Fig. 1.1
Elements of value-based medicine
1.
Autonomy, in which the patient has the right to choose or refuse methods for the management of their medical problem. Neurosurgeons and medical doctors must recognize the correct practice of autonomy is to work with the patient as a partner in order to make decisions about the best method of treatment.
2.
Beneficence, in which the physician or surgeon must consider the patient’s benefit as the sole goal for the relationship with patient. The neurosurgeon should ask himself/herself honestly if the suggested method brings the most benefit for the patient.
3.
Nonmaleficence, in which the neurosurgeon and the team have to do their best not to harm the patient. This risk of the proposed treatment should be minimized and explained to the patient very well, and every precaution should be taken to prevent it.
4.
Justice, in which fairness and equality of medical care is applied for every patient, which includes distribution of the doctor’s time and attention. Every patient has the right to receive the best possible and affordable medical care.
5.
Dignity, which flows in both directions. In every treatment plan and every interaction, the patient and the treating team should be treated with respect and dignity.
6.
Truthfulness and honesty, in which the relationship between a patient and the treating surgeon should be based on unconditional truth telling and honesty. The neurosurgeon should answer every patient’s question honestly and should admit openly any mistakes made.
Figure 1.2 shows the relationship between ethics and values and other components of medical care.
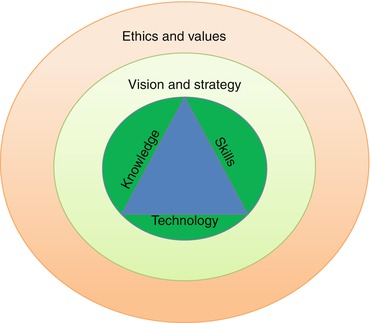
Fig. 1.2
Venn diagram showing the relationships of technical, strategic, and ethical medical care
The surgeon is first and foremost obliged to establish a relationship and rapport with the patient to understand their wishes and goals of treatment and to make them feel as comfortable as possible at a very frightening time. When discussing risks and benefits during informed consent, the neurosurgeon can gain valuable insight into the patient’s culture and beliefs. Culture and belief play a vital role in the discussion of benefits and harm – while a particular course of treatment may present the best physical outcome, it may cause irreparable psychological damage if it goes against the patient’s culture or moral standards. The neurosurgeon should assist the patient in weighing the benefits and harm, without asserting pressure or influence. Meaningful informed consent can only be reached when autonomy and beneficence work in tandem.
1.7 Conclusion
There is no doubt that history has great influence and impact on our daily lives. Human life is highly valued and respected in all ancient and modern civilizations. All religions without exception placed high value on human life, and medical practice in different periods of history was heavily influenced by religion. But ethical standards and norms cannot be written in stone and applied uniformly everywhere. They are now confronting more and more complex challenges, and ethical practices vary from culture to culture, religion to religion, country to country, city to city, and even hospital to hospital (e.g., depending on whether the hospital is a government/public hospital or private hospital).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





