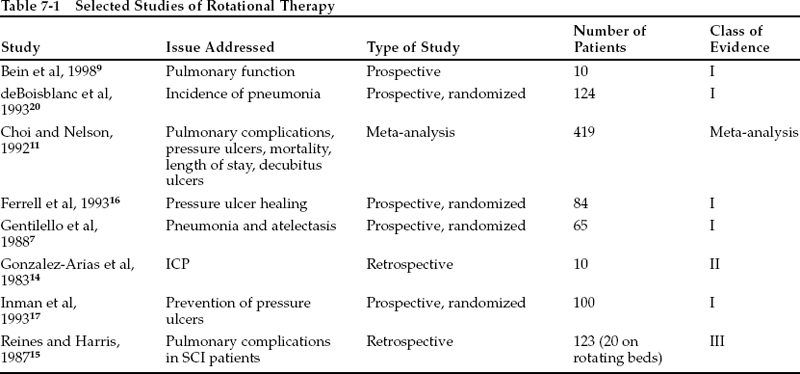
BRIEF ANSWER The prolonged immobility caused by traumatic brain injury (TBI) and spinal cord injury (SCI) renders patients with these conditions especially vulnerable to skin breakdown and to impairments in pulmonary function. Specially designed beds are particularly helpful in dealing with these problems. Class I, II, and III data demonstrate that beds that provide automatic side-to-side rotation improve pulmonary function and decrease the incidence of pulmonary complications. Class I data also indicate that lowair-loss beds decrease the incidence of, and expedite the healing of, pressure ulcers. However, not all studies have demonstrated such benefits, probably because of differences in design and implementation of the investigational protocols of the various studies. The effects of kinetic therapy on intracranial pressure (ICP) have not been studied as rigorously, but modest elevations of ICP that have sometimes been reported to occur with rotational therapy do not seem to be clinically significant, especially if rotation is not performed toward the side of a cerebral mass lesion. Background Rationale for Patient Mobilization Nosocomial pneumonia is a major problem in the critically ill patient. Its estimated prevalence is 5 to 10 per 1000 hospital admissions. The risk of pneumonia increases fourfold in patients receiving mechanical ventilation.1 Furthermore, the recumbent position is associated with decreases in tidal volume and in mucociliary transport, which in turn lead to atelectasis. In the 1960s, it became apparent that the established practices of bed rest and immobilization in the treatment of seriously ill patients increased their susceptibility to pulmonary complications and to loss of skin integrity. Thus, early use of kinetic therapy came to be recommended. Kinetic therapyis a general term used to describe the movement of immobilized patients. This movement is provided generally with the patient in the supine position and is directed at improving the perfusion of the lungs, decreasing atelectasis, and mobilizing secretions. Extrapulmonary benefits include reduction in venous stasis and prevention of skin and subcutaneous tissue breakdown. For many years, periodic changing of body position in critically ill patients has been accomplished by nurses physically positioning and turning patients every 2 hours. These efforts result in improved pulmonary blood flow, ventilation, and mobilization of bronchopulmonary secretions.2 This most basic form of kinetic therapy continues to be part of standard practice in many intensive care units.3 Notable adverse effects of this turning of patients, however, include cardiac arrhythmias, inadvertent removal of intravascular access and monitoring lines, significant manpower requirements, and job-related injuries.2 Furthermore, patients with head or spinal cord injury are especially difficult to mobilize readily. These negative aspects of an otherwise important treatment modality served as the impetus for the development of automated kinetic beds. Definitions and Types of Specialty Beds The first form of automated rotational therapy was introduced in 1967 by Keane.4 This bed was the forerunner of the current Roto Rest bed (Kinetic Concepts, Inc., San Antonio, TX). It consisted of a firm surface with surrounding pads that allowed side-to-side tilting of patients with maintenance of their supine position. Keane proposed that improved mobilization of secretions by such therapy could decrease pulmonary complications. The Roto Rest beds rotate from side to side through an arc of up to 62 degrees from the horizontal in each direction (total arc 124 degrees). Because these beds employ a rigid platform, they maintain immobilization of patients with unstable spines, and cervical traction may be applied. A disadvantage of these beds is that they are large, cumbersome, and very difficult to move. These considerations become important if a patient requires frequent transport for operative procedures or radiologic studies. Furthermore, use of such beds may be unnecessary in patients with stable spines. Kinetic therapy may also be administered via a Biodyne-type bed (Kinetic Concepts, Inc., San Antonio, TX). These beds are filled with multiple pockets of air that sequentially inflate and deflate to permit patient rotation through a large arc.5 Literature Review Scope of Studies Numerous studies have examined the effects of patient positioning and kinetic therapy on cardiopulmonary function. The results provide evidence for improved oxygenation and decreased atelectasis. Other investigations have assessed the effects of kinetic therapy on functional improvement, decubitus ulcer formation, and wound healing. Several of these reports provide class I or II evidence. Table 7-1 summarizes some representative studies of the effects of kinetic beds on pulmonary function, wound healing, and ICP in patients with head or spinal cord injury. Kinetic Therapy and Pulmonary Function Several prospective studies have compared mechanical rotational therapy to standard turning of patients every 2 hours by nursing staff. Kelley et al6 performed a prospective randomized study of 53 patients who had suffered an acute stroke that left them drowsy, stuporous, or lightly comatose (class I data). Pneumonia occurred in 13 of 25 patients (52%) in the standard hospital bed and in five of 18 (28%) in the rotational bed (p = .20) (author’s calculation). Despite this trend toward a lower rate of pneumonia in patients in the rotating beds, the mortality rate was slightly increased in the study group: six of 18 (33%) versus five of 25 (20%) in patients in the standard hospital beds (p = .48) (author’s calculation). Of further concern is that all patients who died of transtentorial herniation had been treated with rotating beds, including two patients enrolled in the study and three who were disqualified because of their short lengths of survival. In another study, Gentilello et al7 prospectively randomized 65 critically ill patients to treatment in a conventional hospital bed (n = 38) or to mechanical kinetic therapy (n = 27) (class I data). These patients suffered from head injury, spinal injury, or orthopedic injury requiring traction. Baseline data indicated that the two groups were comparable in terms of gender distribution and percentages with pulmonary contusion, spinal cord injury, and need for traction. Patients in the study group were rotated through an arc of 124 degrees every 7 minutes. The proportion of patients with major pulmonary complications (either atelectasis or pneumonia) was higher in the control group (66%) than in the study group (33%) (p <.01). Summer et al2 performed a randomized prospective study of continuous mechanical turning on 83 patients with the following illnesses: sepsis (30), chronic obstructive pulmonary disease/asthma (16), drug overdose (11), metabolic coma (12), stroke/neuromuscular (14) (class I data). Patients were randomized either to standard turning every 2 hours by nurses or to rotational therapy. The kinetic therapy group tended to have a shorter length of stay in the intensive care unit (ICU) (6.7 days for the kinetic therapy group versus 11.6 days for the control group; difference not significant). In a small study that used a historical control group, Pape et al8 concluded that bed rotation to 62 degrees significantly improved lung function compared with conventional supine positioning (class II data). Bein et al9 conducted a prospective investigational study to examine the effect of continuous rotational therapy with a Roto Rest bed on ventilation-perfusion inequality in 10 patients with acute lung injury (class I data). The etiologies of lung injury included lung contusion, polytrauma, pneumonia, and aspiration. These authors used the multiple inert gas elimination technique to assess ventilation-perfusion relationships. Each patient served as his or her own control, and supine measurements were compared with measurements performed while rotating. Continuous rotation led to an acute reduction in ventilation-perfusion mismatch when lung injury was mild to moderate, but not when it was more advanced. No significant differences were found in cardiac index, mean arterial pressure, or heart rate during continuous rotation versus the supine position. The authors hypothesized that the change in intrapulmonary shunting occurred as a result of redistribution of pulmonary blood flow from nonventilated to well-ventilated lung units. They also speculated that continuous movement on a rotating bed seemed to be of greater benefit than intermittent semidecubitus positioning. Dolovich and colleagues10 used a radiolabeled aerosol to investigate the effect of continuous lateral rotational therapy on lung mucus transport in 13 mechanically ventilated patients (class I data). The intent of this study was to determine if continuous rotation altered mucus transport in critically ill, intubated patients. Prior reviews had suggested that rotational therapy was associated with a decrease in pulmonary complications, possibly from improved clearance of secretions.1,11 Dolovich et al found that, in comparison to the supine position, continuous lateral rotational therapy to 30 degrees in each direction was associated with a slight but not significant increase in mucus clearance. It is possible that use of a greater depth of angle of rotation, i.e., rotation beyond 30 degrees, might have demonstrated significant improvements in clearance of mucus and diminution of atelectasis. Pearl
 7
7 
Can Special Beds Reduce the Incidence of Complications in Head-Injured and Spinal Cord—Injured Patients?
Can Special Beds Reduce the Incidence of Complications in Head-Injured and Spinal Cord—Injured Patients?
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree