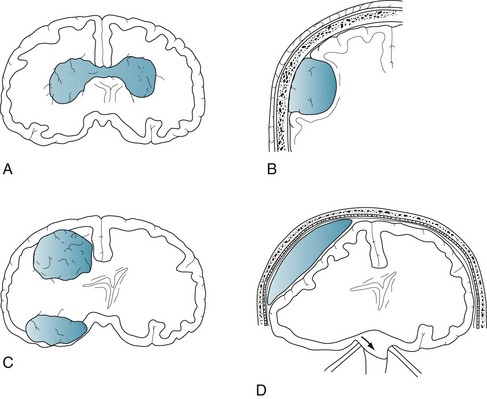
FIGURE 19-1 A, A glioblastoma – the most malignant form of glioma – typically infiltrates along white-matter tracts. Sometimes it spreads through the heavily myelinated corpus callosum in a “butterfly” pattern (see Figs 20-8 and 20-20). B, Meningiomas arise from the meninges overlying the brain or spinal cord and grow slowly (see Fig. 20-10). They compress and irritate, but do not infiltrate, the central nervous system. C, Metastatic tumors, usually multiple and surrounded by edema, destroy large areas of brain and raise intracranial pressure (see Fig. 20-8). D, A subdural hematoma, typically located over one cerebral hemisphere (see Fig. 20-9), compresses the underlying brain and ventricles, and pushes away (shifts) midline structures. Large, acute, rapidly expanding subdural hematomas force the brainstem and ipsilateral oculomotor (third cranial) nerve through the tentorial notch. Such transtentorial herniation, which occurs with epidural as well as subdural hematomas (see Chapter 22), constitutes an immediately life-threatening condition. In contrast, small meningiomas and chronic subdural hematomas cause relatively few symptoms because they are extra-axial and exert little mass effect.
Meningiomas
Arising independently or as an integral part of neurofibromatosis type 1 (see Chapter 13), meningiomas usually create symptoms by compressing the underlying brain or spinal cord (see Figs 19-1, B and 20-10). They grow slowly and predominantly in middle-aged women. Because their expansion is insidious, meningiomas often grow quite large before they produce symptoms.
Primary Cerebral Lymphoma
On CT and MRI, primary cerebral lymphoma resembles cerebral toxoplasmosis (see Figs 20-11 and 20-21). The clinical features of cerebral toxoplasmosis, including focal neurologic deficits and seizures, overlap those of cerebral lymphoma. Although surgery cannot remove lymphomas, steroids often produce dramatic, although temporary, remissions.
Metastatic Tumors
Systemic tumors metastasize to the brain and spinal cord by hematogenous routes. They cannot spread through a lymphatic system because the brain, unlike almost all other organs, does not have one. Metastatic tumors tend to be multiple, surrounded by edema, and rapidly growing. Although individual tumors may each be small, their combined mass constitutes an oppressive intracerebral burden (see Figs 19-1, C and 20-8).
Initial Symptoms
Local Signs
By damaging surrounding tissue, brain tumors usually produce lateralized neurologic deficits, often called “local signs,” such as hemiparesis and dominant- or nondominant-hemisphere neuropsychologic disorders (see Chapter 8). Tumors arising in “eloquent” regions – cerebral cortex areas critical to motor or neuropsychologic function, such as Broca’s or Wernicke’s areas – produce obvious impairments. Tumors that are small, slowly growing, or located in “silent” regions of the brain, such as the right frontal lobe or either of the anterior temporal lobes, notoriously fail to produce symptoms. Tumors that arise from cranial nerves, although rare, almost immediately result in readily recognizable deficits. For example, optic nerve gliomas cause visual loss, and acoustic neuromas cause unilateral progressive hearing loss and tinnitus (see later).
Seizures in individuals older than 60 years are frequently the presenting feature of cerebral tumors. However, because strokes cause seizures nearly as often as tumors, a 60-year-old individual presenting with the first seizure is approximately equally likely to have sustained a stroke as have developed a brain tumor. When the etiology is either a brain tumor or stroke, seizures typically begin as a partial seizure that undergoes secondary generalization (see Chapter 10).
A brain tumor’s tendency to cause seizures also pertains to electroconvulsive therapy (ECT). For example, if a patient harboring a brain tumor were to undergo ECT, the procedure might give rise to multiple, uninterrupted, life-threatening seizures (status epilepticus). However, the benefits of ECT might outweigh the risks if the tumor were small enough not to cause neurologic deficits or surrounding cerebral edema. Large brain tumors, on the other hand, constitute an unequivocal problem regarding ECT. Not only might large brain tumors account for depressive symptoms, but also they might precipitate transtentorial herniation during ECT (Fig. 19-1, D). Thus, before their patients undergo ECT, neurologists order either an MRI or CT.
Signs of Increased Intracranial Pressure
Another sign of increased intracranial pressure, papilledema, occurs as pressure is transmitted along the optic nerve to the optic disks (Fig. 19-2). Although papilledema has a notorious association with brain tumors, it occurs late, if at all, in their course. In fact, among young adults, especially overweight females with menstrual irregularity, idiopathic intracranial hypertension (pseudotumor cerebri) is much more likely than a brain tumor to explain papilledema (see Chapter 9). In general, because only a small proportion of brain tumor patients have papilledema during an initial examination, its absence should not be taken as evidence against the presence of a brain tumor.
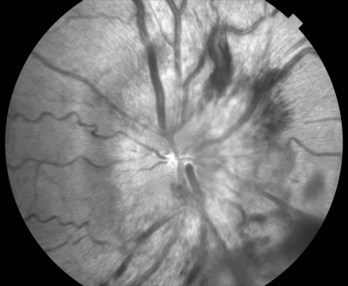
FIGURE 19-2 Papilledema’s main features consist of reddening of the optic disk, which loses its distinct margin, and distension of the retinal veins. In addition, the disk is elevated and hemorrhages appear at its edge. (Compare this disk to the normal optic disk in Figure 4-4.)
In considering manifestations of brain tumors, meningiomas constitute a special category. Unlike gliomas, as discussed previously, small meningiomas are common and usually small. Even large ones may remain asymptomatic. Also, they arise and usually remain entirely in extra-axial locations and produce characteristic syndromes. For example, a meningioma arising from the falx, a parasagittal meningioma, can compress the medial motor cortex and cause spastic paresis of one or both legs. A meningioma arising from the sphenoid wing can damage the adjacent temporal lobe and, because of its proximity to the orbit, cause proptosis and paresis of eye movement. Likewise, an olfactory groove meningioma can compress the adjacent olfactory and optic nerves and the overlying frontal lobe (see Foster–Kennedy syndrome, Chapter 4), causing anosmia, unilateral blindness, and, when large, frontal lobe dysfunction (see Chapter 7).
Initial Mental Symptoms
Direct Effects of Tumors
As a preliminary practical point, most rapidly evolving tumor-related cognitive impairments or personality changes result from a glioblastoma. Another point is that tumors in the frontal lobe produce “frontal lobe personality changes,” consisting of psychomotor retardation, emotional dulling, loss of initiative, poor insight, and reduced capacity to execute complex mental tasks. This clinical picture, like the clinical picture of frontotemporal dementia (see Chapter 7), consists of disturbances in behavior and affect that overshadow cognitive impairments, and those disturbances in turn overshadow physical impairments.
Medication and Other Treatment
In an acute, often debilitating side effect, chemotherapy tends to induce nausea and vomiting (chemotherapy-induced emesis). This problem usually stems from chemotherapy agents triggering the brain’s chemoreceptor zone and its adjacent vomiting center. These zones are located in the area postrema of the medulla, which is one of the few regions of the brain unprotected by the blood–brain barrier. The absence of a blood–brain barrier leaves the chemoreceptor zone freely accessible to any blood-borne substance. Thus, if people inadvertently ingest toxins, such as in poisonous mushrooms, they will immediately vomit. From a medical perspective, morphine, heroin, and high doses of L-dopa, as well as several chemotherapeutic agents, activate the chemoreceptor zone and induce vomiting. On the other hand, both dopamine-blocking agents and 5-HT3 antagonists prevent chemotherapy-induced nausea and vomiting (see Chapter 21).
Depending on the radiation’s total dose and rapidity with which it is administered, radiotherapy sometimes causes inflammatory arteritis and necrosis. Small strokes, which begin to accumulate 6–18 months after a course of radiotherapy, lead to a stepwise progression of cognitive impairments and personality changes resembling vascular cognitive impairment (see Chapter 11). Hemiparesis and dysarthria often accompany neuropsychologic changes. MRIs of patients with radiation-induced cognitive impairments typically reveal white-matter changes (leukoencephalopathy). Overall, radiotherapy induces more cognitive impairment than most chemotherapy agents.
Infections and Organ Failure
Infective agents sometimes invade the CNS, but not other organs. Because cancer patients often cannot respond with fever or leukocytosis to an infection, they may not show the usual markers. In fact, only 5% of cancer patients with meningitis will have the classic triad of fever, nuchal rigidity, and encephalopathy. Also, because of their immunocompromised state, cancer patients are susceptible to opportunistic infections. For example, progressive multifocal leukoencephalopathy (PML) probably results from a papovavirus that attacks CNS myelin. Indeed, CSF analysis in PML cases yields JC virus DNA. Usually complicating the late course of an illness, PML causes dementia and variable physical impairments, but not delirium, fever, or leukocytosis. PML has also complicated AIDS and immunosuppression therapy, including the multiple sclerosis treatment natalizumab (see Chapters 7, 15, and 20).
Paraneoplastic Syndromes
Systemic cancer sometimes causes neurologic syndromes not by invading the nervous system, but by inciting antibody-mediated immune responses directed against the CNS, PNS, or neuromuscular junction. Neurologists previously aptly called these disorders “remote effects of carcinoma,” but now they term them paraneoplastic syndromes. Paraneoplastic syndromes seem to begin with the patient’s synthesizing antibodies against a tumor’s antigens. The antibodies cross-react with neurons’ intracellular components, cell surfaces, or synaptic receptors. Antibodies involved in paraneoplastic syndromes include ones directed against voltage-gated potassium channels (VGKC) and N-methyl-D-aspartate (NMDA) receptors. Of the numerous paraneoplastic syndromes, three are particularly relevant: Cerebellar degeneration, limbic encephalitis, and Lambert–Eaton myasthenic syndrome (LEMS). Their pathophysiology likely represents “molecular mimicry” that is analogous to antistreptococcal antibodies cross-reacting with basal ganglia to cause Sydenham chorea (see Chapter 18).
Lambert–Eaton Myasthenic Syndrome
In LEMS, small cell lung cancer provokes antibodies directed against the presynaptic side of the neuromuscular junction where they impair release of acetylcholine (ACh) (see Chapter 6). The antibody-induced neuromuscular junction dysfunction in LEMS causes proximal limb muscle weakness, which patients partly overcome with repetitive actions. Their weakness has different qualities and different distribution than myasthenia gravis – the well-known disorder of the ACh receptors on the postsynaptic side of the neuromuscular junction. Patients with myasthenia primarily have facial and extraocular muscle weakness that worsens on exertion. Antibody tests and electromyograms readily distinguish these two neuromuscular junction disorders.
Diagnostic Tests for Brain Tumors
Neurologists generally order CT or MRI of the brain, admittedly liberally, for patients who have intellectual decline, those over 50 years who show substantial emotional changes, most adults with headaches not attributable to migraine, cluster, or giant cell arteritis (see Chapter 9), or, as previously discussed, those with excessive concern. Neurologists often also suggest CT or MRI for patients with any new psychiatric illness severe enough to warrant hospitalization or ECT.
CT remains a satisfactory screening procedure in many situations (see Chapter 20). It is sensitive to most tumors and other mass lesions, rapidly performed, relatively inexpensive, permissible for patients with pacemakers, and tolerable for most with claustrophobia. It remains preferable for detecting acute intracranial bleeding, including subarachnoid hemorrhage, subdural hematomas, and intracerebral hemorrhages. CT will also detect fractures and other abnormalities of the skull. On the other hand, its ionizing radiation, at least in children, carries a risk of inducing a malignancy (see Chapter 20).
Neurologists generally do not perform an LP to analyze CSF when they suspect a brain tumor or other intracranial mass lesion because, in such cases, the CSF profile lacks a distinctive profile and rarely reveals malignant cells (see Chapter 20). More important, with large, expanding supratentorial mass lesions, an LP can precipitate transtentorial herniation (Fig. 19-3). Neurologists perform an LP when patients may have either carcinomatous or chronic infectious meningitis. Testing requires large volumes of CSF for neoplastic cells, chemistry studies, fungi, and bacterial and fungal antigens. In an exception to the general rule of not performing an LP in patients with a cerebral lesion, neurologists may perform one to test the CSF for Epstein–Barr virus in an AIDS patient found to have a cerebral tumor because a positive result would indicate a cerebral lymphoma and obviate surgery. Similarly, they may perform one in cases of suspected PML to look for JC virus DNA.
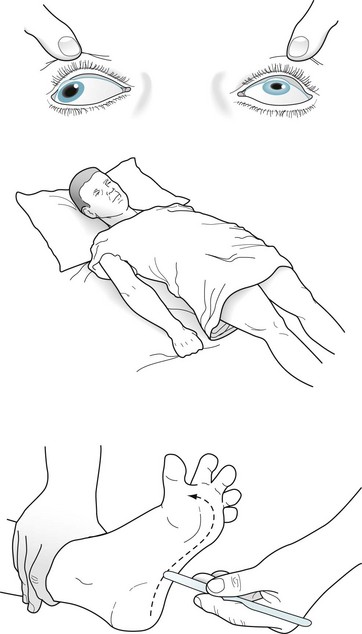
FIGURE 19-3 A patient in transtentorial herniation from a right-sided subdural hematoma (see Fig. 19-1, D) has coma, decerebrate (extensor) posture, Babinski signs, and a dilated right pupil. The right temporal lobe compressing the right-sided (ipsilateral) oculomotor nerve and brainstem through the tentorial notch causes this catastrophe.
Related Conditions
Pituitary Adenomas
Most pituitary adenomas are either prolactinomas, which secrete prolactin, or chromophobe adenomas, which do not. Although prolactinomas usually remain microscopic, they sometimes grow larger than 10 mm, in which case neurologists consider them macroadenomas. Pituitary adenomas of that size may exert pressure on surrounding structures (Fig. 19-4). Their upward pressure on the diaphragm sellae usually causes bitemporal and generalized headache. Compressing the optic chiasm, which is above the diaphragm, causes the visual field deficits. Initially they cause bitemporal superior quadrantanopia and, with further enlargement, bitemporal hemianopsia (see Fig. 12-9).
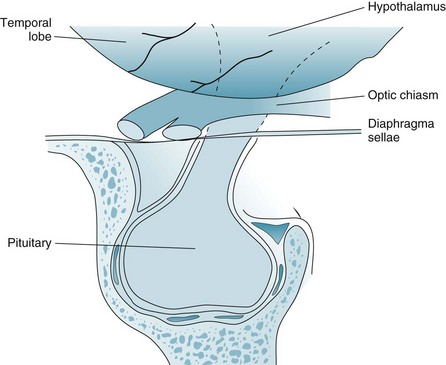
FIGURE 19-4 Pituitary adenomas grow laterally and inferiorly against the walls of the sella turcica and upward against the diaphragm sellae. Large adenomas compress the optic chiasm, which causes a distinctive bitemporal hemianopsia or bitemporal superior quadrantanopia (see Fig. 12-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








