Chapter 5
Case Studies
Chapter objectives
- Provide case studies that illustrate clinical application of the Hypertonicity Intervention Planning Model (HIPM) presented in Chapter 3.
- Describe the process of assessment and location of upper limb characteristics along the HIPM continuum for these cases.
- Describe the process of establishing clinical aims, daily-life goals and potential intervention options based on the person’s upper limb characteristics and personal and situational factors.
- Implementation and outcomes of interventions are provided in Chapter 11.
Abbreviations
| AROM | Active range of motion |
| BoNT-A | Botulinum neurotoxin-A |
| CMC | Carpometacarpal (joint) |
| DIP | Distal interphalangeal (joints) |
| EPL | Extensor pollicis longus |
| FDP | Flexor digitorum profundus |
| FDS | Flexor digitorum superficialis |
| FE | Fingers extendeded |
| FF | Fingers flexed |
| HGF | House, Gwathmey and Fidler Thumb Classification |
| HIPM | Hypertonicity Intervention Planning Model |
| IF | Index finger |
| IP | Interphalangeal (joints) |
| LF | Little finger |
| MASMS | Modified Ashworth Scale of Muscle Spasticity |
| MCP | Metacarpophalangeal (joints) |
| MF | Middle finger |
| MTS | Modified Tardieu Scale of Muscle Spasticity |
| PIP | Proximal interphalangeal (joints) |
| PROM | Passive range of motion |
| RF | Ring finger |
| ROM | Range of motion |
| Z&Z | Zancolli and Zancolli Hand Classification |
5.1 Wendy
5.1.1 Background information
Wendy is 69 years old, and had a left stroke resulting in right hemiplegia nine years ago. She has aphasia, walks with a single point stick and, together with husband Paul, leads an active and social life. Before her stroke she worked part time as a nurse and enjoyed activities such as golf. At initial assessment, Wendy indicated that she assisted with daily care tasks such as dressing and showering using her unaffected arm. Paul completed all household tasks such as cooking, cleaning and shopping. At rest, Wendy positioned her right upper limb with her elbow flexed to 90°, wrist flexed to 35°, her RF and LF MCPs hyperextended and all finger PIPs flexed (Figure 5.1). She was able to shrug her right shoulder to lift her arm and place it on the arm rest of her chair. Other than this, Wendy reported she did not use her right arm in any functional tasks.
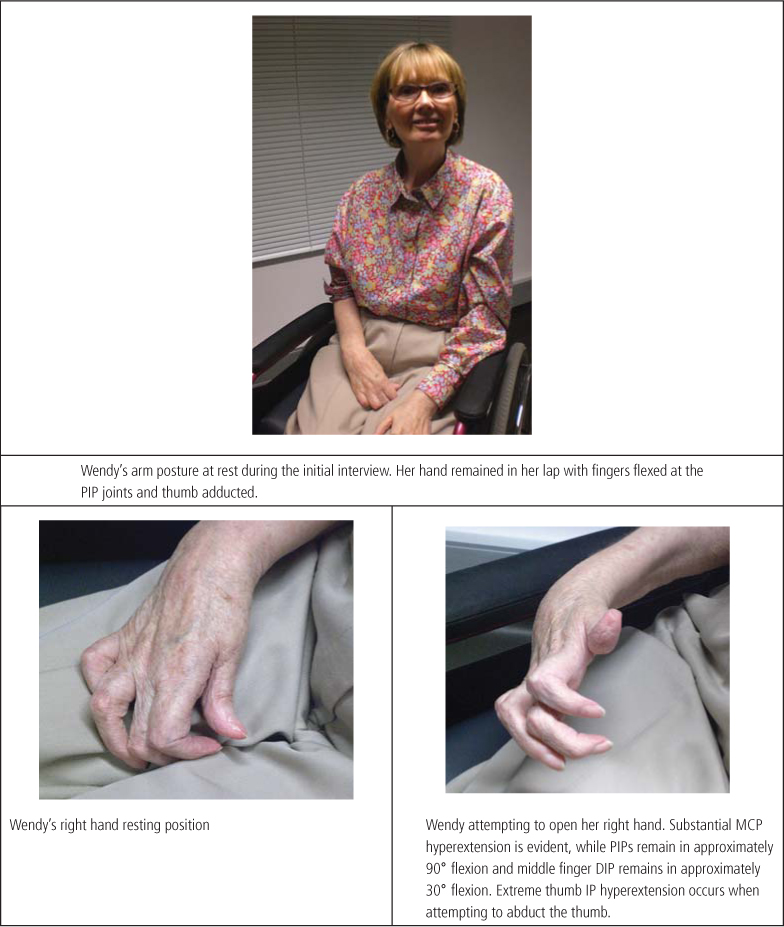
Figure 5.1 Pre-intervention arm and hand positioning.
Wendy had received a resting hand splint as part of her rehabilitation programme several years ago, but reported that the splint had become uncomfortable and she had ceased wearing it. Wendy had been receiving Botulinum neurotoxin-A (BoNT-A) injections every three months for the two years previous to this assessment. Injections were reportedly located at her shoulder, elbow flexors and forearm. Wendy and Paul reported that the injections usually made it easier for Paul to passively lift her arm during tasks such as showering. She also noticed that her fingers were straighter for a while following the injections and at these times she was able to initiate small active movements of her fingers. Wendy’s most recent injections occurred six weeks before the assessment. Paul and Wendy reported that they were concerned about the “clawing” position of her hand (Figure 5.1).
5.1.2 Positive and negative features
Positive and negative features were discerned from observing Wendy’s resting position and the way in which she moved her arm and hand (Table 5.1). The distinction between positive and negative features is described in Chapter 4 (Box 4.4).
Table 5.1 Positive and negative features: Wendy’s right upper limb.
| Positive Features | Negative Features |
| Primary Elbow flexion Forearm pronation Wrist flexion Thumb adduction (CMC) Finger PIP flexion Secondary Finger MCP hyperextension (RF, LF) Thumb IP hyperextension | Shoulder flexion Elbow extension Forearm supination Wrist extension Thumb abduction, opposition (CMC) Thumb IP flexion (lack of flexion allows hyperextension) Finger MCP flexion (lack of flexion allows hyperextension in RF and LF) Finger PIP extension Lack of proximal and distal transverse hand arches (leading to a flat hand) |
5.1.3 Upper limb range of motion, hypertonicity and movement patterns
Once the distribution of positive and negative features was determined, the active and passive ranges of motion (AROM, PROM) and hypertonicity measures required became evident. As Wendy and Paul reported that Wendy had minimal active movement, her AROM was measured at most joints to ascertain the extent of her movement control and weakness. Where positive or negative features were impacting on a joint, PROM was measured in the opposite direction to her joint posture. For example, as her finger MCPs postured in hyperextension, passive MCP flexion was measured. The Modified Ashworth Scale (MASMS) was used to rate the stiffness or resistance to passive movement in relevant muscle groups; the Modified Tardieu Scale (MTS) was used to measure spasticity and to determine whether contractures existed in the muscle groups that demonstrated limited PROM. Initial assessment (pre-intervention) measures are presented in Table 5.2.
Table 5.2 Range of motion, stiffness and spasticity: Wendy’s pre-intervention measures.
| Right UL | AROM | PROM (R2) | MASMS | MTS (X) | Catch (R1) | Comments |
| Shoulder Flexion | 5° | Full | 0 | 0 | No catch elicited | Flicker of active shoulder abduction and small amount of scapula elevation when attempting to move shoulder |
| Elbow | ||||||
| From resting position at 90° to 125° of flexion | Full | 1 | 0 | No catch elicited | Active movement in mid-range Stiffness evident initially, but relaxes when passively ranged |
| 0° | 145° | 1+ | 2 | 115° | Spasticity angle = R2 – R1 = 145°–115° = 30° |
| Supination | To mid-position | 60° | 1 | 1 | No catch elicited | |
| Wrist extension (FF) | Nil | 15° | 1+ | 1 | No catch elicited | |
| Wrist extension (FE) | Nil | To 20° of flexion (from flexed resting position, i.e. –20° from neutral). See Figure 5.2 | 3 | 2 | Catch at 30° flexion (i.e. –30° from neutral) | Spasticity angle = R2–R1 = (−20°)–(−30°) = 10° |
| Finger MCP flexion | 10–20° at IF and MF during grasp, nil at RF and LF (remain in hyperextension) | Full | Tissue stiffness | 0 | No catch elicited | Increased MCP hyperextension when attempting to open hand |
| LF PIP extension | Nil – remains in 90° flexion (flickers of extension at PIPs and DIPs of other fingers when attempting to open hand) | To 40° of flexion (from flexed resting position, i.e. –40° from neutral) | NA | 0 | No catch elicited | Possible LF PIP joint contracture, therefore an individual PROM measure was taken at this joint |
| Thumb | ||||||
| 30° | 35° | Nil detected | 0 | No catch elicited | Active abduction occurs with IP and MCP hyperextension |
| Nil | To neutral (from hyperextension) | Nil detected | 0 | No catch elicited |
R1 = angle of muscle reaction when limb moved at fast velocity; R2 = PROM when limb moved at slow velocity (Section 4.3.5); X = quality of muscle reaction on the MTS.
5.1.4 Interpretation of measures and movement patterns
Assessment indicated that:
- Wendy had organic contractures in her elbow flexors (passive extension to 145°), forearm pronators (passive supination to 60°), wrist flexors (wrist extension with fingers flexed was 15°), finger flexors (wrist extension with fingers extended was only to 20° of flexion, that is, it did not reach neutral; see Figure 5.2) and thumb adductor (abduction to 35°). She also had a possible contracture in her long thumb extensor (extensor pollicus longus [EPL]), as her thumb IP could only be passively flexed to neutral from a hyperextended position.
- Of these contractures, her short finger flexor (FDS, which flexes the PIP joints) was most affected.
- Wendy’s finger flexors were severely affected by hypertonicity (MASMS 3), with other muscle groups demonstrating MASMS 1 to 1+
- Wendy’s finger flexors and elbow flexors were moderately affected by spasticity (MTS 2).
- Even when Wendy’s wrist was in full flexion, her little finger PIP joint could not be ranged to neutral. This indicated a possible fixed joint contracture and so a separate measure was taken at this joint.
- Wendy had minimal active movement at her shoulder and some active elbow flexion and forearm supination. Shoulder elevation, elbow flexion and supination occurred together when she attempted to flex her elbow.
- Wendy had no active elbow or wrist extension, indicating possible paralysis in these muscle groups.
- She was unable to reach towards an object using active shoulder and elbow movement but when an item was held close to her hand and she was asked to open her fingers, flickers of PIP and DIP extension were apparent in all fingers, with accompanying MCP hyperextension. She was unable to open her fingers enough to place the object into her palm (PIPs remained in 90° of flexion), but rather pushed it into her palm with her non-affected left hand. She was able to abduct her thumb actively to 30° but could not actively oppose her thumb around the object. Her thumb therefore remained adducted against the object, resulting in an insecure grasp (Figure 5.3). Her thumb IP joint remained in a hyperextended position. With the object in her hand, Wendy’s finger PIPs and DIPs were positioned in significant flexion due to the hypertonicity/contracture in her finger flexors. She flexed these joints further using weak but detectable active finger flexion to keep the item in her hand. Her little finger and ring finger MCPs remained in hyperextension while her middle and index fingers moved into slight flexion. Her wrist remained in flexion throughout.

Figure 5.2 Wendy’s pre-intervention passive range of motion for wrist extension with fingers extended.
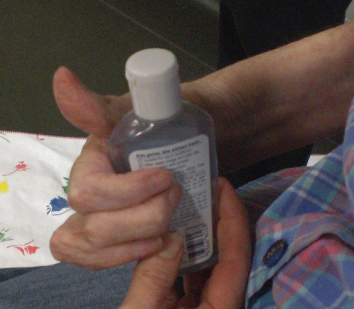
Figure 5.3 Wendy’s grasp at initial assessment.
While negative features were contributing to Wendy’s difficulty in actively using her arm and hand, positive features, particularly contracture and increased hypertonicity in her finger flexors, were also making it harder for her to open her hand and to position it with joint alignment at rest. This meant that it was difficult for Wendy’s husband to assist her with daily care tasks such as dressing, as her fingers would often become caught when donning sleeves. The spasticity and contracture in Wendy’s elbow flexors was not of concern to either her husband or herself at this time, as she had enough passive extension for most daily self-care tasks and her elbow did not flex significantly when walking or during other activities.
5.1.5 Situating the person’s upper limb characteristics on the HIPM continuum
The HIPM (Table 3.2) categorises upper limb capacity along a continuum of ‘mild’ to ‘severe’ disability. The assessment of Wendy’s upper limb characteristics placed her capacity within the ‘moderate to severe’ HIPM 2b category. The upper limb features typical of this category are presented in Table 5.3, with Wendy’s characteristics highlighted in italics.
Table 5.3 Association between the HIPM and Wendy’s assessment findings.
| HIPM 2ba | |
| Impairment (body structure) |
|
| Function |
|
a HIPM 2b category of upper limb features extracted from Table 3.2.
b Based on assessment findings, Wendy’s upper limb characteristics that are associated with the HIPM 2b category are italicised.
5.1.6 Negotiating daily-life goals based on a realistic level of function
The client’s positive and negative features, active and passive movement, and degree of spasticity/ hypertonicity can be used by the clinician to predict a possible “level of function” within which to situate goals (see Section 4.4.1).
Wendy had some active movement in her fingers, thumb and forearm, but significant proximal weakness, therefore, it was considered realistic to aim for two levels of function:
- Comfortable positioning of the limb to support whole body movement/ positioning/ assistance from carers.
- Use of the hand as an active stabiliser – whole hand gross grasp.
Personalised, daily-life goals were negotiated based on these levels of function and in terms of their meaningfulness to Wendy and Paul. The goals were to:
- Increase ease and speed of dressing.
- Stabilise items with a right whole hand grasp while manipulating them with the left hand, for example, peeling a banana, holding a toothbrush to put toothpaste on, holding a tube of moisturiser while opening it with the left hand, holding a golf club to putt.
5.1.7 Clinical aims to support goal achievement
Once goals have been established, the clinician is able to identify clinical aims for upper limb function or status that directly connect to the achievement of the person’s daily-life goal for activity or participation (Section 4.2.4). These clinical aims can be expressed at two levels: (i) the position, movement or action components that are required to achieve the goal, and (ii) underlying these, the changes to impairment factors, such as hypertonicity, weakness and range of motion, that might allow the position, movement or action to be achieved. Table 5.4 matches the movements/positions/actions and associated changes to impairment factors that are required to achieve Wendy’s daily-life goals.
Table 5.4 Clinical aims supporting achievement of Wendy’s daily-life goals.
| Daily-Life Goal | Clinical Aims | |
| Movement/position/ action | Impairment factor changes | |
| Increase ease and speed of dressing |
|
|
| Stabilise items with whole hand grasp (banana, toothbrush, moisturiser, golf club) | ||









