Case Studies
Apple the Approach to Some Real Patients
Apple the Approach to Some Real Patients
You are now ready to try your hand at diagnosing neurologic conditions based on the level of the NeurAxis that seems most likely affected given the signs and symptoms present. These cases should allow you to use and further hone your diagnostic skills while providing some useful information about a number of common neurologic conditions. The discussion of potential answers follows each individual case. Be sure to use the NeurAxis chart for reference!
Case Study 1: “Maybe it’s a pinched nerve?”
Mr. Alchemy is a 64-year-old right-handed retired chemist who was sitting still (reading), when his left hand and arm suddenly lost feeling and strength (ability to move). He picked his left arm up with his right arm, and it felt “like a noodle.” There was no tingling, burning, or discomfort at all. There was no change in vision, speech, language, or mentation. The lower extremity did not seem involved, but he didn’t walk much so he is not entirely certain. The sensory loss improved slowly over 2 days, but he still notices mild weakness and admits to trouble fastening buttons with his left hand (trouble with fine motor movements). His grandmother, father, sister, and uncle died in their 40s or 50s from heart disease.
Your examination reveals diminished rapid alternating movements in the left hand and minimal finger abduction weakness. Muscle stretch reflexes are hyperactive in the left upper extremity compared to the right. There is also subtle facial asymmetry, with the left side of the mouth somewhat lower than the right. The left-sided facial weakness appears to be new when compared to his driver’s license photo.
What is your initial clinical impression?
cervical radiculopathy
carpal tunnel syndrome (median neuropathy at the wrist)
stroke (cerebral infarct)
polymyositis
DISCUSSION
a) Cervical radiculopathy certainly can lead to some limb weakness and dermatomal sensory loss. Nerve root compression, however, is usually very painful, and the weakness would be isolated to the affected myotome in that limb. With cervical radiculopathy, the limb pain may also worsen significantly with rotation of the head in the direction of the involved limb (foraminal closure test) and with coughing or sneezing (Valsalva maneuver). The pattern of symptoms in the lower extremity would be similar for lumbar radiculopathy. Here, straight leg raising and/or extension of the lumbar spine may make the symptoms worse. Back or neck pain are not necessary features of radiculopathy. In fact, they are often absent in pure radiculopathy.
b) Carpal tunnel syndrome is a common peripheral mononeuropathy. You may want to refresh your memory by reviewing a peripheral neurology reference, noting that sensory change with median nerve damage is usually isolated to the lateral three or four digits (including the thumb, index, and middle fingers), and any weakness would be detected only in the thenar eminence (mainly, the abductor pollicis brevis). With median neuropathy due to carpal tunnel syndrome, the symptoms generally are insidious in onset, and typically wax and wane during the day and night, depending on activity and hand position.
d) Polymyositis is an inflammatory myopathy that primarily affects the limb muscles. Because it is a muscle disorder, there
should be no sensory loss. The weakness is usually primarily proximal in distribution, with distal fine motor movements (rapid alternating movements) relatively spared. Although myopathy can be somewhat painful, any discomfort would be widespread (i.e., not focal or isolated to a single limb).
should be no sensory loss. The weakness is usually primarily proximal in distribution, with distal fine motor movements (rapid alternating movements) relatively spared. Although myopathy can be somewhat painful, any discomfort would be widespread (i.e., not focal or isolated to a single limb).
c) Correct: Stroke is the best choice available because you already suspect a CNS problem based on the presence of painless weakness with sensory loss. In addition, rapid movements were slowed and muscle stretch reflexes were hyperactive in the same limb, both suggesting CNS dysfunction. Although you likely considered cervical myelopathy, the patient’s facial weakness suggests a problem “above the neck.” The presence of aphasia certainly would have helped you isolate the problem to the cerebral hemisphere, but it would not be expected in this case because his problem appears to be located in the nondominant hemisphere. MRI scan of the brain did, in fact, reveal a small right MCA distribution subcortical infarct. Stroke prophylaxis was instituted after the appropriate medical evaluation, and the patient continued to improve some with rehabilitation over the next 3 months.
Case Study 2: “I keep blinking out.”
Sarah is a 23-year-old student who is very concerned that she may have to drop out of college this semester. She occasionally has trouble studying for tests because of spells that leave her feeling tired and confused for the rest of the evening. These spells are unpredictable other than being immediately preceded by an odd familiar feeling that she has “been there before” (déjà vu). She then seems to just lose time for a couple of minutes. This has been occurring about two or three times per month since the semester began 4 months ago. Some of these spells have been witnessed by her roommate, who reports that she will stare around the room and pick at her clothes or rub her face, but she does not respond to questions during the spell. Afterward, she is very tired and wants to sleep, and when she awakens, it is often too late to complete her homework or finish studying. She also mentions episodes of “passing out” several times per year since adolescence, labeled “hypoglycemia.”
Her complete neurologic examination (including mental status) is normal, as are her vital signs.
Your clinical diagnosis is:
hypoglycemia
complex partial seizures
cerebellar hypoplasia
absence seizures
CLUES
Sarah’s loss of consciousness (or limited responsiveness) implies an alteration of cerebral hemisphere and/or brainstem function. This type of dysfunction may be due to any number of conditions that affect one or both of these regions. Several clues are present in her history that lead you to the diagnosis. To begin, when a spell “comes and goes” in neurology three things should always be considered: (i) vascular “event” (TIA or syncope), (ii) seizure, and (iii) migraine accompaniment. Clearly, there are many other things that can lead to symptoms that come and go, but these are by far the most common in neurology. If the diagnosis continues to remain elusive after considering these, a consultation may be necessary (possibly with a neurologist, psychiatrist, or sleep specialist, depending on the story).
Syncope is sudden, usually with minimal to no warning, and affected patients recover almost as soon as they “hit the ground” (assuming they fall from a standing position). It rarely occurs when people are sitting or lying down unless a cardiac rhythm disturbance contributes to the global hypoperfusion of the brain. Clues that suggest syncope include occurrence immediately on standing (e.g., orthostatic hypotension), a history of severe dehydration, or associated certain psychological stressors (e.g., some faint at the sight of blood).
TIAs tend to affect individuals with vascular disease risk factors such as advanced age, hypertension, heart disease, smoking, diabetes, hypercholesterolemia, and family history of similar problems. The average length of a TIA is 30 to 60 minutes, although the symptoms may last hours (by definition, up to 24 hours). These patients report a sudden full or partial loss of function (i.e., “negative” symptoms), such as loss of vision, language function, strength, or sensation. “Positive” symptoms such as picking at clothing, limb pain, or seeing bright flashing lights are very uncommon. Typically, those who have a large number of TIAs (especially if these continue for months or years) will eventually experience a stroke with the resultant permanent clinical deficit.
Recurrent seizures occur in patients who suffer from epilepsy. There may be altered consciousness along with “positive” symptoms such as limb shaking, tongue biting, and/or automatisms (stereotyped repetitive movements). Sometimes the symptoms such as limb shaking or paresthesias will actually “march” or evolve over a minute or two. This implies the seizure was partial in onset with spreading (sometimes called “Jacksonian march”). Likewise, any type of warning such as a strong odor, irrational fear, déjà vu (delusion of recognition), or jamais vu (familiar things seem unfamiliar) suggests that the seizure was focal or partial in onset (even if there is secondary generalization). A postictal state of confusion and/or feeling very tired often occurs after complex partial and convulsive seizures.
Migraine accompaniments are usually visual but may be somatic as well. Although possible, loss of consciousness is not a commonly reported problem with migraine. Flashing lights (often bright and colored), evolution of a zig-zag line followed by scotoma, or tingling of the face or limbs are among the more common symptoms. These are most often “positive” and evolve over 10 to 15 minutes. Headache may or may not be reported immediately after migraines occur, but there is usually a history of headaches. Remember to inquire about pain because individuals with frequent headaches may neglect to mention the associated pain, in part because they are so accustomed to having head discomfort.
DISCUSSION
a) Hypoglycemia occurs almost exclusively in diabetics, especially when they use more medication or insulin than necessary or miss meals after their diabetic medication. The warning (if any) would typically include diaphoresis, tachycardia, and feeling light headed. The person would not usually spontaneously recover after just a few seconds to minutes unless given oral or intravenous glucose.
c) Even if you don’t know exactly what cerebellar hypoplasia is, you recall that an isolated problem in the cerebellum will not lead to changes in consciousness unless there is mass effect placing pressure on the brainstem. A smaller than usual cerebellum (hypoplasia) would not cause intermittent spells of altered consciousness. If a cerebellar lesion of any type does expand due to growth, hemorrhage, or edema, then coma might ensue. This type of problem would not “come and go” for minutes at a time
(especially over months or years). If the brainstem were involved, one would also expect to see other overt clinical signs of brainstem compression.
(especially over months or years). If the brainstem were involved, one would also expect to see other overt clinical signs of brainstem compression.
d) Absence seizures are a specific type of generalized onset seizure that begins in childhood or adolescence. They rarely begin as late as early adulthood and are not associated with a warning (aura). These seizures are usually brief (5-10 seconds) and may occur as many as 10 to 20 times in a single day, but without a postictal state of confusion or lethargy. It is important to consider this type of spell in a young person (child or adolescent) because the etiology and treatment is different than with partial onset seizures. The former (outdated) term for these seizures is “petit mal.” When episodes of staring begin in the late teen or adult years, they are usually not “absence” or “petit mal” seizures. If seizures are the cause, then they are likely complex partial in type. Remember that absence seizures are quite different from complex partial seizures (see next paragraph), and with very rare exception, do not begin in young adulthood or after.
b) Correct: Complex partial seizures are partial onset epileptic seizures that arise from one region of the brain and cause altered consciousness or awareness. They usually begin in the temporal or frontal lobe and may be preceded by an aura or warning (which is actually a focal seizure itself). There may be associated automatisms as well, and the spell generally lasts 0.5 to 2 minutes. Afterward, there is often a postictal state of confusion or lethargy that may last minutes to an hour. With seizures, the “partial” refers to the onset being focal, and the “complex” refers to altered consciousness (with amnesia for part of the spell being common). Isolated limb shaking due to seizure would correctly be labeled “focal” unless altered responsiveness or amnesia was noted. A generalized convulsive seizure could be either primarily generalized in type (generalized at the onset) or secondarily generalized (focal in onset). If an aura is reported prior to a seizure, this serves as a reliable clue that the seizure was, in fact, focal in onset. Most adults with new onset seizures will need brain imaging to rule out a treatable focal brain abnormality (e.g., a tumor).
This patient was diagnosed with epilepsy, which is defined as two or more unprovoked seizures (not predictable and not caused by
a “fixable” problem). She was subsequently found to have mesial temporal sclerosis by brain MRI, which many believe is evidence of a remote injury or developmental abnormality. Her EEG revealed epileptiform discharges emanating from this region. These tests supported the diagnosis of a complex partial seizure disorder. In patients with epilepsy, however, the EEG and MRI imaging of the brain are not always abnormal. She was treated with the antiepileptic drug carbamazepine (Tegretol) for seizure prophylaxis and was able to continue with her college education.
a “fixable” problem). She was subsequently found to have mesial temporal sclerosis by brain MRI, which many believe is evidence of a remote injury or developmental abnormality. Her EEG revealed epileptiform discharges emanating from this region. These tests supported the diagnosis of a complex partial seizure disorder. In patients with epilepsy, however, the EEG and MRI imaging of the brain are not always abnormal. She was treated with the antiepileptic drug carbamazepine (Tegretol) for seizure prophylaxis and was able to continue with her college education.
Case Study 3: “He keeps getting lost on the way home.”
Ms. Watson brought her husband to your clinic because he has repeatedly had trouble navigating his way to the local grocery store and has become lost several times on the way home. He doesn’t really think there is a problem and, in fact, is rather perturbed that she brought him to see the doctor. He is a 78-year-old retired engineer who has stopped playing poker with his “buddies” because he kept losing track of which cards were in his hand and which game they were playing. His wife reports that he has also had some difficulty remembering phone numbers and even names of familiar people. She now manages the checkbook and pays the bills because of several significant errors he made writing checks over the past year.
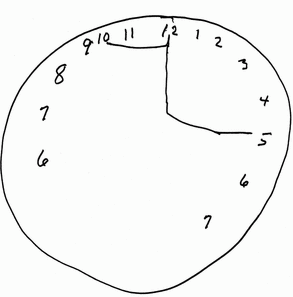
Your examination reveals a fairly jocular, pleasant elderly man who has normal cranial nerve, motor, and sensory function. He, of course, knows who he is and recognizes his wife, and is somewhat irritated with her for bringing him to the clinic. He assumes she brought him in “for a checkup.” He can correctly state the month and the year, and knows a few details about the current president, but can’t seem to come up with his name. When he draws the face of a clock for you, the numbers are spaced unevenly with the 6 and 7 repeated (see clock). When asked to show “10:15,” the hands originate at the 12 instead of at the center, and the minute hand incorrectly points toward the 5. He refers to the hands as “arms” when asked how he indicated the time.
You suspect:
cervical myelopathy
complex partial seizure disorder
left hemisphere stroke
dementia, possibly Alzheimer’s disease
|
DISCUSSION
a) Cervical myelopathy is a problem that may lead to weakness of all four limbs and upper motoneuron signs on your examination. This would not cause difficulty with cognition, which Mr. Watson clearly demonstrates.
b) Complex partial seizures are associated with altered consciousness, but the seizures “come and go” causing distinct but intermittent changes in neurologic function (and his problems are consistently present).
c) Left hemisphere stroke would lead to weakness and/or sensory change on the right side of the body. Language function may be abnormal as well, with varying degrees of aphasia, depending upon the exact location and size of the injury. Although language function is affected in many patients with dementia, to diagnose dementia there must be a significant change (decline) in memory plus at least one other domain of cognitive function (e.g., praxis, language, visuospatial perception, calculation, executive functioning).
d) Correct: Dementia is the diagnosis in this case, and overall Alzheimer disease (AD) is the most common cause of dementia in the elderly. When mildly affected individuals are examined early on in the process, the standard “Mini Mental State” score often falls in the expected “normal” range. This is a standard test of more basic mental function that is scored on a 1 to 30 scale. Loss of ability to perform higher-level cognitive tasks usually occurs first, and this is sometimes more difficult (and time consuming) for the examiner to detect. Historically, the patient’s spouse or a close friend will often be the one to notice these “thinking problems” first. The patient may exhibit difficulty with practical (daily) activities such as balancing the checkbook, driving to the grocery store, keeping up with a golf score or poker hand, and the like. More detailed discussion with the patient will help identify other problematic areas such as trouble remembering names of close friends or difficulty with handling novel situations such as a minor traffic accident. Once cognitive difficulty has been confirmed, you then know that there is some type of problem affecting the cerebral hemispheres. The actual cause, however, cannot always be confirmed with currently available laboratory tests. Brain imaging rarely reveals evidence of a treatable cause such as subdural hemorrhage, but some potentially treatable causes are not visible on neuroimaging. These include pseudodementia (memory difficulties due to depression) and medication side effects (especially in cases of polypharmacy). In Mr. Watson’s case, the MRI brain study showed moderately severe generalized cerebral atrophy, and serum studies also did not reveal a treatable cause. A clinical diagnosis of AD was made, and he continued to progress (worsen) for several years until nursing home placement was necessary. At the current time, the only method of definitively “proving” a diagnosis of AD is by microscopic examination of brain tissue, which is usually obtained at autopsy.
Case Study 4: “We just found him on the sidewalk.”
“John Doe” was discovered unconscious on the sidewalk and transported to your hospital by ambulance. He was reportedly found next to an abandoned downtown building. He has no wallet or any form of personal identification on his person.
Your exam reveals an unconscious casually dressed man in his 40s in no obvious discomfort, breathing regularly at a rate of 16 breaths per minute. His blood pressure, pulse, and temperature are normal. A large scalp hematoma is evident on the back of his head, with a small overlying laceration. He does not respond to verbal commands or light tactile stimuli to the limbs.
You can see that he is in a coma and quickly hypothesize that it may be related to:
myasthenic crisis
a small right cerebral hemisphere stroke
head trauma
spinal cord compression
CLUES
Coma is a problem caused by damage to or dysfunction of the brainstem or both cerebral hemispheres. The brainstem reticular activating system along with at least one of the two cerebral hemispheres is necessary to maintain consciousness. Note that the brainstem and/or both hemispheres can be indirectly affected by an expanding mass or large lesion of the cerebellum or a single cerebral hemisphere by (a) placing pressure on other areas (e.g., the brainstem or opposite cerebral hemisphere) or (b) increasing intracranial pressure.
DISCUSSION
a) Myasthenia gravis is a disorder of the NMJ. A “crisis,” as the name implies, refers to acute worsening of the disease and is considered a potential neurologic emergency because the person may lose his or her ability to breathe normally. As you recall, myasthenia causes muscle weakness without pain, sensory changes, or incontinence. Common early symptoms include eyelid ptosis, binocular diplopia (due to dysconjugate gaze), and/or nasal sounding speech. The progressive weakness that occurs when myasthenia worsens can lead to inadequate pulmonary ventilation with resultant hypoxemia. If the hypoventilation became severe enough, the hypoxemia would lead to coma and even death. However, this type of patient would exhibit respiratory distress with rapid shallow respirations with tachycardia (i.e., they wouldn’t be breathing comfortably as this patient was).
b) A small hemispheric infarct would not directly cause coma. Remember, to maintain consciousness, we need at least one cerebral hemisphere and the brainstem reticular activating system to be intact and working normally. A small isolated lesion in one cerebral hemisphere (or in the cerebellum) would not be expected to cause unconsciousness. However, a very large hemisphere or cerebellar stroke (infarct or hemorrhage) could cause coma by indirectly affecting the other areas via mass effect or increased intracranial pressure.
d) Spinal cord injury at any level would not directly lead to coma. A lesion high enough in the cervical cord could cause pulmonary hypoventilation, but the affected patient would not exhibit normal respiratory function.
c) Correct: Head trauma can definitely lead to coma (often prolonged if severe enough), and this is considered an emergency. Remember to look for evidence of cranial trauma in comatose patients. Other potential causes of coma include hypoglycemia, illicit drug use, and hypoxic-ischemic encephalopathy due to cardiac arrest. In this patient, a glucose level was immediately drawn because hypoglycemia is a common and easily treatable cause of coma. Because trauma was also suspected in his case, a brain CT scan was obtained to rule out a treatable intracranial abnormality such as epidural hemorrhage. The scan was normal, and he slowly recovered over several days. One early hypothesis was that he somehow fell from the abandoned building. Eventually, it became apparent that he was assaulted and lost his wallet and identification in the robbery.
Case Study 5: “My feet burn all the time.”
Mr. Smith is a 58-year-old florist with “burning feet.” The symptom began about a year ago in his toes and has slowly moved up to his ankles. The feeling is worse at night and better during the day when he is up and around. There is no weakness at all, and he denies any hand or upper extremity involvement. He has noticed some slight sensory loss on the soles of his feet, and they feel “like wood” when he walks without shoes.
Your exam reveals normal cranial nerve function and limb strength. Muscle stretch reflexes are symmetric and present throughout, except
for absent ankle jerks (Achilles or gastrocnemius muscle stretch reflex). Sensation is decreased distally in the feet and toes, more to pinprick and temperature than to vibration and light touch.
for absent ankle jerks (Achilles or gastrocnemius muscle stretch reflex). Sensation is decreased distally in the feet and toes, more to pinprick and temperature than to vibration and light touch.
You decide to order:
blood glucose to see if there is evidence of diabetes mellitus as a cause of peripheral polyneuropathy
lumbar spine MRI to confirm spinal stenosis
serum CK and muscle biopsy to prove inflammatory myopathy
brain CT imaging study looking for a left parietal (sensory area) stroke
DISCUSSION
b) Lumbar spinal stenosis consists of a narrowed spinal canal, usually due to degenerative changes and/or protruding intervertebral disc(s). Patients with this condition complain of lower extremity discomfort (usually in the calf and/or thigh region), especially with standing and/or ambulating. This condition is often referred to as “pseudoclaudication” because the pain worsens with ambulation. The difference is that the leg pain with true vascular claudication improves when the patient stands still to rest. With spinal stenosis, the pain does not improve and may even continue to worsen when standing still. The discomfort is presumed to be a product of multilevel nerve root/cauda equina compression, with the pain being due to either circulatory changes in or direct compression of these roots. Patients become symptomatic with standing and/or walking because the stenotic lumbar spinal canal tends to narrow more in this position due to greater lordosis. Relief can be realized with sitting or with bending over because these positions tend to open the narrowed canal slightly by decreasing the amount of lordotic curve.
c) Myopathy can be painful (especially if inflammatory in type), and the discomfort is usually proximal and aching in quality. However, weakness is the hallmark of myopathy, without sensory loss or significant changes in muscle stretch reflexes. Both of the latter were seen in this instance.
d) A parietal lobe infarct could cause contralateral hemisensory loss (i.e., sensory loss on the opposite side of the body) but
would rarely cause pain. An uncommon cause of central pain would be a small thalamic infarct (lacune), which is sometimes associated with contralateral hemisensory change and somatic discomfort. This central pain is sometimes referred to as “funicular pain.” It is typically a regional, unilateral, and difficult to define (amorphous) discomfort that is generally not position dependent.
would rarely cause pain. An uncommon cause of central pain would be a small thalamic infarct (lacune), which is sometimes associated with contralateral hemisensory change and somatic discomfort. This central pain is sometimes referred to as “funicular pain.” It is typically a regional, unilateral, and difficult to define (amorphous) discomfort that is generally not position dependent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree