18 Cerebral Revascularization for Moyamoya Disease
Moyamoya disease
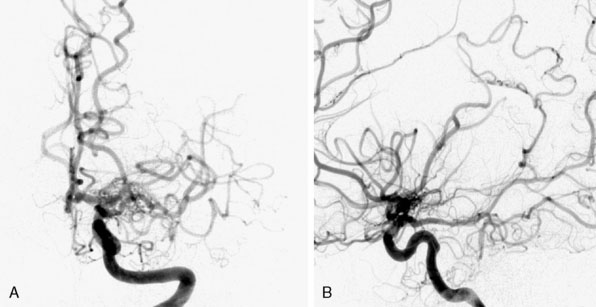
Moyamoya disease (MMD) is a rare cerebrovascular disorder characterized by idiopathic and progressive stenosis or occlusion of the supraclinoid internal carotid arteries bilaterally with frequent involvement of the bilateral anterior and middle cerebral arteries1 (Figure 18–1). The term Moyamoya meaning “a puff of smoke” in Japanese was first coined in 1969 by Suzuki and Takaku to describe the resulting characteristic abnormal vascular networks that form secondarily to the stenosis/occlusion,2 but the disease was first described in the Japanese literature in 1957 by Takeuchi and Shimizu.3 Although genetic links are implicated in MMD,4 the etiology remains unknown. Moyamoya syndrome (MMS) has similar clinical and angiographic characteristics to MMD but is associated with other conditions such as Downs syndrome, neurofibromatosis type-1 (NF-1), prior irradiation, and sickle cell disease.5 Patients with unilateral findings have MMS, although approximately 40% of these patients develop angiographic progression on the contralateral side.6 In this chapter, we will give an overview of MMD and provide a comprehensive surgical view of cerebral revascularization for MMD, emphasizing the technical nuances and complications of the procedure.
Epidemiology
Although MMD was initially described in patients of Asian descent, it recently has been increasingly reported in patients of all demographic groups, although the exact incidence is not completely known.7 Japanese studies report an annual incidence between 0.35 to 0.94/100,000 persons per year and annual prevalence between 3.16 to 10.5 per 100,000 persons.8–10 There is a bimodal distribution of age of onset with the first peak at 5 years of age and a second peak between 45 and 49 years of age. There are twice as many female patients as compared to male patients.8,9 The reported incidence and prevalence of MMD in the United States is significantly lower when compared to Japanese studies. A study of Moyamoya patients from Washington and California identified 298 individuals with MMD for an incidence of 0.086/100,000 persons per year. In a subgroup of Asian Americans, however, the incidence of 0.28/100,000 was closer to those of the Japanese studies.11 A study looking at the epidemiology of MMD in Hawaii, where the cohort was primarily of Asian descent, also revealed a higher incidence when compared to the general population in the United States.12
Presentation
Patients with MMD generally present either with hemorrhage or with ischemia. The rate of hemorrhage is approximately seven times more common in adult patients (14.6%) when compared to pediatric patients (2.1%).5,13 However, this was not true for the 432 patients treated at Stanford from 1991 to 2009, where ischemic symptoms were far more common than hemorrhage.13 Some have suggested that the hemorrhage rate is higher in Asians.14–17 Occasionally patients may also present with seizure, headaches, or behavioral changes. Some studies suggest a relation between headaches and hypoperfusion leading to cortical depression and associated migraine symptoms.18 Others have suggested that dilation of dural and meningeal vessels irritate the pain fibers on the dura, resulting in a migraine-like headache that is refractive to medical therapies.19 This headache initially persisted in 63% of patients even after cerebral revascularization, although it would often improve over time.
Pathophysiology
On histopathologic examination, the internal carotid arteries demonstrate eccentric fibrocellular thickening of the intimal layer, proliferation of smooth muscle cells, and tortuous and often duplicated internal elastic lamina with no inflammatory or atheromatous involvement, resulting in artery stenosis/occlusion.4 The resulting hypoxia induces collateralization through formation of dilated and tortuous perforating arteries. These “Moyamoya” vessels have thinned media with fibrin deposition in the vessel walls, fragmented elastic lamina, and microaneurysm formation that may be secondary to increased expression of numerous growth factors, including hypoxia-inducible factor 1 (HIF-1), vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), transforming growth factor-beta (TGF-beta), hepatocyte growth factor (HGF), and matrix metalloproteinases (MMPs).4
Genetic factors play a role as up to 15% of MMD patients are familial indicating an autosomal dominant inheritance pattern with incomplete penetrance. A number of genome-wide studies from these familial carriers of MMD suggest links to chromosomal regions including 3p24.2-p26,20 6q25,21 8q23,22 12p12,22 and 17q25.23 Recently, carriers of a mutation in the vascular smooth muscle cell (SMC)–specific isoform of alpha-actin (ACTA2) were found to present with a variety of vascular diseases including premature onset of coronary artery disease, non-Marfan’s thoracic artery aneurysms and dissections, non-MMD early onset stroke, and MMD.24
Natural history and prognosis
There are limited studies on the natural history of MMD, but each of the studies has demonstrated inevitable disease progression if left untreated.6,25,26 In one study, the 5-year cumulative risk of any recurrent ipsilateral stroke in patients treated without surgery with impaired hemodynamic reserve, as measured by increased oxygen extraction fraction on positron emission tomography (PET), was approximately 65%. In patients with bilateral disease, the stroke risk over 5 years was 82%.14 Another North American study found a recurrent stroke rate of 18% in the first year and a 5% per year risk in subsequent years.17 A nationwide survey in Japan of asymptomatic Moyamoya patients found a 3.2% per year stroke rate in medically treated patients.27 In contrast, the estimated rate of perioperative or subsequent stroke or death after surgical revascularization was between 5.5%13 and 17%14 over 5 years, demonstrating the need for surgical treatment of these patients.
Diagnoses and treatment
The diagnoses of MMD or MMS should be considered in any patient, especially in a child or young adult who presents with neurologic deficits or symptoms secondary to cerebral ischemia or hemorrhage. Radiologic evaluation can include CT, MRI, cerebral angiography, and cerebral perfusion studies, including CT perfusion, xenon-enhanced CT, or PET, MR perfusion, and SPECT or CT imaging without and with acetazolomide challenge. Cerebral angiography, CT angiography, and MR angiography imaging can reveal intracerebral vascular occlusion along with the resulting Moyamoya vessels. CT and MRI can reveal hemorrhage or ischemic changes. Cerebral perfusion studies help to characterize blood flow and elucidate the hemodynamic state preoperatively and postoperatively.28
Although there are no randomized studies comparing medical treatment versus surgical revascularization for patients with MMD, we believe that the stroke rate is significantly reduced in surgically treated patients. As discussed in the previous section, the natural history of these patients is to progress and the risk of recurrent stroke is extremely high with medical management only. The main medical treatment option for these patients is antiplatelet therapy. All patients are on aspirin pre- and postoperatively. Full anticoagulation drugs such as warfarin are rarely used.5
Patients with MMD have occlusion of the internal carotid arteries with sparing of the external carotid system. Surgical treatment uses the external carotid system to supply blood to the ischemic cerebrum by either creating a “direct” or an “indirect” revascularization bypass. A direct bypass involves dissection of a branch of the external carotid artery, specifically the superficial temporal artery (STA), which is then directly anastomosed to a distal (usually M4) cortical branch of the middle cerebral artery (MCA). An indirect bypass is performed by placement of vascularized tissue supplied by the external carotid (such as dura, the temporalis muscle, or the STA itself) onto the cortical surface of the brain leading to an ingrowth of new blood vessels to the cortex beneath it. There are no randomized studies comparing the efficacy and safety of indirect versus direct bypass, and a review of the literature failed to reveal a difference in surgical morbidity or stroke rate (perioperative or long term) between methods.29 Many institutions will perform direct revascularization for adults and indirect revascularization for children because of the smaller and more friable caliber of the vessels in children.30,31 However, there are many groups that perform indirect bypass for adult patients as well.14,17,32 Our philosophy is to perform direct bypass on all patients unless the STA or MCA is too small or friable. Direct revascularization procedures have the advantage of providing immediate increase in blood flow to the ischemic cortex. In bilateral MMD, we first revascularize the symptomatic hemisphere. If there are no lateralizing signs or symptoms, we prefer to revascularize the non-dominant hemisphere because of increased incidence of transient neurologic symptoms after surgery on the dominant hemisphere. The contralateral side is generally revascularized 1 week after the first side unless there were significant complications after the first procedure.