26 Bypass Surgery for Complex Basilar Trunk Aneurysms
Clinical presentation
Mid- and lower-basilar aneurysms are uncommon lesions, accounting for fewer than 1% of all aneurysms in most neurosurgical series.1,2 Yamaura et al. reported a frequency of 5% (10/202) for posterior circulation aneurysms.3 In contrast, Drake and Peerless and Peerless et al. reported that mid- and lower-basilar aneurysms accounted for 15.2% (193/1266) of all posterior circulation aneurysms.4,5 Undoubtedly, however, this higher incidence reflected the referral bias of their institution.
The clinical features of ruptured aneurysms in the mid- and lower-basilar artery location tend to be indistinguishable from subarachnoid hemorrhage (SAH) from other cerebral aneurysms. As with any SAH, sudden headache, nuchal pain, altered mental status, nausea, and vomiting are the typical manifestations. Intraparenchymal bleeding, which can be associated with anterior circulation aneurysms, is rarely a feature of these aneurysms. As with other posterior circulation aneurysms, the natural history of these aneurysms appears to be that of high rupture rates.5 Unruptured giant aneurysms can produce neurological symptoms specific to their anatomic location, ranging from isolated cranial neuropathies to brainstem compression syndromes.
Fusiform and dissecting aneurysms are more common in the posterior circulation than in the anterior circulation and are associated with a poor prognosis.6 Large dolichoectatic aneurysms involving the basilar trunk and vertebral arteries may be the result of dissection with subsequent fusiform degeneration of the artery, progressive enlargement, and luminal thrombosis or may be a consequence of intracranial atherosclerosis. These lesions are particularly challenging and often require indirect approaches for their obliteration compared to the standard direct clipping techniques most often used for saccular aneurysms.
Management principles
Standard intraoperative management is utilized. Intraoperative hypotension is avoided. In fact, intraoperative blood pressure is allowed to run mildly hypertensive, especially during temporary vessel clipping. For brain protection, all patients receive intravenous doses of barbiturates (pentobarbital) to achieve electroencephalographic burst suppression. As required, brain relaxation is achieved with hyperventilation, mannitol, barbiturates, or spinal drainage of cerebrospinal fluid (CSF). Comprehensive electrophysiological monitoring is used routinely:7 somatosensory-evoked potentials, brainstem auditory responses (in both ears or the contralateral ear alone if ipsilateral hearing is to be sacrificed), and monitoring of the facial nerve and other appropriate CNs.
Surgical overview
The general principles for surgical treatment of aneurysms located in this part of the basilar artery are the same as those for any aneurysm.6,8–17 The main surgical difference relates to the anatomical considerations specific to the constrained aneurysm locations and the surrounding vital neuroanatomy. Regardless, the primary endpoint for the surgeon should be complete obliteration of the aneurysm from the circulation, with preservation of the parent vessels, particularly the perforators supplying the brainstem.
To achieve optimal aneurysm obliteration, maximal exposure of the basilar artery and the aneurysm itself is required. This exposure must be achieved without exposing the brain or critical structures to undue retraction while simultaneously obtaining adequate control of the parent vessel and aneurysm. Given the challenges of exposure in this region, specialized operative approaches are often necessary. In some cases, such approaches must be combined with the technique of hypothermic cardiac standstill.18–22 Alternatively, additional methods may be used for revascularization to allow proximal artery occlusion or trapping of the aneurysm.
Surgical decision making
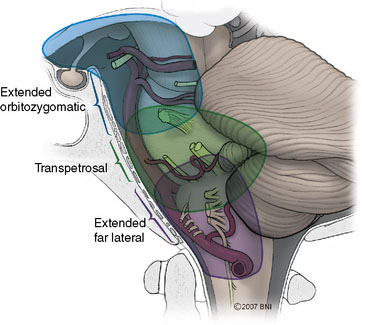
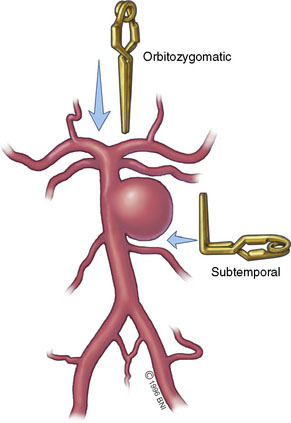
The various approaches that provide overlapping amounts of exposure can be seen in Figure 26–1. Typically, the subtemporal and orbitozygomatic approaches are used for basilar tip lesions, but the extended orbitozygomatic approach can provide access to the upper two-fifths of the basilar artery. Some aneurysms of the basilar trunk below the SCAs can be approached in this manner. The transpetrosal provides exposure further inferiorly, allowing the middle three-fifths of the basilar trunk to be accessed. With the combined supra- and infratentorial approach, access can be extended down to the vertebrobasilar junction. The far-lateral approach gives access primarily to the lower two-fifths of the basilar artery and is suitable for vertebrobasilar junction aneurysms. Both the far-lateral and extended orbitozygomatic approaches provide a view along the aneurysm neck, allowing a clip to be applied along this line of sight. In contrast, however, the transpetrosal approach exposes the aneurysm sac between the surgeon and the neck. A right-angled clip is required, increasing the technical difficulty of clip application (Figure 26–2).