22 | Cervical Fractures in Diffuse Idiopathic Skeletal Hyperostois |
 | Case Presentation |
History and Physical Examination
The patient, a 73-year-old male, was involved in a motor vehicle accident. He was a restrained front passenger when his car rear-ended another vehicle at ~30 miles per hour. He reported that he had hit his head on the windshield. The patient denied any loss of consciousness and went home ambulating with no apparent neurological compromise. The initial complaints consisted of back pain and headache. Upon awakening the morning after the accident the patient was unable to move his lower extremities. He was subsequently brought to the emergency room. On presentation he had full strength in his bilateral upper extremities and 0/5 motor strength in his bilateral lower extremities. The lower extremity deep tendon reflexes were absent. He had positive Babinski with upgoing toes, no evidence of clonus, and absent rectal tone. The bulbocavernosis reflex was intact.
Radiological Findings
Plain radiographs demonstrated diffuse nonmarginal osteophytes in the cervical spine. The swimmer’s view demonstrated subtle anterior distraction at C7-T1 (Fig. 22–1A). Sagittal and coronal views on a computed tomographic (CT) scan revealed subtle anterior disk space widening at C7-T1 (Fig. 22–lB,C). Fat suppressed T2-weighted sagittal magnetic resonance imaging (MRI) was most revealing, demonstrating high signal intensity at the C7-T1 disk space with concomitant anterior soft tissue edema (Fig. 22–1D).
Diagnosis
Diffuse idiopathic skeletal hyperostosis with distraction-extension injury at C7-T1
 | Background |
Diffuse idiopathic skeletal hyperostosis (DISH) was first described by Forestier and Rotes-Querol in 1951. They identified a disorder characterized by spinal stiffness, osteophytosis, and new bone formation about the thoracic spine. To distinguish this disorder from ankylosing spondylitis (AS) they termed it senile ankylosing hyperostosis. The condition is a systemic bone-forming diathesis with primary spinal and various extraspinal clinical and radiographic findings. Resnick later suggested the term diffuse idiopathic skeletal hyperostosis, which is most often used in the current literature.1 It is often also referred to as Forestier disease. DISH is a common disease, most prevalent in persons over 50 years of age. The reported prevalence of the disease varies slightly. Mata et al in 1998 reported a prevalence of 2.5 to 10% in persons over the age of 70.2 On the other hand, in autopsy series reported by Boachie-Adjei and Bullough the prevalence was 28%. The average age of the subjects was 65 in that study.3 Some authors have suggested that disease starts between the ages of 20 and 40 years but requires several decades to mature to the diagnostic criteria.3
The widely accepted diagnostic criteria was first suggested by Forestier and then supplemented by Resnick. To make the diagnosis of DISH, the radiological studies should satisfy three criteria: (1) there should be flowing ossification along the anterolateral aspect of at least four contiguous vertebrae; (2) the disk height in the involved segments should be preserved, with the absence of significant degenerative changes such as marginal sclerosis in vertebral bodies; and (3) there is an absence of facet-joint ankylosis, sacroiliac erosions, or intra-articular osseous fusion.3 The last two criteria are intended to eliminate AS or degenerative spondylosis as alternative diagnoses. The critical distinguishing feature between AS and DISH is that patients with AS have marginal syndesmophytes, whereas those with DISH have nonmarginal syndesmophytes.
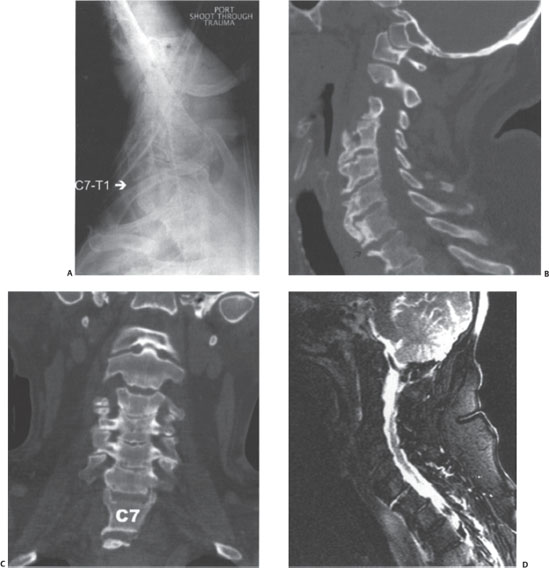
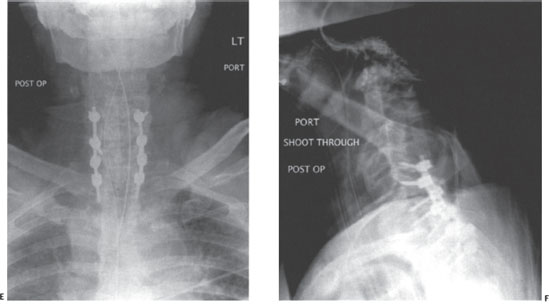
Figure 22–1 (A) Plain radiographs demonstrate diffuse nonmarginal osteophytes in the cervical spine. The swimmer’s view demonstrates subtle anterior distraction at C7-T1. (B,C) Sagittal and coronal views on a computed tomographic scan reveal subtle anterior disk space widening at C7-T1. (D) Fat-suppressed T2-weighted sagittal magnetic resonance imaging demonstrates high signal intensity at the C7-T1 disk space with concomitant anterior soft tissue edema. (E,F) Postoperative anteroposterior and lateral cervical spine radiographs reveal posterior instrumentation from C5 to T2.
It is important to understand the pathophysiology of fracture formation in the cervical spine affected with DISH. The radiographic findings of the disease are most common in the lower segments and less prevalent in the more cephalad levels.4 Ossification and loss of elasticity occur along the anterior paravertebral tissues, such as the anterior longitudinal ligament. Ligamentum flavum hypertrophy, ossification of the posterior longitudinal ligament, and mild cervical kyphosis also occur. All these processes lead to the loss of cervical spine tissue elasticity.5 The long, fused segments increase the lever arm on the normal areas of the cervical spine and predispose those areas to fracture. Contrary to AS where most of the fracture occurs through the disk space, in spines affected with DISH most of the fractures propagate through the vertebral body, though fractures through the disk space are certainly possible. Paley et al, in 1991, presented a series of nine fractures in eight patients with DISH. He described two fracture patterns that occurred in that group. Five fractures occurred through the midportion of the ankylosed segment and involved the vertebral body. Four fractures occurred through the top or bottom of the fused segment and were either disk disruptions or odontoid fractures.6 These patterns are thought to occur for several reasons. The ankylosing bridges in DISH are broader, thicker, and stronger at the level of the disk space. These bridging syndesmophytes attach to the vertebral bodies over a broad area involving proximal and distal thirds. This leaves the middle third of the vertebral body with the least amount of hyperostosis and support and rarefied from the adjacent stress shielding. There is also a relative preservation of the disk space. Finally, most of these patients have significant osteoporosis present in their vertebral bodies. All these factors lead to lowered resistance to fracture in the center of the vertebral body.6
Patients with DISH are at significantly increased risk for cervical fracture. The increased lever arm of the fused segments causes instability and displacement of the cervical spine, even with low-energy minor trauma. Cervical fractures in patients with DISH are often misdiagnosed or present with a delayed diagnosis. There is also a high rate of immediate and delayed neurological deficits. As a result physicians must have a high level of suspicion when dealing with patients with DISH. The patients that present with a history of trauma or neck pain should be carefully evaluated with CT or MRI for occult fractures. Hyperextension injuries with a horizontal shear pattern are more frequent with DISH. Patients may also sustain a flexion-induced compression fracture. In Meyer’s series of 29 patients, 72% of the fractures were the result of a fall and 24% were the result of a motor vehicle accident. Most of the patients sustained an extension injury, almost always at the C6-7 and C7-T1 levels.5 The extension injury in itself is less likely to result in neurological compromise. In an extension injury, the spinal cord is moved away from the fractured vertebra and fractured posterior longitudinal ligament; in addition, with extension injuries the widening of the spinal canal occurs. Flexion injuries, although less common, carry a higher incidence of neurological deficit for the same reasons. Odontoid fractures and atlantoaxial subluxation have been reported in association with DISH but are not considered typical findings.7 However, extension distraction injuries are unstable shear injuries.
 | Authors’ Preferred Method of Surgical Management |
The patient in the clinical vignette was treated with long-segment posterior stabilization. He underwent awake intubation. Neurophysiological monitoring was used, with care to establish baselines prior to positioning. The fracture was stabilized with posterior instrumentation and fusion. The surgical construct extended from three levels above the fracture site to two levels below with segmental fixation (C5 to T2) (Fig. 22–1E,F). Proximal fixation was achieved with lateral mass screws at C5 and pedicle screws at C7. C6 could not accommodate lateral mass screws due to the proximity of the C7 pedicle screws. Distal fixation was achieved with pedicle screws at T1 and T2.
In patients with DISH, it is important to emphasize once again that even minor trauma can cause significant instability and neurological compromise. Unfortunately the diagnosis is often delayed and is not made until a neurological deficit occurs.8 Treatment of the fractures is similar to that of patients with AS. The treatment plan should be based on the type of fracture, the degree of stability, and, most importantly, the presence or absence of neurological compromise. Cervical traction should be avoided in patients with DISH. There is lack of elastic ligamentous structures due to the pathophysiology of the disease. As a result, cervical traction can result in excessive distraction of the injury and catastrophic neurological compromise. For a minor injury with no instability and no neurological deficits, for example, the flexion crimp type of fracture, the patient can probably be treated with a halo vest. For most other fractures, surgical intervention is the only viable option to stabilize the spine and prevent neurological compromise and other complications.
Pearls and Pitfalls
Deciding on whether to use an anterior or posterior approach for fracture fixation depends on the location of the fracture, the location of the fracture fragments in the canal, the presence and severity of neurological symptoms, and the degree of osteoporosis. The most commonly used approach for treating cervical fractures in patients with DISH is posterior. The instrumentation construct should extend sufficiently above and below the injury to be able to counteract the increased deforming forces acting at the fracture site. Because the DISH spine is relatively stiff with autofusion over multiple levels, increasing the length of instrumentation would not significantly sacrifice motion.
The simplest and the oldest technique is posterior cervical wiring. Since its first description by Rogers in 1942,9 several biomechanical studies have shown that simple posterior wiring constructs are stable in flexion but less stable in extension and rotation. Currently, most surgeons prefer the triple wire technique. The triple wire technique has been shown to be mechanically sound and safe and effective if the lamina and spinous processes are intact. Unfortunately, the fixation provided by the laminar wiring is not sufficient for the patients with DISH. The long moment arm created by the fused segments, significant osteopenia, and a frequent involvement of posterior elements in the fracture makes wiring a poor choice for fixation from a biomechanical perspective.
The most optimal fixation alternative for the fractures in DISH is lateral mass and pedicle screw fixation. We generally use lateral mass screws in the subaxial spine and pedicle screws at C7 and T1. The patient should undergo awake intubation and positioning. Neurophysiological monitoring is recommended.
In patients with DISH, the posterior instrumentation for fracture fixation sometimes has to be supplemented by anterior fixation as well. Indications for supplemental anterior fixation include ventral compression from fracture fragments requiring anterior decompression and the presence of significant osteopenia, which would render the posterior-alone screw fixation less than adequate for the task at hand. Given the pathology of the disease already discussed, DISH fractures can often lead to significant spinal instability that necessitates both posterior and anterior fixation for adequate stability. When anterior instrumentation is required, we generally prefer unicortical locking screws due to the presence of osteopenia.



