♦ Preoperative
Operative Planning
- Review appropriate imaging including anteroposterior, lateral, and flexion-extension x-rays, magnetic resonance imaging (MRI), computed tomography scan of the cervical spine
- Choose arthroplasty device (two are currently approved by the US Food and Drug Administration for single level placement)
- PRESTIGE ST (Sofamor Danek)
- Stainless steel, ball-and-trough design
- Vertebral body screws used to fix the position in the interspace
- Semiconstrained
- Stainless steel, ball-and-trough design
- PRODISC-C (Synthes, West Chester, PA)
- Two cobalt chrome alloy endplates and an ultra-high molecular weight polyethylene inlay in a ball-and-socket configuration
- Central keel for primary fixation
- Semiconstrained
- Two cobalt chrome alloy endplates and an ultra-high molecular weight polyethylene inlay in a ball-and-socket configuration
- PRESTIGE ST (Sofamor Danek)
- Patient counseling
- Discuss risks of implant failure, new or residual radiculopathy, migration, subsidence, and reoperation
- Discuss alternatives including fusion or other motion-sparing procedures such as posterior foraminotomy
- Discuss MRI compatibility
- Discuss risks of implant failure, new or residual radiculopathy, migration, subsidence, and reoperation
- See Chapter 94, Anterior Cervical Discectomy/Foraminotomy, as indicated.
- Artificial disc implant system (choices listed previously)
- To maximize ergonomics, right-handed surgeons may be positioned to the patient’s right.
- Endotracheal tube should then be placed to the left corner of the patient’s mouth.
- The C-arm fluoroscope is positioned to obtain cross-table lateral cervical x-ray views.
Anesthetic Issues
- One to two grams of cefazolin are given preoperatively depending on patient weight (or other appropriate antibiotic of choice).
- Dexamethasone may be given before surgery, although it is not mandatory.
- Intraoperative neuromonitoring with somatosensory evoked potentials and/or electromyelography is optional.
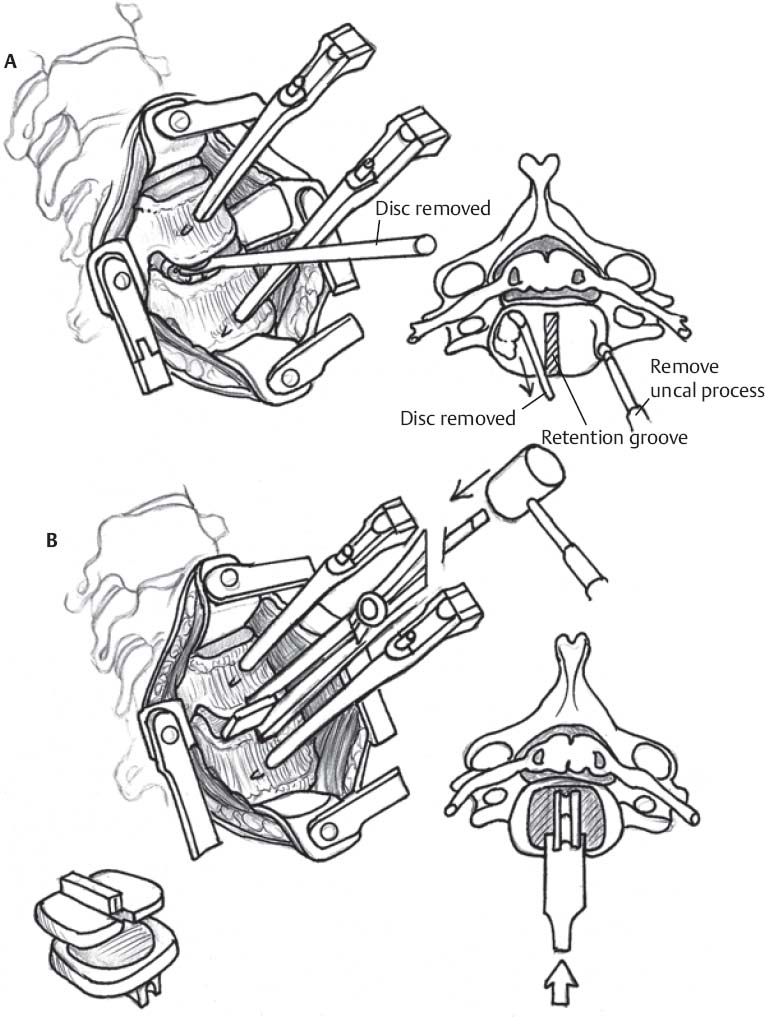
Intraoperative (Fig. 99.1)
Positioning and Exposure
- See Chapter 94, Anterior Cervical Discectomy/Foraminotomy, as indicated.
- Position the patient supine with the neck supported dorsally with a roll.
- The neck should be in a neutral or mildly lordotic position for device placement.
- The shoulders are retracted caudally to help with intraoperative fluoroscopic visualization.
- Visualization is important for precise placement of the arthroplasty device.
- The patient’s body habitus should be taken into consideration prior to the procedure.
- Visualization is important for precise placement of the arthroplasty device.
- A transverse right-sided skin incision is made through a preexisting skin crease.
- After exposure, a lateral, localizing fluoroscopic x-ray is used to confirm all operative levels.
- A self retaining anterior cervical retractor is placed under the elevated edges of the longus colli muscles.
- Anteroposterior fluoroscopic x-ray can be used to confirm midline.
Discectomy and Endplate Preparation
- Vertebral body distraction pins may be placed to enlarge the disc space. Placement of these pins can be useful in marking the midline.
- The entire visible disc is removed from the endplates exposing the posterior longitudinal ligament (PLL).
- The PLL is also removed.
- With significant spondylotic changes, a power drill may be used to remove the disc and osteophytes.
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree