Fig. 9.1
Very acute phase of intraparenchymal haemorrhage of the posterior limb of the left internal capsule (oxyhaemoglobin) occurring during a hypertensive crisis. The haematoma is hyperdense (a) on CT scan and hyperintense on the MRI FLAIR sequence (b). The site of the haematoma in the posterior limb of the internal capsule is characteristic of haematomas due to hypertensive crisis
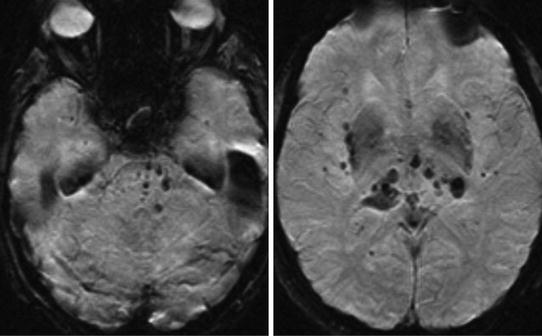
Fig. 9.2
Patient with a history of chronic hypertension. Multiple deep intraparenchymal microhaemorrhages visualized as focal hypointensities involving the brainstem and basal ganglia on T2*-weighted images
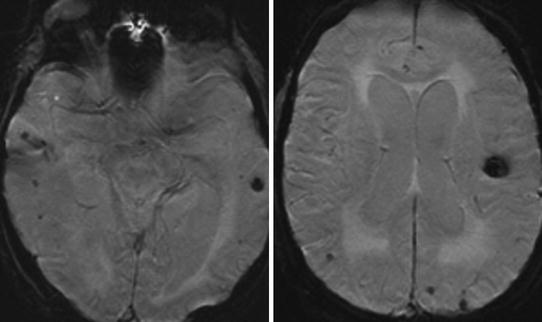
Fig. 9.3
Patient with cerebral amyloid angiopathy. Multiple peripheral cortico-subcortical intraparenchymal microhaemorrhages visualized as focal hypointensities on T2*-weighted images
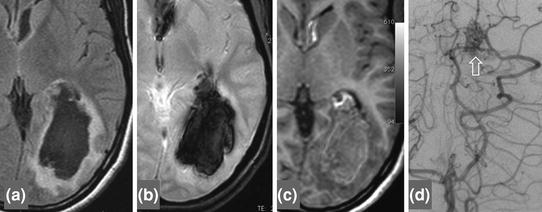
Fig. 9.4
Acute phase of left occipital intraparenchymal haemorrhage (deoxyhaemoglobin). The haematoma is hypointense with a hyperintense corona on the FLAIR sequence (a), hypointense on T2*-weighted images (b) and isointense on T1-weighted images (c). Arteriography shows an arteriovenous malformation responsible for bleeding (d hollow arrow)
Non-vascular causes: clotting disorders (leukaemia, anticoagulant or antiplatelet therapy), primary (Fig. 9.5) and secondary brain tumours.
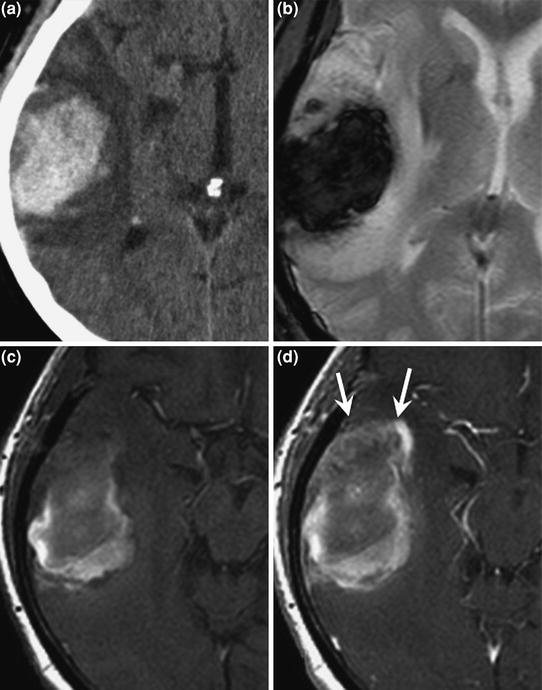
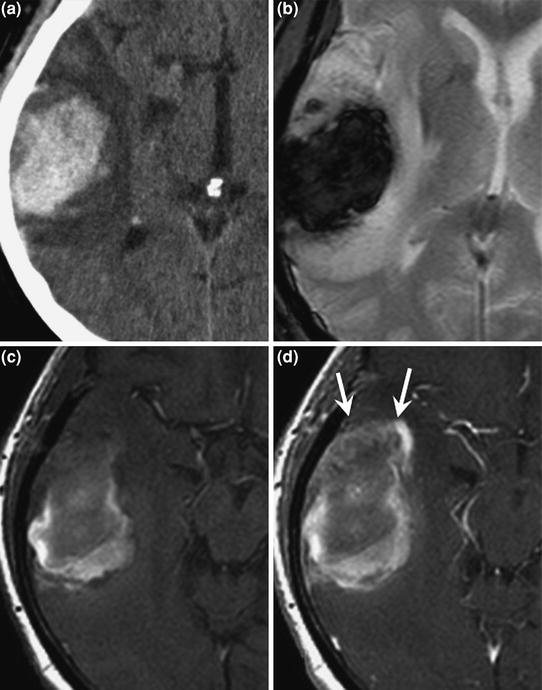
Fig. 9.5
Right temporal intraparenchymal haemorrhage secondary to brain tumour. The haematoma is hyperdense on CT scan (a), hypointense on T2*-weighted images (b) and heterogeneous (hyper- and iso-intense) on T1-weighted images (c). Note the anterior nodular contrast enhancement (d gadolinium-enhanced T1-weighted sequence, arrows), which raised the suspicion of an underlying lesion. Postoperative histological examination demonstrated glioblastoma
Aetiological Work-Up
Look for HBP (not always known before onset of haemorrhage).
Look for predisposing laboratory abnormalities:
Complete blood count, platelets, PT, APTT, thrombin time.
Systematic ECG.
Look for complications of HBP: TTE (left ventricular hypertrophy), renal function, funduscopy.
When the site of the haematoma is unusual for HBP (although haematomas associated with HBP can occur anywhere), or in the absence of HBP or multiple haematomas and when the clinical features are suggestive: investigations to detect underlying neoplasm (chest, abdomen, pelvis CT scan).
Three months after the acute episode, brain MRI must be systematically performed to detect an underlying lesion (tumour or vascular [cavernous malformation or arteriovenous malformation]) that may have been initially masked by blood or compressed by the haematoma.
Imaging
CT
Hyperdense intraparenchymal collection. Hypodensity around the lesion associated with resorption of oedema or mass effect. Usual site in basal ganglia in the case of HBP. However, the site of the haematoma is not predictive of the cause. CSF-blood fluid level (hypodense-hyperdense fluid level) in the case of intraventricular haemorrhage.
MRI
Signal varies with time (Table 9.1).
Table 9.1
CT and MRI appearance of haematomas according to the stage of haemoglobin degradation and over time
May be associated with other old haematomas visualized as hypointensity on T2-weighted gradient-echo images.
AVM: evidence of flow voids over the haematoma.
Definitive diagnosis: venous arterialization on TOF sequences. Perfusion-weighted imaging: marked increase in CBV and decreased MTT over the AVM.
Treatment
Treatment of the cause. Blood pressure control (target values during the acute phase of haemorrhage: systolic BP: 180 mmHg, diastolic BP: 90 mmHg). Anticoagulants and antiplatelet agents are contraindicated. The only exception is cerebral venous thrombosis, in which anticoagulants are the mainstay of treatment.
Meningeal Haemorrhage
Until proved otherwise, any nontraumatic meningeal haemorrhage is due to ruptured intracranial aneurysm!
When an aneurysm is discovered, always look for one or more other aneurysms (multiple aneurysms in 20 % of patients).
Subarachnoid haemorrhage between arachnoid and pia mater.
Clinical Features
Typically sudden thunderclap headache, but can be less severe and more progressive. Meningeal syndrome with neck stiffness and photophobia. Impairment of consciousness or coma. Mortality rate: 30 % in the acute phase and 50 % in the first month if haemorrhage is associated with ruptured intracranial aneurysm.
The aetiology can be suggested by the site of bleeding:
Lateral sulcus: aneurysm at the middle cerebral artery bifurcation;
Frontal interhemispheric: aneurysm of the anterior communicating artery or pericallosal artery;
Basal cistern: aneurysm of the posterior communicating artery;
Posterior fossa: aneurysm of the vertebrobasilar system;
Exclusively perimesencephalic: no known aetiology in 90 % of cases.
Aetiologies
Rupture of intracranial aneurysm (80 % of cases), often profuse haemorrhage in the lateral sulcus and basal cisterns (Fig. 9.6).
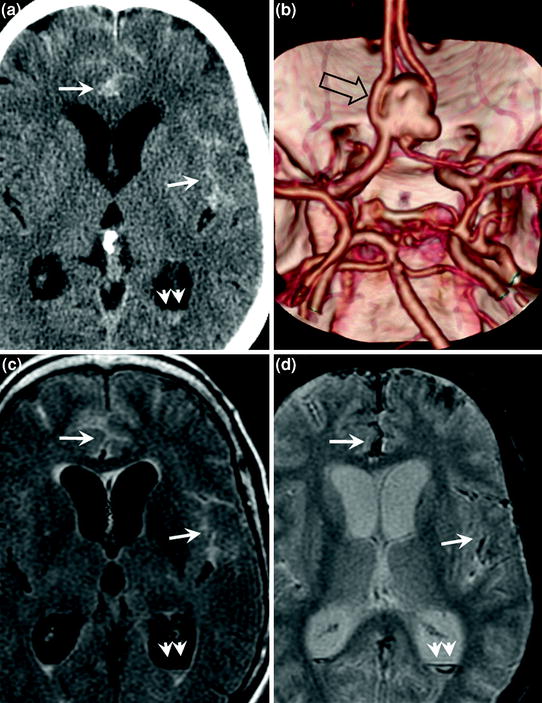
Fig. 9.6
Ruptured intracranial aneurysm with Fischer grade 4 subarachnoid meningeal haemorrhage in a 57-year-old female patient. CT visualizes the haemorrhage as hyperdensities of cortical sulci, well seen in the interhemispheric region and left lateral sulcus (a simple arrows). There is an associated intraventricular haemorrhage visualized as a fluid level in the occipital horns (a double arrows). CT angiography shows ruptured aneurysm of the anterior communicating artery (b hollow arrow). On MRI, the haemorrhage is hyperintense on the FLAIR sequence (c) and hypointense on T2*-weighted images (d)
Head injury.
Cerebral vasculitis, reversible cerebral vasoconstriction syndrome, cerebral amyloid angiopathy.
Intracranial arterial dissection.
Idiopathic (particularly in perimesencephalic haemorrhage).
When focal meningeal haemorrhage involves the convexity away from the cisterns and the lateral sulci, four main aetiologies: cerebral amyloid angiopathy (Fig. 9.7), cortical venous thrombosis, reversible cerebral vasoconstriction syndrome and cerebral vasculitis.
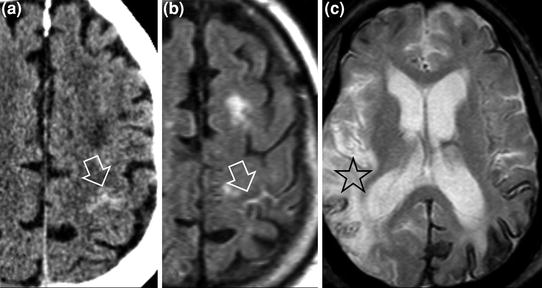
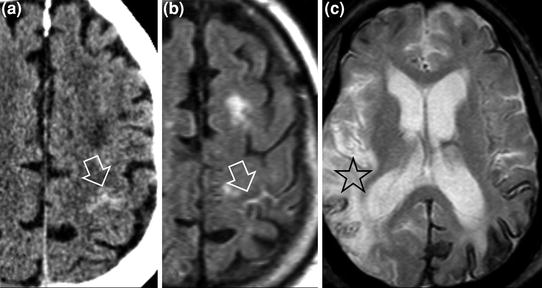
Fig. 9.7
70-year-old patient with focal meningeal haemorrhage hyperdense on CT (a hollow arrow) and hyperintense on MRI FLAIR sequence (b hollow arrow). Cognitive decline for several years, not investigated. Cerebral amyloid angiopathy was diagnosed on the basis of the clinical features and associated chronic lesions discovered on MRI: areas of cortical gliosis (c star) and diffuse superficial siderosis reflecting chronic meningeal haemorrhages visualized as cortical hypointensity on T2*-weighted images (c)
Imaging
Classification of meningeal haemorrhages due to ruptured aneurysm according to Fischer:
grade 1: haemorrhage not visible on imaging (diagnosed by lumbar puncture);
grade 2: subarachnoid haemorrhage less than 1 mm thick;
grade 3: subarachnoid haemorrhage more than 1 mm thick;
grade 4: subarachnoid haemorrhage in combination with intraparenchymal haemorrhage or intraventricular haemorrhage.
CT
CT can sometimes be normal: lumbar puncture must be performed to exclude meningeal haemorrhage.
CT is the standard procedure to detect meningeal haemorrhage.
Hyperdensity of one or more cortical sulci and/or basal cisterns.
Brain CT angiography may demonstrate an aneurysm responsible for the haemorrhage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








