Chapter 232 Cervical Disc Herniation with Radiculopathy
Anterior Cervical Discectomy with Interbody Fusion
Anterior cervical discectomy and fusion (ACDF) is a common and accepted treatment for the patient with cervical disc herniation with radiculopathy. Successful results have been reported since the original descriptions of the operative techniques of Smith and Robinson1 and Bailey and Badgley2 and the refined techniques and instruments developed by Cloward.3,4 Although single-level ACDF has a generally high fusion rate by several techniques, argument continues as to the added benefit of plating for treatment of single-level disease. Proponents of plating cite reduction in interbody graft migration, diminished rates of pseudarthrosis, improved immediate postoperative segmental rigidity, reduction in kyphotic angulation, and the lack of need for cervical orthosis.
Case for Fusion without Plating
Satisfactory Clinical Outcomes without Plating
Samartzis et al.5 demonstrated an increased fusion rate in noninstrumented patients (100%) using autologous iliac crest compared to patients undergoing ventral plating (90.3%), though the finding was noted not to be statistically significant. Cervical plating may theoretically produce detrimental stress shielding of the segment that is intended to undergo arthrodesis. Distractive forces imparted by a rigid plate-screw construct may reduce desirable compressive stress at the graft–end-plate interface and could contribute to delayed fusion and pseudarthrosis.6–8
Epstein9 reviewed her series of 178 patients undergoing ACDF with autograft iliac crest bone grafting. Dynamic radiographs and computed tomography showed fusion or pseudarthrosis without motion in 99% of patients undergoing single-level surgery.
Use of autologous iliac crest, once considered the gold standard for interbody fusion material, is known to carry significant graft site complications. In light of this, many surgeons have turned to the use of allogeneic bone sources and have employed cervical instrumentation as a means to augment fusion rates out of concern for increased risk of pseudarthrosis. However, multiple reports indicate favorable radiographic and clinical outcomes with allogeneic grafting material independent of the presence of fixation. Martin et al.10 reviewed 317 cases of ACDF surgery using freeze-dried fibular allograft without ventral plating. They reported a 90% fusion rate in single-level surgeries in a population of which more than 25% were habitual smokers.
Jagannathan et al.11 reviewed 170 patients undergoing single-level ACDF using a modified Cloward technique with freeze-dried allograft. Rigid cervical orthosis was not utilized, though patients were offered soft cervical collars for comfort. They reported a 94% fusion rate and 96% of patients demonstrating favorable neurologic outcomes.
Matz et al.12 recently performed an excellent evidence-based review of the current literature with regard to various techniques for the treatment of anterior cervical nerve root compression. They identified 17 prior studies that compared ACDF with and without fixation and concluded that the addition of an anterior cervical plate did not improve long-term clinical outcomes but may reduce pseudarthrosis rates and graft-related problems.
Increased Cost Associated with Fixation
In today’s ever cost-conscious health-care climate, the added expense of cervical instrumentation cannot be completely ignored. Angevine et al.13 performed a retrospective cost analysis with regard to the addition of an anterior cervical plate following ACDF with allograft. Outcome in this cost-effectiveness analysis was measured in quality-adjusted life-years (QuaLYs). The improvement in quality of life following ACDF surgery with allograft alone came at a cost of $496 per QuaLY. The additional gains following ACDF with plating increase the cost to $32,560 per QuaLY.
Branch has previously reported on the increased cost of ACDF with plating versus ACDF alone.14 Sources of increased cost include increased operating time required for placement of fixation, surgical fees, and charges for hardware costs. The hospital charges for single-level ACDF with plating were approximately $3123 higher than charges for similar cases without internal fixation.
A recent European study examined the cost effectiveness of various surgical treatments of single-level cervical radiculopathy.15 Patients were allotted to one or four groups: cage only, autograft and plating, cage with allograft particles and plating, and disc arthroplasty. All groups had similar improvements in neck and arm pain scores, and all patients who underwent fusion procedures demonstrated radiographic evidence of fusion at 1 year. The average total cost was least in the cage-only group (≤1930), which was the most cost-effective treatment option for single-level ACDF.
Alternatives to Ventral Cervical Plating
Anchored Interbody Spacers
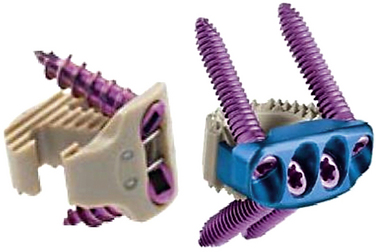
Several recent devices have come to market that share the properties of being a low-profile interbody spacer that allows for fixation to the adjacent vertebral bodies without a formal anterior cervical plate (Fig. 232-1). The polyetheretherketone (PEEK) Prevail cervical interbody device (Medtronic Sofamor Danek, Memphis, TN) is an interbody device with rostral and caudal midline flanges that allow for a screw interface with the ventral corner of the adjacent vertebral body. The device utilizes nitinol wires as a locking mechanism to prevent screw backout.
The Zero-P device (Synthes, West Chester, PA) has similar properties but does not require preparation of the anterior surface of the vertebral body. This “anchored spacer” consists of a polyetheretherketone interbody cage with a ventral titanium housing that allows for anchoring screws to be placed diagonally into the adjacent vertebral bodies. Scholz et al.16 recently examined the biomechanical properties of this stand-alone cervical interbody device. This device demonstrated decreased range of motion compared to interbody cage alone (no fixation) and no significant difference when compared to the addition of a locking or dynamic anterior cervical plate.
Cervical Total Disc Arthroplasty
In the absence of significant coexisting cervical disc disease at other levels, total disc arthroplasty is another option for treatment of cervical disc herniation with radiculopathy. Mummaneni et al.17 recently presented the 3- to 5-year results of a prospective randomized trial of ACDFP versus arthroplasty with the Prestige device (Medtronic Sofamor Danek). Of 541 patients included in the study, 276 underwent discectomy and disc arthroplasty. Neck disability index and neck pain scores were significantly better in the arthroplasty group at 3 years but were similar to the ACDFP group at 5 years. The arthroplasty devices maintained a mean of 7.1 degrees of flexion-extension motion, and the arthroplasty group had fewer secondary surgeries than did the ACDFP group.
Angevine P.D., Zivin J.G., McCormick P.C. Cost-effectiveness of single-level anterior cervical discectomy and fusion for cervical spondylosis. Spine (Phila Pa 1976). 2005;340:1989-1997.
Branch C.L.Jr. Anterior cervical fusion: the case for fusion without plating. Clin Neurosurg. 1999;45:22-24.
Jagannathan J., Shaffrey C.I., Oskouian R.J., et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008;8:420-428.
Matz P.G., Ryken T.C., Groff M.W., et al. Techniques for anterior cervical decompression for radiculopathy. J Neurosurg Spine. 2009;11:183-197.
Mummaneni PV, Haid RW Jr., Traynelis VC, et al. 3-year and 5-year follow up from the prospective randomized US FDA IDE trial of the Prestige cervical disc arthroplasty. Presented at the 25th Annual Meeting of the AANS/CNS Section on Disorders of the Spine and Peripheral Nerves. March 11–14, 2009. Phoenix, AZ.
Schloz M., Reyes P.M., Schleicher P., et al. A new stand-alone cervical anterior interbody fusion device. Biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976). 2009;34:156-160.
1. Smith G.W., Robinson R.A. The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg [Am]. 1958;40:607-624.
2. Bailey R.Q., Badgley C.E. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg [Am]. 1960;42:565-594.
3. Cloward R.B. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602-617.
4. Cloward R.B. The anterior surgical approach to the cervical spine: the Cloward Procedure: past, present, and future. The presidential guest lecture, Cervical Spine Research Society. Spine. 1988;13:823-827.
5. Samartzis D., Shen F.H., Lyon C., et al. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J. 2004;4:636-643.
6. Wang J.C., McDonough P.W., Endow K.K., et al. The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord. 1999;12:467-471.
7. Shapiro S. Banked fibula and the locking anterior cervical plate in anterior cervical fusion following cervical discectomy. J Neurosurg. 1996;84:161-165.
8. Capen D, Rah A, Nagelberg S, et al. Clinical significance of instrumented versus noninstrumented anterior cervical discectomy and fusion. Paper presented at the Annual Meeting of the North American Spine Society; October 25, 1997; New York.
9. Epstein N.E. Anterior cervical discectomy and fusion without plate instrumentation in 178 patients. J Spinal Disord. 2000;13:1-8.
10. Martin G.J., Haid R.Q., MacMillan M., et al. Anterior cervical discectomy with freeze-dried allograft. Overview of 317 cases and literature review. Spine (Phila Pa 1976). 1999;24:852-859.
11. Jagannathan J., Shaffrey C.I., Oskouian R.J., et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008;8:420-428.
12. Matz P.G., Ryken T.C., Groff M.W., et al. Techniques for anterior cervical decompression for radiculopathy. J Neurosurg Spine. 2009;11:183-197.
13. Angevine P.D., Zivin J.G., McCormick P.C. Cost-effectiveness of single-level anterior cervical discectomy and fusion for cervical spondylosis. Spine (Phila Pa 1976). 2005;340:1989-1997.
14. Branch C.L.Jr. Anterior cervical fusion: the case for fusion without plating. Clin Neurosurg. 1999;45:22-24.
15. Bhadra A.K., Raman A.S., Casey A.T.H., et al. Single-level cervical radiculopathy: clinical outcome and cost-effectiveness of four techniques of anterior cervical discectomy and fusion and disc arthroplasty. Eur Spine J. 2009;18:232-237.
16. Schloz M., Reyes P.M., Schleicher P., et al. A new stand-alone cervical anterior interbody fusion device. Biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976). 2009;34:156-160.
17. Mummaneni PV, Haid RW Jr, Traynelis VC, et al. 3-year and 5-year follow up from the prospective randomized US FDA IDE trial of the Prestige cervical disc arthroplasty. Presented at the 25th Annual Meeting of the AANS/CNS Section on Disorders of the Spine and Peripheral Nerves. March 11–14, 2009. Phoenix, AZ.
Anterior Cervical Discectomy with Interbody Fusion with Plating
Anterior cervical discectomy with interbody fusion (ACDF) is a very common surgical procedure that can be used to treat multiple cervical pathologies. ACDF surgery is commonly used to treat radiculopathy and myelopathy due to degenerative cervical disease. ACDF was initially done without instrumentation and demonstrated very good results in treating radiculopathy and myelopathy.1 However, pseudarthrosis and graft extrusion are known complications of ACDF.2 To address these complications, plating was added to ACDF, as first described by Bohler and Gaudermak in 1964.3
Description of Procedure
The following is a description of our technique for ACDF.
The patient is placed supine on the operating room table. Once the anesthesiologist’s endotracheal tube and lines and are appropriately secured, the patient’s head should be placed in a neutral position or in slight extension. This can be done with a small shoulder roll or by dropping the head of the table. The head can be placed on a donut to secure it in position or in traction if desired. The shoulders should be pulled down toward the feet either with tape or with wrist straps if necessary to visualize the lower cervical levels. To avoid injury to the brachial plexus, care should be taken not to pull too tightly. Electrophysiologic monitoring can be used to minimize the risk for iatrogenic injury due to positioning, decompression, and instrumenting as desired by the primary surgeon.4
External landmarks can be used to estimate cervical spine levels, which should then be confirmed with fluoroscopy. The hyoid bone is close to the C2-3 interspace. The top of the thyroid cartilage is close to C3-4, while the inferior border can be estimated as C4-5. The cricoid ring is roughly at the C5-6 level. One finger breadth above the clavicle is estimated as C7-T1.5
The neck is then prepped and draped in the usual sterile fashion. A transverse incision over the level of interest should be adequate for most surgical exposures, though if a particularly long ventral construct is being performed, then a longitudinal incision along the medial border of the sternocleidomastoid muscle provides greater exposure.6
The transverse incision should be just off midline and extend laterally to the sternocleidomastoid. The incision is normally performed on the left side to reduce the risk of injury to the recurrent laryngeal nerve, though it is unclear whether this actually reduces the risk.7 The skin is opened with a knife, exposing the platysma. The platysma is then divided and undermined. After the sternocleidomastoid (SCM) has been identified and the carotid has been palpated, a plane medial to SCM and carotid sheath and lateral to the trachea and esophagus should be identified. With the use of blunt dissection, this avascular plane is followed down to prevertebral fascia. The omohyoid muscle may obstruct this approach at the C5 level and can be divided without significant consequences (Fig. 232-2).
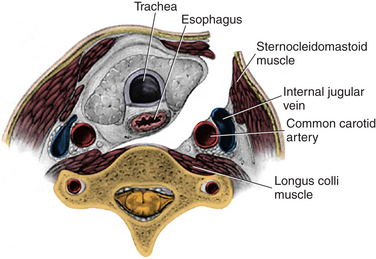
FIGURE 232-2 The corridor for anterior cervical discectomy and fusion approaches.
(Used with permission from Barrow Neurological Institute.)
By using cautery, the longus colli muscles are then detached medially to laterally, and the retractor system can be placed. Placement of the retraction blades on the longus colli muscles is important to reduce risk of injury to the underlying carotid and esophagus. One theory about injury to the recurrent laryngeal nerve is that it is a compressive injury of the endolaryngeal segment of the nerve between the retractor and the endotracheal tube rather than a direct dissection injury. Apfelbaum et al. reported that if the endotracheal tube cuff was deflated after the retractor blades were placed and was then reinflated, their rate of injury went from 6.4% to 1.7%.8
The graft is then inserted into the disc space. Autograft or allograft can be used. Autograft has a slightly higher fusion rate, quoted as being between 83% and 97%, but there is the risk for donor site complications, and the allograft fusion rate of 82% to 94% is nearly as good.9 The graft is slightly oversized and the vertebral bodies are slightly distracted so that the graft is under compression, which helps with fusion. Distracting the vertebral bodies can be done with distractor pins, gentle cervical traction, or disc spacers. Care is taken not to oversize the graft so that the vertebral bodies are not overdistracted. Once the graft is in place, the distraction force is removed, and a radiograph is taken to evaluate alignment and graft position.
The plate should be placed in the midline—straight up and down. Unicortical screws are often used. The screws should be toed in, or directed medially in the horizontal direction, and toed out, or directed away from the graft, in the vertical direction to help reduce pull-out. The screws should not violate the end plate, as this will predispose the patient to adjacent-segment disease (Fig. 232-3).
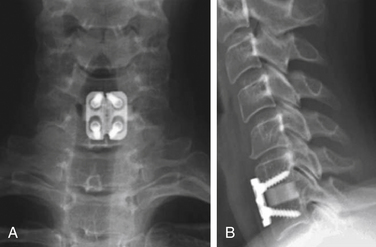
FIGURE 232-3 Anteroposterior (A) and lateral (B) views of instrumented anterior cervical discectomy and fusion.
(From Rhee JM, Riew KD: Dynamic anterior cervical plates. J Am Acad Orthop Surg 15:640–646, 2007.)
Complications
ACDF surgery has been shown to have a great deal of success in treating cervical radiculopathy, but there are some well-known complications. One study quoted the following complication rate: recurrent laryngeal nerve palsy, 3.1%; postoperative dysphagia, 9.5%; postoperative hematoma, 5.6%; dural perforation, 0.5%; esophageal perforation, 0.3%; wound infection, 0.1%; and hardware failure, 0.1%.10 With knowledge of these complications, care can be taken to avoid them.
Plate versus Uninstrumented
The act of placing a plate in ACDF adds to operative time, cost, and blood loss. Many studies show that patients get an excellent fusion in single-level ACDF without instrumentation. Fuse rates for single-level surgery have been quoted as being greater than 90% with or without plating.11 However, plating is recommended in patients who are having an operation on multiple levels, as the pseudarthrosis rate is significantly higher in noninstrumented patients. A study by Wang et al. shows a pseudarthrosis rate of 25% in two-level ACDF patients without instrumentation and no pseudarthrosis in patients with plating.12 Also, some patients are unable to wear hard collars; by placing the plate over the graft and screwing it into the vertebral body, the orthosis is moved interiorly so that collars or halos are often not required.
Dynamic versus Fixed
During the last 20 years, there have been many developments in the design of the plating systems. The different plating systems have different retractors and distractors but, most important, different screw plate interfaces. The major choice in selection of the plate system is whether a dynamic or fixed system is chosen. In a fixed system, the screw-plate interface is constrained. This provides for a more stable construct, but it also stress-shields the graft and diminishes load sharing between plate and bone graft. Grafts are best incorporated into constructs when they are subjected to compressive forces. This can be achieved by oversizing the graft and distracting the vertebral bodies, but a fixed anterior cervical plate will still shield the graft from the normal daily compressive forces that help bones to remodel (Fig. 232-4).
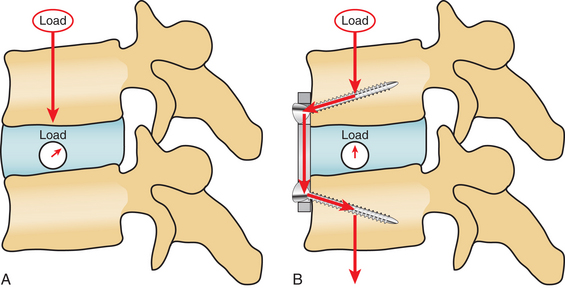
FIGURE 232-4 Biomechanical differences of force vectors in the uninstrumented (A) and instrumented (B).
(From Rhee JM, Riew KD: Dynamic anterior cervical plates. J Am Acad Orthop Surg 15:640–646, 2007.)
Dynamic plating systems allow movement at the screw-plate interface. This may decrease the rigidity of the construct, but it allows compressive forces to run through the graft. In theory, this should help to promote fusion. However, several studies comparing the fusion rate between dynamic and fixed plate systems show similar fusion rates. One study demonstrated slightly better outcomes from a pain perspective with the dynamic plates,13 but in general, the few studies that have been completed showed minimal difference between fixed and dynamic plates.14
Bartolomei J., Sonntag V. Anterior approach including cervical corpectomy. In Youmans J., editor: Neurological surgery, ed 5, Philadelphia: WB Saunders, 2004.
Fountas K.N. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32:2310-2317.
Kilburg C., Sullivan H.G., Mathiason M.A. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine. 2006;4:273-277.
Kim S.H., Sebastian C.T., Nathan D.J., et al. Operative techniques: anterior cervical decompression, fusion, and instrumentation. In: Kim D.H., Ludwig S.C., Vaccaro A.R., editors. Atlas of spine trauma: adult and pediatric. Philadelphia: WB Saunders, 2008.
Rhee J.M., Riew K.D. Dynamic anterior cervical plates. J Am Acad Orthop Surg. 2007;15:640-646.
Smith G.W., Robinson R.A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg [Am]. 1958;40:607-624.
1. Smith G.W., Robinson R.A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg [Am]. 1958;40:607-624.
2. Connolly P.J., Esses S.I., Kostuik J.P. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996;9:202-206.
3. Bohler J., Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma. 1980;20:203-205.
4. Slimp J.C. Electrophysiologic intraoperative monitoring for spine procedures. Phys Med Rehabil Clin North Am.. 2004;15:85-105.
5. Bartolomei J., Sonntag V. Anterior approach including cervical corpectomy. In Youmans J., editor: Neurological surgery, ed 5, Philadelphia: WB Saunders, 2004.
6. Kim S.H., Sebastian C.T., Nathan D.J., et al. Operative techniques: anterior cervical decompression, fusion, and instrumentation. In: Kim D.H., Ludwig S.C., Vaccaro A.R., editors. Atlas of spine trauma: adult and pediatric. Philadelphia: WB Saunders, 2008.
7. Kilburg C., Sullivan H.G., Mathiason M.A. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine. 2006;4:273-277.
8. Apfelbaum R.I., Kriskovich M.D., Haller J.R. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976). 2000;25:2906-2912.
9. Samartzis D. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J. 2003;3:451-459.
10. Fountas K.N. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32:2310-2317.
11. Samartzis D., Shen F.H., Lyon C., et al. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J. 2004;4:636-643.
12. Wang J.C., McDonough P., Endow K., et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2000;25:41-45.
13. Saphier P.S., Arginteanu M.S., Moore F.M., et al. Stress-shielding compared with load-sharing anterior cervical plate fixation: a clinical and radiographic prospective analysis of 50 patients. J Neurosurg Spine. 2007;6:391-397.
14. Rhee J.M., Riew K.D. Dynamic anterior cervical plates. J Am Acad Orthop Surg. 2007;15:640-646.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree