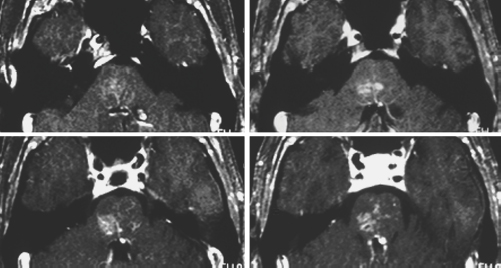
7 Quoc-Anh Thai, Gustavo Pradilla, and Daniele Rigamonti Cerebral vascular malformations are hamartomatous lesions1,2 originally classified by McCormick and colleagues into four separate categories: arteriovenous malformations (AVMs), cavernous malformations, capillary telangiectasias, and venous malformations.3 These disorganized vascular structures have distinct gross, histologic, radiographic, and clinical characteristics that generally differentiate them from one another. However, a spectrum of intermediate forms of the above categories has been described, suggesting that these lesions may actually be a continuum of progression of a single pathologic process. As such, it would be expected that combinations of these variants, in different stages of development, would be detected over time, and several of these lesions would be associated together within close proximity to each other. Reports have associated venous malformations with cavernous malformations,4–11 cavernous malformations with capillary telangiectasias,8,12,13 capillary telangiectasias with venous malformations,14,15 and venous malformation with both a cavernous malformation and capillary telangiectasia.2,8 With the continuing development of better imaging techniques, these lesions are being followed much more closely than before, and recent reports have also noted de novo formation of cavernous malformations in association with a venous malformation.5,6,11,16,17 These reports make a compelling story for a common pathway of disease, however, there is still no direct evidence supporting such a theory at this time. This chapter focuses on the known pathologic processes of the venous malformations, cavernous malformations, and capillary telangiectasias. We will then discuss the reported associations of the various forms of vascular malformations and examine possible pathologic links between them. Capillary telangiectasias, cavernous malformations, and venous malformations are all vascular malformations that occur on the capillary-venous side of the cerebral circulation. Morphologically, they are a group of disorganized vessels that resemble primitive anastomotic plexuses present during embryogenesis.18 In autopsy series, the incidence of cerebral vascular malformations is 4.6%.19 Venous malformations are the most common (3%), followed by capillary telangiectasia (0.8%) and cavernous malformation (0.3%).19 Capillary telangiectasias are collections of ectatic, thin-walled, endothelial-lined vascular channels separated by normal neuropril.20 These capillary-like channels lack smooth muscles and elastic fibers, and they range in size from saccular dilatations of capillary vessels to groups of channels that resemble cavernous spaces.12 They can be found throughout the brain or spinal cord, but they are more common in the posterior fossa, in the pons, as well as in the cerebral cortex and basal ganglia.15 They are thought to have a benign natural history20 and usually become symptomatic when there is hemorrhage. Instances of hemorrhage have been associated with the coexistence of a cavernous malformation.21 The etiology of capillary telangiectasia is thought to be congenital. Failure in the involution of brain capillaries, which normally occurs during the second month of gestation,21 results in formations of capillary telangiectasias associated with dilated draining veins and normal feeding arterioles.22 The hereditary form of capillary telangiectasia is autosomal dominant and is part of the Osler-Weber-Rendu syndrome, which is characterized by the development of capillary telangiectasias in the skin, gastrointestinal tract, nasal mucosa, and central nervous system.23 Capillary telangiectasias have also been reported to form de novo after radiation.24 Magnetic resonance imaging (MRI) is the best imaging modality to visualize capillary telangiectasias. They are hypo- to isointense on T1-weighted images and iso- to hyperintense on T2-weighted images. There is uniform enhancement with gadolinium contrast injection.20 On gradient-echo images, there is signal loss due to blood oxygen level-dependent contrast.25 Computed tomography (CT) and angiography are not as useful in detecting capillary telangiectasias. CT scans are often normal; there may be faint areas of increased density after contrast administration. Capillary telangiectasias are usually angiographically occult. Cavernous malformations (also referred to as cavernous angiomas, cavernous hemangiomas, capillary hemangiomas, and cavernomas) are well-circumscribed lesions of endothelial-lined vascular sinusoids without intervening parenchyma.26 These dilated vascular channels, or “caverns,” occur throughout the brain and spinal cord, most commonly in the subcortical white matter, external capsule, and pons.27 They resemble capillaries but have an abnormal basal lamina. There are no ensheathing pericytes, smooth muscle cells, or astrocytic processes, and there are gaps between endothelial cells lining the channels of the cavernous malformation.28 This yields an incompetent blood-brain barrier that may contribute to their etiology. The etiology of cavernous malformation has traditionally been presumed to be congenital and present at birth, but more recent reports of their ultrastructure, de novo formation, and pathophysiology suggest there may be other mechanisms. Cavernous malformations occur in a sporadic form, in which lesions are solitary, and in a familial form, which is accompanied by multiple lesions as well as a family history of seizures.26 Ultrastructural analysis shows that there is an incompetent tight junction and lack of blood-brain barrier components, which may lead to leakage of red blood cells into the surrounding brain and cause seizures.28 This leakage of red blood cells may account for the dynamic nature of cavernous malformations. A prospective MRI analysis showed that there is a tendency for progression from type IV to type I to type II to type III.17 There are also growing reports of de novo formation of cavernous malformation. Zabramski and colleagues followed 21 members of 6 unrelated families with familial cavernous malformations for an average of 2.2 years and documented 17 de novo formations.26 Cavernous malformations have also been reported to occur after stereotactic and radiation therapy29 and have been associated with viral infection23 and venous malformations,5,6,11,16,17 suggesting that other pathophysiologic mechanisms are involved. Cavernous malformations are visualized on MRI as having a reticulated core of mixed signal intensity surrounded by a hypointense rim of hemosiderin.30 This gives it an appearance similar a “mulberry” or “popcorn-like” lesion, which represents hemorrhage in different stages of evolution. These different stages have been classified as type I (subacute hemorrhage), type II (mixed subacute and chronic; the classic popcorn-like lesions), type III (chronic), and type IV (small punctate hypointensity on gradient echo).26 CT imaging usually shows an isodense to moderately hyperdense lesion on nonenhanced images; there could be little to prominent enhancement after contrast injection. Cerebral angiography has virtually no role for the sole purpose of studying cavernous malformations, as they are generally angiographically occult. However, as discussed later, they are sometimes associated with other vascular malformations that do appear on angiography. Venous malformations (also referred to as developmental venous anomaly, venous angioma, or venous caput medusae) consist of a group of veins resembling a chandelier or caput medusae draining normal brain tissue.31 The vessels are abnormally enlarged and are separated by normal parenchyma. These vessels then drain into a central venous trunk, which then drains into a venous sinus; there is no abnormal arteriovenous shunting. Found throughout the central nervous system in rough proportion to tissue volume, these lesions are relatively benign. Rarely, venous malformations may be associated with hemorrhage, and in those instances, there should be high suspicion of an associated cavernous malformation as the etiology.4 The etiology of venous malformations is thought to be congenital, resulting from failure of normal embryogenesis.2 By 45 days of gestation, the vasculature consists primarily of primitive embryologic medullary veins with a single draining vein into a venous sinus. By 90 days of gestation, these structures have normally evolved into the superficial and deep venous systems.32 Arrested development of this venous caput medusae during this window of development would result in a venous malformation that drains the surrounding normal brain structures. These hypotheses are corroborated by (1) findings of venous malformations in infants and children, (2) lack of mature venous systems surrounding these lesions, (3) angiographic opacification of venous malformations at the same time sequence as normal veins, (4) drainage of vascular malformations into normal extraparenchymal collectors, and (5) observation of venous infarction of the adjacent brain after removal of vascular malformations.21,32,33 Alternatively, there could be a focal abnormality in the venous drainage system during development, leading to formation of collateral, dilated medullary drainage veins.23 The diagnostic study for venous malformations is an angiogram showing the pathognomonic caput medusae in the venous phase.31 The arterial phase is usually normal, and there is sometimes a late capillary blush. On MRI, there are a series of tubular hypointensities on T1. These are better seen on T2, showing a venous plexus draining into a larger central vein, which exhibits high-velocity signal loss.34 There is generalized enhancement with gadolinium. Nonenhanced CT scans typically do not reveal venous malformations well; they are usually normal or show a slightly hyperdense, ill-defined lesion. As with MRI, there is enhancement after contrast injection.35 Cerebral vascular malformations with mixed characteristics or a combination of characteristics are well documented and may represent a spectrum of the same disease process. The incidence of these structures is unknown, as is their etiology. These malformations are mostly thought to be congenital, resulting from failure of the primitive vasculature to mature, and they are generally thought to be benign and static. However, reports have shown that some of these lesions are dynamic. A prospective MRI study showed that cavernous malformations evolve from being a type IV to type I to type II to type III.17 There are numerous reports of de novo formation of cavernous malformation in the presence of a venous malformation.5,6,11,16,17 Zabramski and colleagues26 found an overall frequency of 0.4 new lesions per patient per year in their series of familial cavernous malformations. Also, there are associations of each of the lesions with one another. The increasing number of reports of associations of two or more lesions in close proximity to each other makes it less likely that this is due to coincidental appearances of different diseases. It is estimated that 20 to 30% of cavernous malformations are associated with venous malformations.1,4,23 Also well documented is the association of cavernous malformations with capillary telangiectasias.28 Associations of capillary telangiectasias and venous malformation are less common. Hypotheses regarding the linkages between these lesions have been postulated since the 1930s, beginning with the Russell theory stating that capillary telangiectasias are precursors for cavernous malformations. Since then, numerous other hypotheses have surfaced and will be discussed in the following sections. The association of a cavernous malformation with a venous malformation is the most common of the vascular lesions, reported to be as high as 33% of cavernous malformations.36 Venous malformations are the most commonly encountered vascular malformations of the brain, accounting for up to 60% of cerebral vascular malformations. These benign lesions are usually found incidentally.31 They tend to become symptomatic when there is a hemorrhage, but this is usually always associated with a cavernous malformation.28,31,32,37,38 This has led many to suspect the causal linkage between the two lesions. Abnormal hemodynamics of venous malformations may induce the formation of a cavernous malformation. Numerous studies have cited abnormal venous drainage and pressure associated with the region drained by a venous malformation. A study of venous malformations that are associated with hemorrhages and cavernous malformations showed a high incidence of venous stenosis of the collector vein.11 Nuclear medicine studies have shown increased activity in the venous phase of the region drained by the venous malformation, suggesting that venous outflow is delayed.39,40 The result is a progressive venous overload and hypertension that is transmitted throughout the lesion.41 Subsequently, endothelial cell damage and small breakdown of the blood-brain barrier may lead to deposition of hemosiderin as well as local production of angiogenic factors.42 These events are hypothesized to form de novo cavernous malformations,5,7,41,42 and this process has been referred to as “hemorrhagic angiogenic proliferation”21 by Awad and colleagues. Reports of cavernous malformations appearing adjacent to venous malformations support the rationale that venous hypertension is linked with the pathogenesis of cavernous malformations.6,41,43 Furthermore, venous malformations in association with a hemorrhage or de novo cavernous malformations were found to have a high rate of stenosis or obstruction of the venous outflow.6,11 Therefore, whereas venous malformations are congenital, cavernous malformations appear to be hemodynamically acquired.6,43 Other hypotheses have been proposed by Wilson, stating that intermittent diapedetic extravasation of blood through the capillaries is the initiating process.42 This then results in stimulation of fibroblasts and the appearance of fragile capillaries prone to recurrent hemorrhage, leading to the formation of a cavernous malformation.37,38,42 Once formed, cavernous malformations continue to change due to other factors, further suggesting that there is a continuum of disease progression. An incompetent blood-brain barrier plays a role in the pathophysiology of cavernous malformations. From the first MRI description of cavernous malformations by Rigamonti and colleagues in 1987,30 cavernous malformations have been shown to enlarge, to regress, and to form de novo.17 This dynamic nature is attributed to abnormal venous pressure,6,41,43 hemorrhage, and hemorrhage resolution.17 As discussed, venous hypertension is generally thought to be associated with abnormal venous drainage of adjacent venous malformations. Intermittent hemorrhages may also be related to the venous pressure buildup. In addition, structural abnormality of basement membrane likely plays a major role. A recent ultrastructural and immunocytochemical study28 provided evidence that there is a lack of appropriate junctional complexes as well as ensheathing cells. This translates into an incompetent blood-brain barrier and weakened vessels and increased propensity for recurrent episodes of hemorrhages followed by resolution. This is reflected in MR images by lesion heterogeneity and changes in size17 showing blood of varying ages.17,30 The association of cavernous malformations and capillary telangiectasias has been described since 1931. Russell originally suggested that cavernous malformations could be formed from the fusion of adjacent, dilated loops of the capillary telangiectasia.44 The Russell theory was not generally accepted, but other hypotheses linking the two lesions have also been proposed. This is partially due to observations that cavernous malformations and capillary telangiectasias occur adjacent to each other with higher frequency than expected from coincidence alone. Increased venous pressure from capillary telangiectasias may lead to the formation of cavernous malformation. Capillary telangiectasias, similar to venous malformations, are thought to be congenital and remain relatively static during life. However, the abnormal vasculature is thought to induce venous hypertension and fragile vessels. This is hypothesized to cause clinically insignificant microhemorrhage.42 Subsequently, the blood products cause a reactive angiogenesis with new vessel formation and coalescence.21,42 This “hemorrhagic angiogenic proliferation” is thought to be responsible for formation of a cavernous malformation. Once formed, cavernous malformations have an ordered progression through the Zabramski classification, from type IV to type I to type II to type III.17,26 However, the progression is not linear, and transition from type IV to type I is only at a rate of 0.05 per patient year.45 There is no direct evidence showing this transition of capillary telangiectasia to a cavernous malformation, specifically a type IV, which appears to be the precursor to larger, symptomatic lesions. Indirect evidence from clinical, radiographic, and surgical-autopsy data support the hypothesis that capillary telangiectasias and cavernous malformations may represent two different manifestations of a single pathophysiologic process.12,30,46 Rigamonti and colleagues reported that the division of cavernous malformations and capillary telangiectasias is arbitrary,12 and there are transitional forms between the two lesions.12 In their series of 20 cavernous malformation patients, 35% of cavernous lesions had brain parenchyma in its center. The presence of brain parenchyma (the key differentiating characteristic between capillary telangiectasia and cavernous malformation) in a lesion that would otherwise be characterized as a cavernous malformation suggests that these transitional states are underrecognized. In autopsy, there were transitional forms of capillary telangiectasias identified, and these were correlated with MRI findings of small focal decreased intensities.12 In another report, Diamond and colleagues reported autopsy findings of pontine lesions showing a gradual transition from capillary telangiectasia to cavernous malformation; histology did not provide clear-cut distinctions.47 These findings make the distinction between a capillary telangiectasia and a cavernous malformation, specifically a type IV, difficult and seemingly arbitrary.12,47 However, Rigamonti and colleagues more recently reported that these are distinct entities, and the type IV cavernous malformations can progress through a series of MRI signal changes characteristic of types I, II, and III.45 This establishes that these type IV lesions are not capillary telangiectasias; however, capillary telangiectasias may still be a precursor lesion for type IV cavernous malformations. MRI studies show that both lesions can manifest in the same patient 80% of the time when there is a familial history of a symptomatic cavernous malformation.12 There is a positive correlation between the number of type IV lesions and the age of the patient,48 suggesting that type IV lesions accumulate in a patient over time. As suspected, there are more small lesions than large lesions identified in a particular patient, given the slow rate of change from type IV to type I, and this is especially true in asymptomatic patients.12,30,46 Given the coexistence of capillary telangiectasias and cavernous malformations, some shared characteristics, and correlation of type IV with age, it is plausible that there is a pathologic linkage between the two. The association of capillary telangiectasias and venous malformations is rare. There are only three case reports of such an association,8,14,15 so the hypotheses linking these two lesions is less compelling than that of the established associations discussed previously. However, the association with a venous malformation, which is known to have restrictive outflow and increased venous pressure, has led to speculations that there may be a causal linkage. Vascular malformations are congenital lesions with abnormal venous structures and associated hemodynamics that may more commonly lead to the formation of cavernous malformations and, in rare instances, the formation of a capillary telangiectasia. The central basis for this assertion is the findings of a restrictive outflow, decreased venous drainage, and increased venous pressure in venous malformations.11,39–41 This leads to vessel friability and propensity for microhemorrhage. This results in a reactive angiogenesis and the formation of new vessels and eventual coalescence into a capillary telangiectasia.21,42 Based on this hypothesis, venous malformations can be seen as the primary lesion when there are combinations of vascular malformations in a region.15 It would, therefore, be expected that if venous malformations were the primary lesion in vascular malformations, one would expect to see it in association with both a capillary telangiectasia and cavernous malformation. Indeed, a recent report cited the juxtaposition of a venous malformation, capillary telangiectasia, and cavernous malformation in the brain stem of a patient.8 Although this is the first published case report of such an association, the probability of such a constellation of vascular malformations adjacent to one another by chance alone is remote (Fig. 7-1). The low occurrence of this is congruous with the fact that the association between vascular malformations and capillary telangiectasias is already a rare phenomenon. Another support for the “hemorrhagic angiogenic proliferation” hypothesis21 is the finding of de novo formation of capillary telangiectasias after radiation.24 Radiation-treated vessels are more friable and prone to leakage of blood products, leading to the same cascade of events that ends with the formation of a capillary telangiectasia. This same course of events may also be involved in de novo formation of cavernous malformations after radiation therapy.23
Capillary Telangiectasias, Cavernous Malformations, and Developmental Venous Anomalies: Different Expressions of the Same Disease Process?
 Cerebral Vascular Malformations
Cerebral Vascular Malformations
Capillary Telangiectasia
Cavernous Malformations
Venous Malformations
 Mixed Patterns of Cerebral Vascular Malformations
Mixed Patterns of Cerebral Vascular Malformations
Venous Malformations and Cavernous Malformations
Cavernous Malformations and Capillary Telangiectasias
Capillary Telangiectasias and Venous Malformations
 Hemorrhagic Angiogenic Proliferation Hypothesis of Formation of Cerebral Vascular Malformations
Hemorrhagic Angiogenic Proliferation Hypothesis of Formation of Cerebral Vascular Malformations
Capillary Telangiectasias, Cavernous Malformations, and Developmental Venous Anomalies: Different Expressions of the Same Disease Process?
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree



