7 Cerebral Sinus Thrombosis Isabel Fragata and Aman Patel Thrombosis of cerebral veins and dural sinuses is an uncommon clinical entity, representing less than 1% of all stroke cases in adults. Cerebral sinus venous thrombosis (CVT) is more common in neonates and children than in adults; among adults, it is more common in women.1 The mean age of onset is 39 years, and 75% of cases involve multiple veins and/or sinuses.1 Obstruction of cerebral venous drainage can lead to increased venous and capillary pressure with subsequent blood-brain barrier breakdown and vasogenic cerebral edema, venous hemorrhage, and/or ischemia or cytotoxic edema. Cerebrospinal fluid (CSF) absorption is also impaired, further contributing to elevated intracranial pressure (ICP). Elevated ICP is most common with superior sagittal sinus obstruction, but it can occur with jugular or transverse sinus thrombosis. A high index of clinical suspicion and neuroimaging techniques are the key to diagnosis.2
History and Examination
History
Physical and Neurologic Examination
| Location of CVT | Frequency% | Presenting Symptoms |
| Superior sagittal sinus | 62 | Motor deficits (predominantly affecting lower limbs); possible bilateral deficits Seizures Psychiatric symptoms |
| Transverse sinus | 86 | Intracranial hypertension, aphasia when left transverse sinus occluded |
| Cerebral cortical vein | 17 | Motor/sensory deficits according to territory Focal seizures |
| Deep venous system | 11 | Coma, alteration of mental status Bilateral motor deficits |
| Cavernous sinus | Rare | III, IV, V1, V2, or VI nerve palsy Orbital pain, chemosis, proptosis |
Frequency column data from: Ferro JM, Canhão P, Stam J, et al. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004;35(3):664–670.
Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005;352(17):1791–1798.
Differential Diagnosis
- Cerebral sinus thrombosis. The most common causes are pregnancy and puerperium, oral contraceptives, local infections, and thrombophilia. Most often CVT is multifactorial: more than one cause can be found in 44% of patients. In 15% of patients, no inciting cause is found1 (Table 7.2).
Table 7.2 Common Causes of Cerebral Sinus Thrombosis
Category
Causes
Hypercoagulable state (most common etiology found in 34% of patients)
Protein C, S, or antithrombin III deficiency; factor V Leiden mutation; prothrombin gene mutation; antiphospholipid syndrome (lupus anticoagulant/anticardiolipin antibody); nephrotic syndrome; hyperhomocysteinemia
Infectious (found in 10% of patients)
Encephalitis; cerebritis; meningitis; mastoiditis; otitis; sinusitis; mouth, face, and neck infections
Obstetric
Pregnancy and puerperium
Malignancy
CNS tumors with invasion of the venous sinus, hematologic cancers, hypercoagulable state due to malignancy
Inflammatory diseases
Vasculitis, lupus, Wegener’s granulomatosis, inflammatory bowel disease (Crohn’s and ulcerative colitis), Behçet’s disease, thromboangiitis obliterans, sarcoidosis
Hematologic diseases
Polycythemia, thrombocythemia, paroxysmal nocturnal hemoglobinuria
Drugs
Oral contraceptives (particularly when combined with tobacco use or prothrombotic disease), hormone replacement therapy, asparaginase, tamoxifen, steroids, androgens
Trauma (including iatrogenic)
Head injury, lumbar puncture, neurosurgical procedures, jugular catheter occlusion
Other
Dehydration, congenital heart disease, thyroid disease
Abbreviation: CNS, central nervous system.
- Dural arteriovenous fistula (DAVF). DAVFs are characterized by a direct connection between meningeal arteries and dural venous sinuses or meningeal veins. DAVFs can be associated with sinus thrombosis or trauma. They are classified as type I—dural arterial supply drains anterograde into venous sinus; type II—dural arterial supply drains into the venous sinus, but high pressure in the sinus results in both anterograde drainage and retrograde drainage into subarachnoid veins; and type III—dural arterial supply drains retrograde into subarachnoid veins. Subarachnoid veins can form varices and aneurysms and are prone to rupture. Both type II and III DAVF should be treated endovascularly or surgically to prevent hemorrhage.4
- Stroke (ischemic or hemorrhagic) can present with acute deficits and seizures. Headache and mental status changes are more common with hemorrhagic stroke (ICH, SAH). Venous infarct and ICH can both be caused by sinus thrombosis.
- Brain tumor. A brain tumor can occasionally have strokelike sudden presentation or present with seizure, headache, and/or evidence of elevated ICP.
- Encephalitis/cerebritis/abscess. Look for signs of infection, including fever, elevated white blood cell count (WBC), and lumbar puncture results. Sinus thrombosis may accompany these infections.
- Benign intracranial hypertension (pseudotumor cerebri). This can present with headache and VI nerve palsy, but encephalopathy, focal deficits, and seizure are atypical and should prompt a more thorough evaluation. Patients with suspected pseudotumor cerebri should undergo MR or CT venography (MRV or CTV) imaging to rule out sinus thrombosis.
- Stroke (ischemic or hemorrhagic) can present with acute deficits and seizures. Headache and mental status changes are more common with hemorrhagic stroke (ICH, SAH). Venous infarct and ICH can both be caused by sinus thrombosis.
Life-Threatening Diagnoses Not to Miss
- Cerebral sinus thrombosis. Expedient treatment can prevent intracranial hemorrhage.
- Encephalitis/cerebritis/abscess requires urgent antibiotic administration.
- Any process that causes dangerous elevations in ICP should be diagnosed and managed immediately.
Diagnostic Evaluation
- Imaging studies
- Head CT:
- Can be normal in up to 30% of CVT cases5
- Noncontrast CT: The cord sign (present in 25% of cases, represents a spontaneously hyperdense thrombosed cortical vein), dense triangle sign (hyperdense torcular and/or posterior superior sagittal sinus)
- Postcontrast CT: The empty delta sign (present in 16 to 46% of cases, represents lack of filling of the torcular and/or the posterior superior sagittal sinus)
- Indirect/nonspecific signs of CVT include brain edema, hemorrhagic lesions, gyral enhancement, intense contrast enhancement of the falx, and tentorium.
- CT also helps detect local infectious causes of CVT (otitis, mastoiditis, sinusitis).
- Can be normal in up to 30% of CVT cases5
- CTV: (CT venography)
- Increasingly and reliably used to diagnose CVT, with a reported sensitivity of 95% when compared with digital subtraction angiography (DSA)6
- Fast alternative to magnetic resonance imaging (MRI), especially in patients with pacemakers or ferromagnetic implants. CTV is not subject to flow-related artifacts and pitfalls in interpretation as is MRI.
- Increasingly and reliably used to diagnose CVT, with a reported sensitivity of 95% when compared with digital subtraction angiography (DSA)6
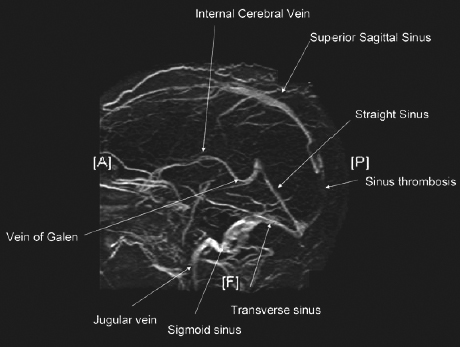
- MRI and MRV: (MR venography)
- Extremely sensitive for diagnosis and follow-up of CVT (Fig. 7.1)

Stay updated, free articles. Join our Telegram channel
- Extremely sensitive for diagnosis and follow-up of CVT (Fig. 7.1)
- Head CT:

Full access? Get Clinical Tree








